Bioanalytical Method Transfer for Chromatographic Assays: A Comprehensive Guide to Strategies, Validation, and Troubleshooting
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the successful transfer of bioanalytical chromatographic methods.
Bioanalytical Method Transfer for Chromatographic Assays: A Comprehensive Guide to Strategies, Validation, and Troubleshooting
Abstract
This article provides a comprehensive guide for researchers, scientists, and drug development professionals on the successful transfer of bioanalytical chromatographic methods. It covers the foundational principles and regulatory requirements, explores practical transfer methodologies including comparative testing and covalidation, addresses common troubleshooting and optimization challenges, and details the critical process of validation and cross-validation. The content synthesizes current best practices and regulatory expectations to ensure data integrity, accelerate drug development timelines, and maintain compliance in regulated bioanalysis.
Understanding Bioanalytical Method Transfer: Core Principles and Regulatory Landscape
Defining Analytical Method Transfer (AMT) in a GxP Environment
Analytical Method Transfer (AMT) is a documented process that verifies a validated analytical procedure performs consistently and reliably in a different laboratory, known as the "receiving laboratory," matching the performance of the original "sending laboratory" [1] [2]. In the highly regulated GxP environment, AMT provides the critical evidence required by agencies like the FDA and EMA that an analytical method remains robust and reproducible when executed by different analysts, using different equipment, and in a different location [1]. This process is foundational to ensuring drug product quality and patient safety, especially when manufacturing is transferred to a new facility or when testing is outsourced to partner labs [1] [3].
The Fundamentals of Analytical Method Transfer
The core principle of AMT is to demonstrate equivalency between two laboratories. It is not a re-invention of the method but a confirmation that the existing, validated method works as intended in a new setting [1] [2]. This is distinct from method validation; validation proves a method is suitable for its intended purpose, while transfer proves it can be executed equivalently in a new environment [1].
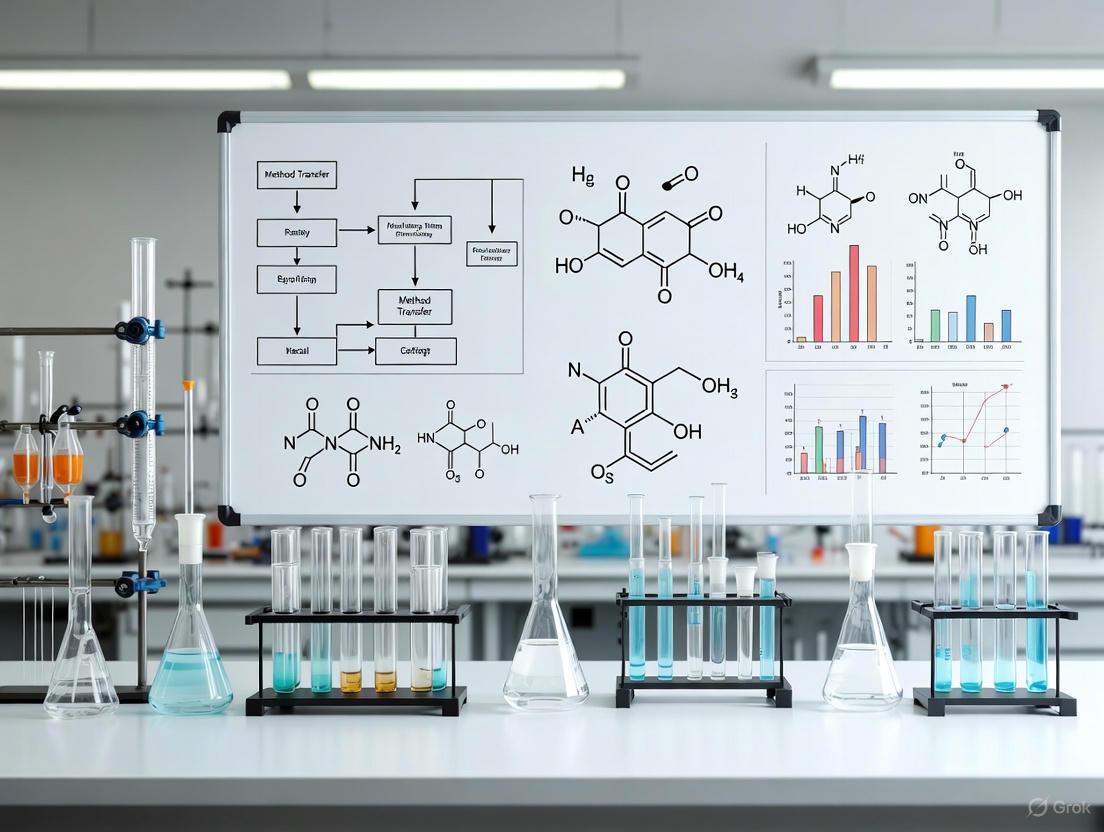
A successful transfer follows a structured, pre-defined path. The diagram below outlines the key stages in the AMT lifecycle, from initial planning to regulatory filing.
Comparison of AMT Approaches
The strategy for transferring a method is not one-size-fits-all. Based on a risk assessment that considers the method's complexity and criticality, different transfer protocols can be applied [1] [4] [5]. The following table compares the four primary types of analytical method transfer.
| Transfer Type | Description | Typical Use Case | Key Advantage | Key Disadvantage |
|---|---|---|---|---|
| Comparative Testing [1] [2] [4] | Both labs analyze identical samples from the same lot(s). Results are statistically compared against pre-defined acceptance criteria. | Most common approach; used for critical methods. | Provides direct, quantitative evidence of equivalency. | Requires significant resources and coordination between labs. |
| Co-Validation [1] [4] [6] | The receiving lab participates in the original method validation studies, providing reproducibility data. | Useful for new or complex methods destined for multi-site use. | Establishes shared ownership and understanding from the start. | Requires early involvement of the receiving lab, which is not always possible. |
| Re-Validation [1] [5] [6] | The receiving lab performs a partial or full validation of the method. | Applied when there are significant differences in equipment or lab environment, or if the originating lab is unavailable. | Does not require parallel testing with the sending lab. | Resource-intensive for the receiving lab; essentially repeats validation work. |
| Transfer Waiver [4] [5] [6] | A formal transfer is omitted based on a justified risk analysis. | Suitable for simple compendial methods (e.g., USP) or when personnel transfer with the method. | Saves time and resources. | Requires robust, documented justification for regulatory acceptance. |
Experimental Protocols for Method Transfer
For a Comparative Testing transfer—the most common protocol—the experiment is executed according to a tightly controlled and pre-approved protocol.
Detailed Methodology: Comparative Testing Protocol
- Sample Selection and Preparation: A single, homogeneous lot of the drug substance or product is typically used to ensure that variability stems from the analytical method itself, not the product [5]. The samples are split and distributed to both the sending and receiving laboratories.
- Parallel Analysis: Both laboratories analyze the samples using the identical, validated analytical procedure. A typical design may include multiple assay parameters (e.g., assay, impurities) and replicate analyses (e.g., n=6) to adequately assess precision [1] [7].
- System Suitability: Both labs must first demonstrate that the analytical system is performing adequately by meeting all system suitability criteria outlined in the method prior to data acquisition [2].
- Data Comparison and Statistical Analysis: The resulting data from both labs are compared using statistical tools. A total error approach is increasingly recommended, which combines accuracy and precision into a single criterion based on an allowable out-of-specification (OOS) rate, overcoming the difficulty of setting separate criteria for precision and bias [7]. Common comparisons include:
- Assay/Potency: Comparison of means using a t-test or equivalence test (e.g., 90% or 95% confidence interval for the difference should fall within ±2.0%) [7].
- Impurity Results: Comparison of means for each specified impurity.
- Content Uniformity: Comparison of means and standard deviations (or variances) [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of an AMT, particularly for chromatographic assays, depends heavily on the quality and consistency of key reagents and materials [1] [2].
| Material/Reagent | Critical Function in AMT | Considerations for Success |
|---|---|---|
| Reference Standard [2] | Serves as the primary benchmark for quantifying the analyte and establishing the calibration curve. | Use the same lot and supplier for both labs to eliminate variability. If not possible, the receiving lab must carefully qualify their standard against the sending lab's [2]. |
| Chromatographic Column [1] | The stationary phase where the critical separation of analytes occurs. | Specify the exact brand, chemistry, dimensions, and particle size. Different column lots can exhibit variations in performance [1]. |
| Critical Reagents (e.g., buffers, ion-pairing agents) [1] | The mobile phase components that directly impact retention time, peak shape, and resolution. | Standardize the grade, supplier, and preparation SOPs. Slight differences in pH or buffer concentration can significantly alter results [1] [2]. |
| Sample Matrix | The biological fluid (e.g., plasma, serum) or placebo formulation in which the analyte is dissolved. | Use the same matrix source (e.g., human plasma from a single lot) or a well-defined synthetic placebo to ensure consistency in sample preparation and analysis [6]. |
| HTH-02-006 | HTH-02-006, MF:C25H29IN6O3, MW:588.4 g/mol | Chemical Reagent |
| KDOAM-25 | KDOAM-25, MF:C15H25N5O2, MW:307.39 g/mol | Chemical Reagent |
Navigating AMT Challenges and the Modern Lifecycle Approach
Despite clear guidelines, laboratories face practical challenges during AMT. Common issues include instrument variability (model, age, calibration), reagent/column variability, differences in analyst technique, and environmental conditions [1] [2]. Mitigation strategies include conducting a thorough risk assessment, ensuring equipment equivalency, standardizing materials, and providing comprehensive, hands-on training for analysts [1] [2].
The landscape of AMT is evolving with the adoption of ICH Q14 and the Analytical Procedure Lifecycle (APL) concept [8]. This paradigm shift moves methods from a static, one-time validation to a dynamic, knowledge-managed system. Key to this approach is defining an Analytical Target Profile (ATP)—a predefined objective for the method's performance—and establishing a Method Operable Design Region (MODR), which is the combination of analytical parameter ranges within which the method performs as expected [8]. Changes within the MODR do not require regulatory re-approval, offering greater flexibility and simplifying post-transfer changes.
By understanding the fundamental principles, choosing the appropriate transfer strategy, meticulously executing experimental protocols, and embracing a modern, lifecycle-oriented mindset, organizations can ensure robust, compliant, and successful analytical method transfers. This ultimately safeguards product quality and accelerates the delivery of therapies to patients [1] [2] [8].
Analytical method transfer is a formally documented process that qualifies a laboratory (the receiving laboratory) to use a validated analytical test procedure that originated in another laboratory (the sending or transferring laboratory) [9]. The primary goal is to ensure that the analytical method continues to perform in its validated state regardless of the change in testing location, thereby guaranteeing the reliability and consistency of data crucial for pharmaceutical development and quality control [10]. This process is fundamental in the lifecycle of a bioanalytical method, ensuring that when methods move—whether from development to quality control, between sites within a company, or to external contract laboratories—data generated remains accurate, precise, and reproducible. A successful transfer hinges on clear communication and a well-defined understanding of the distinct duties assigned to the sending and receiving laboratories [11].
Comparative Roles and Responsibilities
The collaboration between the sending and receiving laboratories is a structured partnership where each party has specific, critical responsibilities. The table below summarizes these key roles for easy reference.
Table 1: Core Responsibilities of Sending vs. Receiving Laboratory
| Area of Responsibility | Sending Laboratory | Receiving Laboratory |
|---|---|---|
| Documentation & Knowledge Transfer | Provides comprehensive method documentation, validation reports, and historical data [11] [5]. | Reviews all provided data for feasibility; identifies gaps or needs for training [11]. |
| Protocol & Report Development | Typically drafts the method transfer protocol, defining objectives and acceptance criteria [11]. | Reviews and approves the protocol; executes the study and drafts the final transfer report [11] [5]. |
| Training & Technical Support | Provides necessary training, which may include on-site sessions for complex methods [11] [12]. | Ensures staff are properly trained and qualified to execute the method [5] [10]. |
| Materials & Equipment | Provides reference standards, test samples, and details on critical reagents [5]. | Verifies availability of required equipment; ensures it is qualified and properly calibrated [5]. |
| Experimental Execution | May analyze pre-determined sample sets for comparative testing [11] [12]. | Perishes the analytical method as per the protocol on a homogeneous lot of material [11] [5]. |
| Communication | Proactively shares tacit knowledge, practical tips, and risk assessments [11]. | Maintains open communication, promptly raising issues or deviations encountered [11] [13]. |
The Sending Laboratory's Role
The sending laboratory acts as the source of truth for the analytical method. Its primary responsibility is the complete and transparent transfer of all technical and scientific knowledge related to the method [11]. This begins with providing the receiving unit with the detailed analytical procedure, the formal validation report, and information on the quality of reference standards and reagents [11] [5]. Crucially, their role extends beyond sharing documents; they must also communicate the "tacit knowledge"—the unwritten practical tips and troubleshooting experience gained during method development and validation [11]. For instance, they might know that a specific column temperature is critical for achieving adequate resolution or that a particular reagent lot can affect sensitivity. This knowledge is often shared through kick-off meetings and, for complex methods, on-site training sessions to ensure the receiving laboratory fully understands the method's nuances [11] [12].
The Receiving Laboratory's Role
The receiving laboratory's role is one of qualification and preparation. Their first task is to conduct a gap analysis, reviewing all information from the sending laboratory to ensure they have the technical capability to perform the method [11]. This involves verifying that all required equipment is available, qualified, and properly calibrated [5]. Furthermore, the receiving lab must ensure its staff are adequately trained on the new method before the formal transfer begins [5] [10]. During the execution phase, the receiving laboratory is responsible for performing the method exactly as written, using the agreed-upon protocol and a single, homogeneous lot of the article to ensure that the comparison focuses on method performance rather than product variability [5]. They must also maintain rigorous documentation of all activities and results, which will form the basis of the final transfer report that concludes the process [11].
The Method Transfer Workflow
The process of analytical method transfer follows a logical sequence from initiation to closure, requiring close collaboration between both laboratories. The diagram below illustrates this workflow and the key responsibilities at each stage.
Diagram 1: Analytical Method Transfer Workflow
The workflow begins with the initiation of the transfer project, often triggered by a need to move testing to a new site. The first critical step is the sharing of documentation and knowledge from the sending unit to the receiving unit [11]. The receiving laboratory then performs a feasibility and gap analysis to assess their readiness and identify any needs for additional training or equipment [11] [12].
A kick-off meeting is highly recommended to align both teams, discuss the method in detail, and plan the transfer [11]. This is often where tacit knowledge is shared. Following this, a detailed transfer protocol is developed and agreed upon, defining the experimental design, acceptance criteria, and responsibilities [11] [5]. With the protocol approved, the execution phase begins, where the receiving laboratory performs the analysis, often in parallel with the sending lab for comparative transfers [12]. The resulting data is then analyzed against the pre-defined acceptance criteria, and a final report is generated to document the success (or failure) of the transfer [11]. The process concludes once the report is approved, and the receiving lab is formally qualified to use the method for its intended GMP purpose.
Experimental Data from a Multi-Platform Bioanalytical Comparison
To ground the principles of method transfer in practical research, a 2024 study provides relevant experimental data. The study directly compared the performance of four different bioanalytical assay platforms—Hybrid LC-MS, SPE-LC-MS, HELISA, and SL-RT-qPCR—for quantifying a single siRNA therapeutic (SIR-2) in a pharmacokinetic study [14]. This inter-platform comparison mirrors the challenges of an inter-laboratory transfer, where demonstrating comparable method performance is key.
Table 2: Quantitative Performance Comparison of Bioanalytical Platforms for siRNA Quantification [14]
| Assay Platform | Key Performance Characteristics | Observed Trend in PK Samples | Potential Cause of Discrepancy |
|---|---|---|---|
| Hybrid LC-MS | High sensitivity, high specificity, potential for metabolite identification | Lower concentrations | High specificity for parent analyte only [14] |
| SPE-LC-MS | Generic reagents, shorter development time, high specificity | Lower concentrations | High specificity for parent analyte only [14] |
| HELISA | High throughput, high sensitivity | Higher concentrations | Lack of specificity; may detect metabolites [14] |
| SL-RT-qPCR | Highest throughput, highest sensitivity | Higher concentrations | Lack of specificity; may detect metabolites [14] |
Experimental Protocol
The methodology for this comparative study was as follows [14]:
- Analyte: A 21-mer lipid-conjugated siRNA therapeutic (SIR-2).
- Sample Matrix: Control Kâ‚‚EDTA plasma.
- Study Design: Samples from a pre-clinical pharmacokinetic study were analyzed by all four developed methods.
- Methodologies:
- Hybrid LC-MS & SPE-LC-MS: Used mobile phases containing 0.1% (v/v) N-Dimethylbutylamine (DMBA) and 0.5% (v/v) hexafluoro-2-propanol (HFIP). An analog siRNA (ISTD-3) was used as an internal standard.
- HELISA: Utilized locked nucleic acid (LNA) capture probes and a ruthenium-labeled anti-digoxigenin antibody for detection.
- SL-RT-qPCR: All reagents were part of commercially available kits, with custom-synthesized primers.
The Scientist's Toolkit: Key Reagents for Bioanalytical Method Transfer
The successful execution of a method transfer relies on a suite of critical reagents and materials. The table below lists essential items and their functions based on the featured study and general practice.
Table 3: Essential Research Reagent Solutions for Bioanalytical Transfers
| Reagent / Material | Function in the Analytical Workflow |
|---|---|
| Locked Nucleic Acid (LNA) Probes | Synthetic nucleic acid analogs used in HELISA and Hybrid LC-MS to specifically capture and enrich the target oligonucleotide, improving sensitivity and specificity [14]. |
| Stem-Loop RT-qPCR Primers | Specialized primers that improve the efficiency of reverse transcription for short RNA targets like siRNA, enabling highly sensitive quantification via PCR [14]. |
| Ion-Pairing Reagents (e.g., DMBA) | Chromatographic additives used in LC-MS mobile phases to facilitate the separation and detection of negatively charged oligonucleotides by interacting with their phosphate backbone [14]. |
| Analog Internal Standard (e.g., ISTD-3) | A structurally similar but non-identical molecule added to samples in LC-MS assays to correct for variability in sample preparation and ionization efficiency [14]. |
| Reference Standards | Highly characterized samples of the analyte used to prepare calibration curves and quality control samples, ensuring the accuracy and traceability of the quantitative results [5]. |
| Critical Biological Reagents | Items such as enzymes (e.g., proteinase K), antibodies, and magnetic beads, which are essential for specific binding, capture, or sample digestion steps in various assay formats [14]. |
| GNE-3511 | GNE-3511, CAS:162112-43-8, MF:C23H26F2N6O, MW:440.5 |
| Pegnivacogin | Pegnivacogin|Factor IXa Inhibitor|Research Use Only |
A successful analytical method transfer is not an isolated event but the result of a meticulously managed collaboration where the sending laboratory acts as the knowledge repository and the receiving laboratory as the qualified implementer. As demonstrated by the comparative bioanalytical data, different methodologies can yield varying results based on their inherent principles, underscoring the need for a controlled and well-understood transfer process. The entire endeavor relies on a foundation of exhaustive documentation, proactive and open communication, and a shared commitment to data integrity. By clearly defining and adhering to their respective roles and responsibilities, laboratories can ensure that analytical methods remain robust, reliable, and in a state of control throughout their lifecycle, thereby safeguarding product quality and patient safety.
In the modern pharmaceutical landscape, Analytical Method Transfer (AMT) has emerged as a critical business process that ensures analytical methods perform consistently and reliably when transferred from one laboratory to another. The objective of a formal method transfer is to guarantee that the receiving laboratory is thoroughly trained, qualified to run the method, and achieves the same results—within experimental error—as the initiating laboratory [15]. This process establishes documented evidence that the analytical method works as effectively in the receiving laboratory as in the originator's facility, qualifying the receiving laboratory to produce Good Manufacturing Practices (GMP) "reportable data" [15].
The business case for AMT extends far beyond mere regulatory compliance. In an era of outsourcing and complex global supply chains, AMT serves as a strategic enabler for operational efficiency, cost reduction, and accelerated drug development. The practice of outsourcing bioanalytical methods from laboratory to laboratory has increasingly become a crucial strategy for successful and efficient delivery of therapies to the market [16]. For generic drug development specifically, technological advancements are profoundly reshaping the development lifecycle, leading to accelerated timelines, significant cost reductions, and enhanced product quality [17]. This article examines the business case for AMT through the lenses of outsourcing efficiency, technological advancement, and strategic drug development optimization.
AMT Methodologies and Transfer Protocols
Core AMT Approaches
The selection of an appropriate AMT strategy depends on the stage of method development, the complexity of the method, and the experience of the personnel involved [15]. There are several well-established approaches to conducting analytical method transfers, each with distinct applications and advantages.
Table 1: Comparative Analysis of AMT Approaches
| Transfer Approach | Description | Typical Application Context | Key Advantages |
|---|---|---|---|
| Comparative Testing | Both laboratories perform a preapproved protocol testing identical samples, with results compared against predetermined acceptance criteria [15] [6]. | Late-stage methods; transfer of complex methods; post-approval situations involving additional manufacturing sites or contract laboratories [15]. | Most common and straightforward approach; provides direct performance comparison; comprehensive assessment. |
| Covalidation | The receiving laboratory participates in the original validation of the method, conducting intermediate precision experiments to generate reproducibility data [15] [6]. | When GMP testing requires multiple laboratories; during initial method validation phases [6]. | Eliminates separate transfer exercise; more efficient; builds method ownership in receiving laboratory. |
| Method Validation/Revalidation | The receiving laboratory repeats some or all of the originating laboratory's validation experiments [15]. | When originating laboratory is unavailable; significant changes in method or instrumentation [6]. | Comprehensive understanding of method performance; demonstrates receiving laboratory proficiency. |
| Transfer Waiver | Formal transfer process is waived based on receiving laboratory's existing experience with similar methods [15] [6]. | Compendial methods (USP, EP); laboratory already testing similar products; transfer of personnel with method expertise [15]. | Saves time and resources; leverages existing capabilities; appropriate for low-risk transfers. |
Experimental Design and Acceptance Criteria
A successful AMT requires a preapproved test plan protocol that details all aspects of the transfer exercise. This document typically takes the form of a Standard Operating Procedure (SOP) specific to the product and method [15]. The protocol must clearly define:
- Scope and Objectives: The specific methods, products, and laboratories involved in the transfer [15].
- Materials and Samples: Representative, homogeneous samples identical for both laboratories, typically pre-GMP materials or "control lots" to avoid triggering out-of-specification (OOS) investigations [15].
- Instrumentation and Parameters: Description of equipment and associated parameters, with consideration given to instrument differences between laboratories [15].
- System Suitability: Established parameters that the method must meet before transfer testing can begin [15].
- Acceptance Criteria: Predetermined statistical criteria for evaluating results, often including means, standard deviations, F-tests, or t-tests [15].
Table 2: Example Experimental Design and Acceptance Criteria for AMT
| Analytical Parameter | Experimental Design | Acceptance Criteria |
|---|---|---|
| Assay and Impurities | Two analysts in receiving lab; one lot in triplicate; compare to original lab data [15]. | 95-105% of original lab results; RSD ≤3% for assay [15]. |
| Content Uniformity | Two analysts in receiving lab; 30 units from one lot; compare to original lab data [15]. | 90-110% of original lab results; RSD ≤6% [15]. |
| Dissolution | Six units from one lot by two analysts in receiving lab; compare to original lab profile [15]. | Similar dissolution profile; difference factor f2 ≥50 [15]. |
The AMT process culminates in a comprehensive transfer report that certifies whether acceptance criteria were met and the receiving laboratory is fully qualified to run the method. This report summarizes all experiments, results, instrumentation used, and any observations made during the transfer [15].
The Outsourcing Imperative: Strategic Business Advantages of AMT
Cost Efficiency and Resource Optimization
The business case for AMT in outsourcing scenarios is compelling from a financial perspective. Partnering with specialized contract manufacturing organizations (CMOs) and contract research organizations (CROs) eliminates the need for substantial capital investments in production equipment and facilities [18]. These significant upfront investments have already been made by the contract organizations, allowing pharmaceutical companies to convert fixed costs into variable costs and maintain financial flexibility [18].
The economic value is particularly pronounced in the generic drug sector, where companies frequently operate with razor-thin profit margins and face intense market pressures [17]. Technological advancements, including those in analytical methodologies, are proving critical for maintaining economic viability in this sector. The substantial cost reductions (up to 40% in drug discovery) and timeline accelerations (up to 70% in development) achievable through advanced approaches represent a vital mechanism for generic companies to sustain operations and capture market share [17].
Focus on Core Competencies and Speed to Market
AMT enables pharmaceutical companies to concentrate internal resources on core competencies such as research and development, innovation, and strategic planning. By outsourcing analytical operations to specialized laboratories, companies can accelerate development timelines and bring products to market faster [18]. This speed-to-market advantage represents a significant competitive edge in an industry where patent protection periods are finite.
The streamlined operations facilitated by effective AMT processes allow medical device and pharmaceutical companies to optimize their supply chain logistics and decrease risks associated with regulatory compliance and quality control [18]. As one contract manufacturer highlights, their comprehensive approach to contract manufacturing allows clients to "concentrate on their core competencies, such as product development, marketing, and sales" without the need to establish and maintain their own manufacturing lines [18].
Access to Specialized Expertise and Technologies
Outsourcing analytical methods through formal transfer protocols provides access to a broader range of skilled professionals and leading-edge technologies that might not be available internally [18]. This access is particularly valuable for complex analytical techniques such as chromatographic-based assays, which require specialized expertise and instrumentation [16] [6].
The field of chromatography continues to evolve rapidly, with recent innovations including:
- AI-powered instrumentation that automates calibration and optimizes system performance [19]
- Micropillar array columns featuring lithographically engineered elements that ensure uniform flow paths [19]
- Microfluidic chip-based columns that replace traditional resin-based columns for exceptional scalability [19]
- Biocompatible/inert columns with passivated hardware to prevent adsorption of metal-sensitive analytes [20]
These technological advancements enable more precise, efficient, and reliable analytical methods, but require significant investment and expertise to implement effectively.
Technological Innovations Enhancing AMT Efficiency
Artificial Intelligence and Automation in Chromatography
The integration of Artificial Intelligence (AI) and Machine Learning (ML) is transforming chromatographic practices, including method transfer processes. AI algorithms are now being employed to automate calibration, optimize system performance, and enhance data analysis [19]. The global AI in pharmaceutical market is valued at $1.94 billion in 2025 and is forecasted to reach approximately $16.49 billion by 2034, demonstrating a robust compound annual growth rate (CAGR) of 27% [17].
Vendors are responding to demands for greater uptime and cost efficiency by incorporating AI directly into instrumentation and workflow design [19]. This technological evolution supports more reliable method transfers by reducing human error and variability between laboratories. Standardized, preconfigured chromatography setups further simplify operation, reducing errors and enabling quicker adoption even by novice users [19].
Advanced Column Technologies
Recent innovations in liquid chromatography columns have significant implications for method transfer success and reliability. The 2025 review of new HPLC columns reveals several trends directly impacting AMT:
Small Molecule Reversed-Phase Columns: New stationary phases with advanced particle bonding and hardware technology enhance peak shapes, improve column efficiency, extend usable pH ranges, and provide improved selectivity [20]. Examples include the Halo 90 Ã… PCS Phenyl-Hexyl column with enhanced peak shape for basic compounds [20], and the SunBridge C18 column with exceptional pH stability (pH 1-12) [20].
Biocompatible/Inert Columns: The trend toward columns with inert hardware continues to address challenges with metal-sensitive analytes [20]. Products like the Halo Inert column integrate passivated hardware to create a metal-free barrier, particularly advantageous for phosphorylated compounds and metal-sensitive analytes [20]. These advancements improve analyte recovery and peak shape, critical factors in successful method transfer.
Specialized Columns for Complex Analyses: New columns designed specifically for challenging separations such as oligonucleotides, proteins, and complex biomolecules are entering the market [20]. The Evosphere C18/AR column, for instance, is suited for oligonucleotide separation without ion-pairing reagents [20].
Cloud Integration and Remote Monitoring
Cloud integration is transforming how chromatographers engage with their instruments, enabling remote monitoring, seamless data sharing, and consistent workflows across global sites [19]. This capability is particularly valuable for AMT activities involving multiple laboratories in different locations. Cloud-based solutions enhance flexibility and collaboration while maintaining data integrity and security.
User-friendly interfaces, including touchscreens, further simplify system control and improve accessibility for personnel of varying expertise levels [19]. This accessibility reduces the training burden during method transfers and facilitates more consistent implementation across sites.
The Regulatory Landscape and Quality Assurance
FDA's Advanced Manufacturing Technologies Designation Program
In December 2024, the FDA finalized its guidance on the Advanced Manufacturing Technologies (AMT) Designation Program, creating a structured pathway for adopting innovative manufacturing technologies [21] [22]. This program aims to facilitate early adoption of AMTs that have the potential to benefit patients by improving manufacturing and supply dependability and optimizing development time of drug and biological products [21].
While distinct from Analytical Method Transfer, the AMT Designation Program shares the overarching goal of enhancing manufacturing and analytical processes in the pharmaceutical industry. The program provides a formal mechanism for FDA recognition of novel technologies that substantially improve manufacturing processes while maintaining or enhancing drug quality [22]. This initiative reflects the regulatory emphasis on technological innovation as a means to address challenges such as drug shortages and quality issues.
Quality Assurance in Analytical Methods
Quality assurance is woven into every aspect of the method transfer process, from initial development through transfer and implementation [6]. Regulatory agencies demand stringent criteria for method validation to ensure the accuracy and reliability of data generated [6]. A successful AMT provides documented evidence that the receiving laboratory can consistently generate reliable results that meet established quality standards.
The foundation of a successful AMT is a properly developed and validated method, with robust robustness studies serving as a development and validation cornerstone [15]. As emphasized in chromatography publications, "the development and validation of robust methods and strict adherence to well documented standard operating procedures is the best way to ensure the ultimate success of the method" [15].
Experimental Protocols and Research Reagent Solutions
Essential Research Reagent Solutions for Chromatographic Assays
Successful method transfer of chromatographic-based assays requires careful attention to critical reagents and materials. The following table outlines key research reagent solutions and their functions in bioanalytical method transfer.
Table 3: Essential Research Reagent Solutions for Chromatographic-Based Assays
| Reagent/Material | Function in Analysis | Critical Considerations |
|---|---|---|
| Reference Standards | Quantification of target analytes; method calibration [6]. | Purity, stability, proper storage; certificate of analysis [15]. |
| Critical Reagents | Antibodies, enzymes, or other specialized reagents used in sample preparation or analysis [6]. | Lot-to-lot consistency; stability documentation; predefined acceptance criteria [6]. |
| Mobile Phase Components | Chromatographic separation of analytes [20]. | pH, buffer concentration, organic modifier; stability and shelf-life [20]. |
| Quality Control Samples | Monitor method performance during validation and transfer [6]. | Representative matrix; low, medium, high concentrations; cover calibration range [6]. |
| Solid-Phase Extraction Cartridges | Sample cleanup and analyte concentration [16]. | Recovery efficiency; selectivity; lot-to-lot reproducibility [16]. |
| Derivatization Reagents | Enhance detection of low-response analytes [23]. | Reaction efficiency; stability; completeness of reaction [23]. |
Workflow Visualization of AMT Process
The following diagram illustrates the comprehensive analytical method transfer process from initiation through completion, including key decision points and documentation requirements.
Diagram 1: Analytical Method Transfer Workflow (32.4KB)
Method Transfer Experimental Protocol
The experimental protocol for a typical comparative testing approach, the most common AMT option, involves method-specific steps but follows a consistent structure [15] [6]:
Protocol Development: Create a preapproved test plan detailing scope, objectives, responsibilities, methods, samples, instrumentation, procedures, and acceptance criteria [15].
Sample Selection and Preparation: Identify representative, homogeneous samples identical for both laboratories, typically using pre-GMP materials or "control lots" to avoid triggering out-of-specification investigations [15].
System Suitability Testing: Both laboratories demonstrate that their chromatographic systems meet predefined criteria before commencing transfer testing [15].
Method Execution: Following a standardized procedure, analysts in both laboratories analyze the predetermined number of sample replicates using identical lots and conditions [15].
Data Collection and Documentation: Both laboratories collect raw data, system suitability results, and any observations during analysis, maintaining complete documentation for all activities [15].
Statistical Comparison: Apply predefined statistical tests (e.g., means comparison, F-tests, t-tests) to evaluate whether results from both laboratories meet acceptance criteria [15].
Report Generation: Document the transfer exercise, including all experiments, results, statistical analyses, instrumentation used, and certification of receiving laboratory qualification [15].
The business case for Analytical Method Transfer rests on its role as a strategic enabler of outsourcing efficiency, technological advancement, and accelerated drug development. In an industry characterized by increasing complexity and pressure to reduce costs while maintaining quality, AMT provides the framework for reliable technology transfer between laboratories. The practice of outsourcing bioanalytical methods from laboratory to laboratory has become a crucial strategy for successful and efficient delivery of therapies to the market [16].
Companies that strategically implement AMT processes with attention to robust method development, clear protocols, and comprehensive documentation position themselves to leverage the benefits of specialized external partners, access cutting-edge technologies, and optimize internal resource allocation. As technological innovations continue to transform chromatographic science and regulatory frameworks evolve to support advanced manufacturing approaches, the strategic importance of effective AMT will only increase.
The integration of AI, advanced column technologies, and cloud-based monitoring systems represents the next frontier in AMT efficiency and reliability. Forward-thinking organizations that embrace these advancements while maintaining rigorous quality standards will achieve sustainable competitive advantages in the rapidly evolving pharmaceutical landscape. Through strategic implementation of AMT principles, companies can balance the competing demands of quality, efficiency, and innovation that define success in modern drug development.
Essential Regulatory Guidelines and Compliance Requirements (FDA, EMA, USP, ICH)
In the realm of pharmaceutical research and development, bioanalytical method validation and transfer are critical processes that ensure the reliability, accuracy, and consistency of data used to support regulatory submissions. Compliance with guidelines from major regulatory bodies—including the U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), United States Pharmacopeia (USP), and International Council for Harmonisation (ICH)—provides a framework for generating credible analytical results that form the basis for regulatory decisions on drug safety and efficacy. These guidelines establish harmonized expectations that are recognized globally, increasing confidence in the accuracy of analytical results and supporting every stage of drug development and manufacturing.
The process of method transfer serves as the critical bridge connecting laboratory-developed methods to the manufacturing environment, ensuring that analytical procedures maintain their integrity and performance characteristics when transitioning between laboratories or to production settings. This guide provides a comprehensive comparison of the regulatory frameworks governing these processes, with a specific focus on chromatographic assays, detailing experimental protocols for compliance and offering visualization of the complex workflows involved in maintaining regulatory standards.
Comparative Analysis of Regulatory Frameworks
The regulatory landscape for bioanalytical methods is governed by harmonized yet distinct guidelines from major international bodies. The following table provides a structured comparison of the essential guidelines applicable to bioanalytical method validation for chromatographic assays.
Table 1: Comprehensive Comparison of Key Regulatory Guidelines for Bioanalytical Methods
| Regulatory Body | Primary Guideline | Status & Date | Geographical Scope | Key Focus Areas | Legal Standing |
|---|---|---|---|---|---|
| ICH | M10: Bioanalytical Method Validation | Finalized (November 2022) [24] | International (Harmonized) | Method validation for chemical & biological drugs; chromatographic & ligand-binding assays; study sample analysis [25] | Scientific guideline, harmonized regulatory expectations |
| FDA | M10 Bioanalytical Method Validation and Study Sample Analysis | Final (November 2022) [24] | United States | Nonclinical and clinical studies supporting regulatory submissions; validation of chromatographic and ligand-binding assays [24] | Guidance document (current thinking, not legally binding) [26] |
| EMA | ICH M10 on bioanalytical method validation | Scientific guideline (adopted ICH M10) | European Union | Chemical and biological drug quantification; validation and study sample analysis [25] | Scientific guideline, part of EU regulatory framework |
| USP | General Chapters & Reference Standards | Continuously updated | United States (Global recognition) | Quality standards; reference materials; analytical procedures; compendial methods [27] | Official compendia (legally recognized under FDCA) |
Inspection and Compliance Verification
Regulatory authorities employ various inspection mechanisms to verify compliance with established guidelines. The EMA coordinates inspections for medicines authorized under the centralized procedure, though it does not conduct inspections itself but rather requests them through national authorities in EU Member States [28]. These inspections can be either "for cause" (triggered by findings of possible non-compliance) or routine (conducted as part of surveillance programs) [28].
The FDA conducts inspections to verify compliance with Current Good Manufacturing Practices (CGMP) and other regulatory requirements, with guidance documents representing the agency's current thinking on regulatory issues [26]. While these guidance documents do not establish legally enforceable responsibilities, they provide the framework for inspection criteria and compliance expectations. For bioanalytical methods, both agencies emphasize the importance of proper method validation, equipment qualification, and data integrity throughout the method lifecycle.
Experimental Protocols for Method Validation and Transfer
Bioanalytical Method Validation Parameters (ICH M10/FDA/EMA)
The ICH M10 guideline provides comprehensive recommendations for validating bioanalytical methods intended for regulatory submissions. The experimental protocols must demonstrate that assays are suitable for their intended purpose through characterization of specific parameters.
Table 2: Required Experiments for Bioanalytical Method Validation per ICH M10
| Validation Parameter | Experimental Protocol | Acceptance Criteria | Chromatographic Assay Specifics |
|---|---|---|---|
| Accuracy and Precision | Analyze minimum 5 replicates at 4 concentrations (LLOQ, L, M, H); 3 separate runs | Within ±15% of nominal value (±20% at LLOQ); Precision ≤15% RSD (≤20% at LLOQ) | Use of stable isotope-labeled internal standards recommended |
| Selectivity/Specificity | Test at least 6 individual matrix sources; evaluate potential interferents | Response <20% of LLOQ for interferents; <5% of internal standard | Chromatographic resolution >1.5 between analyte and closest eluting interference |
| Calibration Curve | Minimum of 6 non-zero standards; 3 separate runs | ±15% deviation from nominal (±20% at LLOQ) | Linear or weighted regression with r² >0.99 typically required |
| Lower Limit of Quantification (LLOQ) | Signal-to-noise ratio ≥5; accuracy and precision within ±20% | Response ≥5 times blank response; precision ≤20% RSD | Confirmed with minimum 5 replicates across multiple runs |
| Stability | Bench-top, freeze-thaw, long-term, processed sample | Within ±15% of nominal value | Evaluate in entire matrix; document storage conditions and duration |
The experimental design must include incurred sample reanalysis (ISR) to demonstrate reproducibility, where a minimum of 10% of study samples (or 50 samples, whichever is greater) should be reanalyzed to confirm method performance with actual study samples [25]. For chromatographic methods specifically, additional parameters such as carryover (assessed by injecting blank samples after high concentration standards) and hematocrit effect (for dried blood spot methods) must be evaluated.
Method Transfer Approaches and Protocols
Method transfer ensures that analytical methods maintain performance characteristics when relocated between laboratories. The transfer process must be documented in a detailed protocol outlining experimental design and acceptance criteria.
Table 3: Comparative Analysis of Method Transfer Approaches
| Transfer Approach | Experimental Protocol | Statistical Analysis | Acceptance Criteria | Applicable Scenarios |
|---|---|---|---|---|
| Comparative Testing | Both labs analyze same set of samples (minimum 3 batches, each in triplicate) [6] | Calculation of mean, % difference, and statistical comparison (e.g., t-test) | Predefined equivalence margins (e.g., ±10% for mean comparison) | Most common approach; suitable for well-established methods |
| Covalidation | Receiving laboratory participates as part of validation team [6] | Intermediate precision experiments to assess reproducibility | Consistency with original validation data | When GMP testing requires multiple laboratories |
| Revalidation | Receiving laboratory repeats specific validation experiments [6] | Comparison with original validation data | Meeting original validation criteria | When originating laboratory unavailable; major method changes |
| Transfer Waiver | Limited verification (e.g., system suitability, key parameters) [6] | Comparison with established method characteristics | Meeting predefined verification criteria | Method already in USP-NF; personnel transfer; minimal changes |
The transfer protocol must clearly define the roles and responsibilities of both sending and receiving laboratories, the number and type of samples to be analyzed, the specific analytical procedures to be followed, and the predefined acceptance criteria that will demonstrate a successful transfer. For chromatographic methods, system suitability tests must be established to ensure the analytical system is operating properly throughout the execution of the transfer protocol.
Visualization of Regulatory Workflows
Bioanalytical Method Validation and Transfer Workflow
The following diagram illustrates the comprehensive workflow for bioanalytical method development, validation, and transfer, highlighting critical decision points and regulatory requirements.
USP Standards Development and Implementation Process
The United States Pharmacopeia plays a critical role in establishing public quality standards. The following diagram outlines the USP standards development process and its integration into regulatory compliance.
Essential Research Reagent Solutions
Successful implementation of bioanalytical methods requires carefully selected reagents and reference materials that meet regulatory standards. The following table details essential research reagent solutions for chromatographic assay development and validation.
Table 4: Essential Research Reagent Solutions for Bioanalytical Chromatography
| Reagent/Material | Function/Purpose | Regulatory Considerations | Example Applications |
|---|---|---|---|
| USP Reference Standards [27] | Highly characterized specimens for qualification and quantification; method validation | Required for compendial methods; accepted by global regulators | System suitability testing; quantitative analysis; identity confirmation |
| Stable Isotope-Labeled Internal Standards | Normalization of extraction efficiency; compensation for matrix effects | Must be well-characterized for purity and stability | LC-MS/MS bioanalysis for small molecules; pharmacokinetic studies |
| Quality Control Materials | Monitor assay performance over time; validate individual runs | Should mimic study samples; prepared in same matrix | Within-run and between-run precision and accuracy assessment |
| Matrix Lots (Plasma, Serum, Blood) | Assessment of selectivity; determination of matrix effects | Minimum 6 individual sources recommended; should cover relevant populations | Selectivity/specificity testing; hemolyzed and lipemic matrix evaluation |
| Critical Reagents (Antibodies, Enzymes) | Essential components for sample processing and analysis | Require characterization and stability data; documentation of source | Ligand-binding assays; immunocapture techniques; enzymatic digestion |
USP Reference Standards are particularly critical as they are "recognized globally" and "accepted by regulators around the world," providing the foundation for analytical rigor in pharmaceutical testing [27]. These standards help reduce the risk of incorrect results that could lead to unnecessary batch failures, product delays, and market withdrawals. For non-compendial methods, internally characterized reference standards must be thoroughly documented with certificates of analysis detailing source, purification methods, and characterization data.
Emerging Trends and Future Directions
The regulatory landscape for bioanalytical methods continues to evolve with several emerging trends impacting compliance requirements. The ICH M10 guideline, while recently finalized, is undergoing implementation with frequently asked questions (FAQ) documents being developed to address practical considerations [25]. Regulatory transparency is increasing, as evidenced by the FDA's recent publication of over 200 complete response letters (CRLs) for drug applications from 2020-2024, providing greater insight into the agency's decision-making process [29].
The USP is transitioning to a new publication model in July 2025, consolidating official publications from 15 to 6 issues per year while maintaining the same content volume [30]. This change aims to provide "expedited publishing timelines, a regular distribution cadence and a single bi-monthly source for official content," potentially impacting how quickly new and revised standards become official.
Regulatory agencies are also increasing collaboration, as demonstrated by the upcoming December 2025 workshop jointly hosted by FDA, USP, and the Association for Accessible Medicines titled "Quality and Regulatory Predictability: Shaping USP Standards" [31]. Such initiatives aim to "increase stakeholder awareness of, and participation in, the USP standards development process, ultimately contributing to product quality and regulatory predictability."
These developments highlight the dynamic nature of the regulatory environment and emphasize the importance of continuous monitoring of guidelines and participation in stakeholder engagement opportunities to maintain compliance in bioanalytical method development, validation, and transfer activities.
In pharmaceutical research and development, the reliability of bioanalytical data is paramount. The journey of an analytical method—from its initial conception in the laboratory to its routine application in quality control—follows a defined pathway known as the method lifecycle. This comprehensive process of method development, validation, and transfer ensures that analytical procedures consistently produce reliable, accurate, and reproducible results, forming the critical backbone for decision-making in drug development [6]. A robust method lifecycle is indispensable for generating data that regulatory bodies such as the FDA and EMA can trust, ultimately supporting submissions for investigational new drugs (INDs), new drug applications (NDAs), and abbreviated new drug applications (aNDAs) [6] [32].
The inherent complexity of modern therapeutics, from small molecules to large biologics like antibody-drug conjugates (ADCs), demands increasingly sophisticated bioanalytical methods [33]. This guide objectively compares the performance of different strategies and technological solutions available for navigating the method lifecycle, providing researchers and drug development professionals with the evidence needed to optimize their analytical workflows.
The Method Development Phase: Building a Robust Foundation
Method development is the crucial first stage where the analytical procedure is designed and optimized. The primary goal is to establish a reliable methodology for quantifying the analyte within a specific biological matrix, outlining everything from sample preparation and separation to detection and data evaluation [32].
Core Challenges and Strategic Comparisons
Researchers face significant challenges during method development. The selection of an appropriate internal standard (IS) is a critical decision point. Stable isotope-labeled versions of the analyte represent the gold standard, as their nearly identical chemical behavior minimizes variability during sample preparation and analysis [32].
Table 1: Comparison of Internal Standard Types for LC-MS/MS Assays
| Internal Standard Type | Key Characteristics | Impact on Assay Performance | Key Limitations |
|---|---|---|---|
| Stable Isotope-Labeled Analyte | Chemically identical, differs by ≥3 amu in mass [32]. | Excellent accuracy and precision; accounts for losses and instrument variation [32]. | Isotopic purity must be high to avoid interference with the analyte [32]. |
| Structural Analogue | Nearly identical structure (e.g., differs by a methyl group) [32]. | Good performance if it undergoes the same extraction processes [32]. | May not perfectly mimic the analyte's behavior, leading to higher variability. |
| No Internal Standard | Practice common in ELISA assays [32]. | Simplifies preparation. | Lower accuracy and precision; data should be considered exploratory or semi-quantitative [32]. |
The sample preparation and analysis stage presents another layer of complexity. For High-Performance Liquid Chromatography (HPLC), common issues include column deterioration, evidenced by peak shape problems and high back pressure, and mobile phase contamination, which leads to rising baselines and noise [32]. For Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS), challenges are often related to optimizing mass spectrometry parameters and managing complex sample matrices [32].
The Analytical Quality by Design (AQbD) Framework
A modern approach to method development involves adopting Analytical Quality by Design (AQbD) principles. Inspired by ICH Q8 and Q9 guidelines, AQbD shifts the focus from a reactive to a proactive methodology [34]. It begins with defining an Analytical Target Profile (ATP), which outlines the method's required performance characteristics, such as the intended measurement, concentration range, and acceptable uncertainty [34]. Through structured experimentation, scientists identify the method's design space—a multidimensional combination of input variables (e.g., mobile phase pH, column temperature, gradient time) that have been demonstrated to provide assurance of quality [34]. Operating within the design space creates a more robust and resilient method, reducing the risk of failure during subsequent validation and transfer.
The Method Validation Phase: Demonstrating Reliability
Following development, a method must undergo rigorous validation to demonstrate its reliability and reproducibility for the intended use [32]. Validation provides evidence that the method meets predefined acceptance criteria for key parameters, giving scientists and regulators confidence in the generated data.
Key Validation Parameters and Acceptance Criteria
Validation involves testing a series of performance parameters using known standards and quality controls within the relevant biological matrix [32]. The following parameters are typically assessed:
- Accuracy and Precision: The closeness of measured values to the true value (accuracy) and the agreement between a series of measurements (precision) [32].
- Selectivity/Specificity: The ability to unequivocally assess the analyte in the presence of other components, such as metabolites or matrix interferences [32].
- Sensitivity: Defined by the Lower Limit of Quantification (LLOQ), the lowest concentration that can be measured with acceptable accuracy and precision [32].
- Stability: The integrity of the analyte under various conditions, including during sample collection, storage, and processing [6].
Navigating Revalidation Challenges Across Species
A significant challenge in drug development is the need to revalidate methods when transitioning from preclinical studies to clinical trials or when adapting to different species. Species-specific metabolic and physiological differences can necessitate modifications to sampling procedures, analytical parameters, or the incorporation of species-specific biomarkers [35]. For instance, circulating target levels for monoclonal antibodies can vary dramatically between animal models and humans, impacting assay specificity [35]. This often requires a partial or full revalidation, extending project timelines and increasing costs [35]. Maintaining a long-term partnership with a single laboratory can mitigate these challenges by ensuring continuity and deep institutional knowledge of the method and compound [35].
The Method Transfer Phase: Ensuring Consistency Across Laboratories
Method transfer is the formal process of moving a fully developed and validated method from one laboratory (the sending unit) to another (the receiving unit), which could be an internal QC lab or an external partner like a Contract Research Organization (CRO) or Contract Development and Manufacturing Organization (CDMO) [6]. The goal is to ensure the method performs consistently and reliably in the new environment, maintaining the integrity and stability of the methods to guarantee consistent product quality throughout its lifecycle [6].
Comparing Method Transfer Approaches
Several standardized approaches exist for method transfer, each with distinct advantages and applications.
Table 2: Comparison of Common Analytical Method Transfer Strategies
| Transfer Approach | Methodology | Typical Use Case | Key Advantage |
|---|---|---|---|
| Comparative Testing | Same samples are tested by both sending and receiving labs; results are compared against predefined acceptance criteria [6]. | Most prevalent approach for standard method transfers [6]. | Provides direct, empirical data comparing lab performance. |
| Covalidation | The receiving lab becomes part of the validation team and conducts specific experiments (e.g., intermediate precision) [6]. | When GMP testing requires multiple labs from the outset [6]. | Integrates transfer into validation, potentially saving time. |
| Revalidation | The receiving laboratory re-performs parts or all of the original validation [6]. | When the originating lab is unavailable or major changes are anticipated [6]. | Provides a standalone validation package for the receiving lab. |
| Transfer Waiver | A formal waiver is granted, forgoing the need for an experimental transfer [6]. | If the receiving lab already uses an identical procedure or the method is specified in a pharmacopoeia like USP-NF [6]. | Eliminates redundant experimental work. |
The Digital Transformation of Method Transfer
Traditional, document-heavy transfer processes are a major industry bottleneck. Relying on PDFs, emails, and manual data re-entry into different Chromatography Data Systems (CDS) is inherently prone to human error, misinterpretation, and mismatched terminology [36] [37]. These manual processes lead to costly deviations, investigations, and project delays. With each delay day for a commercial therapy costing approximately \$500,000 in unrealized sales, the economic incentive for efficiency is immense [36].
A modern, digital approach is solving this old problem. Initiatives like the Pistoia Alliance Methods Hub are pioneering the use of machine-readable, vendor-neutral method exchange formats, such as the Allotrope Data Format (ADF) [36] [37]. This creates a "digital twin" of an analytical method, which can be stored in a central repository and unambiguously executed on different instrument platforms without manual transcription [37]. This digital transformation reduces transfer errors, speeds up tech transfer, and improves overall quality, ultimately accelerating a therapy's time-to-market [36] [37].
Essential Research Reagent Solutions
The success of a bioanalytical method hinges on the quality and appropriateness of its core components. The following table details key reagent solutions and their critical functions.
Table 3: Key Reagents and Materials in Bioanalytical Method Lifecycle
| Reagent / Material | Function / Purpose | Performance Considerations |
|---|---|---|
| Stable Isotope-Labeled Internal Standard | Accounts for variability during sample preparation and instrument analysis in LC-MS/MS [32]. | Ideal standard has ≥3 amu mass difference from analyte and high isotopic purity to avoid interference [32]. |
| Critical Reagents (e.g., antibodies, enzymes) | Enable specific capture and detection of analytes in Ligand Binding Assays (LBAs) [33]. | Development of anti-idiotype or anti-payload antibodies can be resource-intensive and time-consuming [33]. |
| Reference Standards | Provide a known quality and purity benchmark for calibrating analytical measurements [6] [32]. | Essential for establishing calibration curves and defining the analytical method's range [32]. |
| Quality Control (QC) Samples | Monitor the method's performance and ensure ongoing reliability during sample analysis [32]. | Prepared at low, medium, and high concentrations in the relevant biological matrix to assess accuracy and precision [32]. |
Executing a Successful Transfer: Methodologies, Protocols, and Real-World Applications
In the development and application of bioanalytical assays for chromatography research, the reliable transfer of methods from one laboratory to another is a critical yet challenging endeavor. A flawed transfer can lead to discrepant results, delays in product release, and significant regulatory scrutiny [2]. Within the broader thesis on method transfer for bioanalytical assays, this guide objectively compares the four established analytical method transfer protocols. We evaluate their performance through the lens of experimental data, regulatory guidelines, and practical implementation challenges, providing a structured framework to help scientists and drug development professionals select the optimal strategy for their specific context.
The Four Primary Transfer Approaches: A Detailed Comparison
The fundamental principle of any analytical method transfer is to demonstrate that the receiving laboratory can perform a validated analytical procedure and generate results equivalent to those from the originating laboratory [2]. The choice of protocol is a risk-based decision that must be documented in a formal transfer plan [2]. The four primary approaches are detailed below.
Table 1: Comparison of the Four Primary Analytical Method Transfer Approaches
| Transfer Approach | Core Methodology | Typical Acceptance Criteria | Ideal Use Case Scenario | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Comparative Testing [2] [1] | Both originating and receiving labs analyze identical samples; results are statistically compared. | Pre-defined limits for accuracy, precision, and system suitability; results must be statistically equivalent [2] [1]. | Transfer of critical methods for product quality assessment [1]. | Provides direct, quantitative evidence of equivalence; most common and widely accepted approach [2]. | Can be resource-intensive, requiring significant sample analysis and data comparison [2]. |
| Co-validation [2] [1] | Both laboratories collaborate from the outset, jointly performing the method validation studies. | Validation parameters (linearity, accuracy, precision) must meet pre-defined criteria from pooled data [2]. | New or complex methods being established for multi-site use from the beginning [2]. | Fosters shared ownership and deep understanding of the method; efficient for multi-site deployment [1]. | Requires extensive coordination and planning between labs from an early stage [2]. |
| Partial or Full Revalidation [2] [1] | The receiving laboratory performs a full or partial revalidation of the method without direct comparison to the originating lab's results. | Method performance parameters must meet original validation criteria or other justified standards [2]. | When the receiving lab has a high degree of confidence, different equipment, or a unique lab environment [1]. | Demonstrates the receiving lab's standalone capability; useful when originating lab data is unavailable [2]. | Does not provide direct comparability with the originating lab; can be as intensive as the original validation [2]. |
| Waiver of Transfer [2] | A formal transfer is waived under specific, justified circumstances. | Not applicable, but the rationale for the waiver must be thoroughly documented and approved [2]. | Transfer of a simple compendial method (e.g., USP) or between labs with identical equipment and cross-trained staff [2] [1]. | Saves significant time, cost, and resources where risk is demonstrably low [2]. | Requires strong, documented justification and is subject to approval by Quality Assurance [2]. |
Experimental Protocols and Data Presentation
The success of a transfer protocol hinges on a meticulously detailed experimental design and a clear analysis of the resulting data.
Protocol for Comparative Testing
This is the most common protocol and its experimental design serves as a model for rigorous comparison [2].
- Sample Selection: A statistically appropriate number of samples from different batches (e.g., a drug product) are selected. These should cover the specification range, including low, medium, and high concentrations of the analyte[s].
- Experimental Procedure: Both the originating and receiving laboratories analyze the identical set of samples using the same validated method and standardized materials, such as the same lot of reagents and reference standards where possible [2]. The analysis should be performed over multiple days by different analysts to incorporate routine variability.
- Data Analysis: Results from both labs are compared using statistical tests. Common methods include calculating the relative difference between means, using a t-test for accuracy, and a Fisher's test (F-test) for precision [1]. The results must fall within the pre-defined acceptance criteria established in the transfer protocol.
Table 2: Example of Comparative Testing Data for an Assay Method
| Sample ID | Theoretical Concentration (µg/mL) | Originating Lab Result (µg/mL) | Receiving Lab Result (µg/mL) | Relative Difference (%) |
|---|---|---|---|---|
| A (LLOQ) | 1.00 | 1.05 | 0.98 | -6.7 |
| B (Low QC) | 3.00 | 2.95 | 3.10 | +5.1 |
| C (Medium QC) | 50.00 | 49.80 | 50.50 | +1.4 |
| D (High QC) | 80.00 | 81.20 | 79.80 | -1.7 |
| E (ULOQ) | 100.00 | 98.50 | 101.30 | +2.8 |
Acceptance Criteria (Example): The mean results from the receiving laboratory should be within ±10% of the originating laboratory's mean results for each sample level. The precision (RSD) for each lab's results should be ≤5%. All system suitability parameters must be met.
Protocol for a Risk-Based Approach and Strategic Calibration Transfer
Emerging strategies focus on minimizing experimental burden without compromising predictive accuracy. A strategic calibration transfer framework can reduce calibration runs by 30–50% [38].
- Experimental Procedure: This involves iterative subsetting of calibration sets and applying optimal design criteria (D-, A-, and I-optimality). I-optimal design has been identified as the most efficient route to achieve high predictive performance with fewer experimental runs, as it minimizes the average prediction variance [38].
- Data Analysis: The predictive accuracy of models built from these minimal, optimally-selected calibration sets is compared against the full factorial model. Research demonstrates that modest, optimally selected calibration sets combined with Ridge regression and Orthogonal Signal Correction (OSC) preprocessing can deliver prediction errors equivalent to full factorial designs [38]. Ridge regression has been shown to consistently outperform traditional Partial Least Squares (PLS) models, eliminating bias and halving prediction error [38].
A Decision Framework for Selecting a Transfer Approach
The following diagram illustrates the logical decision pathway for selecting the most appropriate transfer method based on key project parameters.
This decision tree should be used in conjunction with a formal risk assessment, which evaluates factors such as method complexity, the analytical technique's familiarity, and the criticality of the data generated [1].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful method transfer relies on the standardization and quality of key materials. The following table details essential reagents and materials, with a focus on LC-MS bioanalysis of small-molecule drugs in physiological matrices [39].
Table 3: Key Research Reagent Solutions for Bioanalytical LC-MS Method Transfer
| Item | Function / Purpose | Critical Considerations for Transfer |
|---|---|---|
| Reference Standards | To identify and quantify the target analyte(s); used for calibration. | Use the same lot number or a certified standard traceable to the original. Purity and stability are paramount [2]. |
| Internal Standards | To correct for variability in sample preparation and instrument response. | Ideally, use a stable isotope-labeled analog of the analyte. Must be co-eluting and show consistent recovery with the analyte [39]. |
| Biological Matrix | The sample material (e.g., plasma, urine) in which the analyte is measured. | Source (species), anticoagulant (for plasma), and storage conditions must be consistent. Matrix effects from different lots should be evaluated [39]. |
| Sample Extraction Sorbents | To clean up the sample and extract the analyte (e.g., SPE cartridges, 96-well plates). | Sorbent chemistry (e.g., C18, mixed-mode), lot-to-lot variability, and retention capacity must be equivalent between labs [2] [39]. |
| LC Chromatography Column | To separate the analyte from matrix interferences. | Specify brand, dimensions, particle size, and pore size. Use columns from the same manufacturer and lot, if possible, to ensure identical selectivity [2]. |
| Mobile Phase Solvents & Buffers | The liquid medium that carries the sample through the LC system. | Use the same grades of solvents, buffer salts, and pH. Minor variations in pH or ionic strength can significantly alter retention times and separation [2]. |
| ONO-7579 | ONO-7579 | Chemical Reagent |
| Nvs-bptf-1 | Nvs-bptf-1, MF:C26H28FN7O3S, MW:537.6 g/mol | Chemical Reagent |
Selecting the appropriate transfer approach is not a one-size-fits-all process but a strategic decision based on method criticality, risk, and operational constraints. Comparative testing remains the gold standard for critical methods, providing robust evidence of equivalence. Co-validation offers a proactive path for multi-site methods, while revalidation asserts a receiving lab's independent capability. The waiver, though efficient, is reserved for low-risk scenarios with strong justification.
The evolving landscape of method transfer emphasizes strategic, risk-based principles. By adopting frameworks that leverage optimal experimental design and advanced data modeling, scientists can achieve regulatory-compliant transfers with greater efficiency and resource conservation. A rigorous, well-documented transfer process, supported by the decision framework and toolkit provided, ultimately transforms a potential operational bottleneck into a strategic advantage, ensuring data integrity and product quality across the global pharmaceutical network.
In the highly regulated landscape of pharmaceutical research and development, ensuring the consistency and reliability of bioanalytical data across different laboratories is paramount. Analytical method transfer is the formal, documented process that qualifies a receiving laboratory to use a method that was developed and validated in another (transferring) laboratory [40]. Among the various approaches available, comparative testing has emerged as the most prevalent and trusted strategy [6] [11]. This guide provides an objective comparison of comparative testing against other method transfer strategies, underpinned by experimental data and framed within the context of modern bioanalytical chromatography research.
The Method Transfer Landscape: A Comparative Analysis
Method transfer is a critical bridge that connects laboratory-developed methods to the manufacturing environment, ensuring consistent product quality throughout its lifecycle [6]. Several standardized approaches exist, each with distinct applications and validation logics. The following diagram illustrates the decision pathway for selecting the appropriate transfer method.
Strategic Approaches to Method Transfer
The choice of transfer strategy is guided by regulatory standards, the method's development stage, and the specific relationship between the involved laboratories [6] [40].
Table 1: Method Transfer Approaches: Principles and Applications
| Transfer Approach | Core Principle | Best-Suited Context | Key Considerations |
|---|---|---|---|
| Comparative Testing | Both laboratories analyze a predefined set of identical samples; results are statistically compared for equivalence [6] [40]. | Well-established, validated methods; laboratories with similar capabilities [40]. | Requires robust statistical analysis and homogeneous samples; most common approach [11]. |
| Covalidation | The receiving laboratory participates as an integral part of the method validation team, conducting experiments to generate reproducibility data [6]. | New methods being developed for multi-site use from the outset [40]. | Demands high collaboration and harmonized protocols; efficient for GMP testing at multiple labs [6]. |
| Revalidation | The receiving laboratory performs a full or partial revalidation of the method as if it were new to their site [40]. | Significant differences in lab conditions/equipment or when the original lab is unavailable [11]. | Most rigorous and resource-intensive; requires a complete validation protocol and report [40]. |
| Transfer Waiver | The formal transfer process is waived based on strong scientific justification and documented risk assessment [6]. | Highly experienced receiving lab using identical conditions; simple, robust methods (e.g., pharmacopoeia) [11]. | Rare and subject to high regulatory scrutiny; requires verification, not full transfer [40]. |
Comparative Testing: The Gold Standard Protocol
Experimental Design and Workflow
The integrity of comparative testing hinges on a meticulously controlled and documented experimental process. The workflow below details the key stages from initial planning to final method qualification.
Key Research Reagent Solutions for Chromatography Assays
The success of a comparative study, particularly for complex bioanalytical assays like those for Antibody-Drug Conjugates (ADCs), relies on high-quality, well-characterized reagents [33].
Table 2: Essential Research Reagents for Bioanalytical Method Transfer
| Reagent / Material | Critical Function | Application in Comparative Testing |
|---|---|---|
| Reference Standards | Serves as the primary benchmark for calibrating instruments and quantifying analytes [33]. | A single, well-characterized lot must be used by both labs to ensure data comparability [40]. |
| Critical Reagents | Includes specific capture/detection antibodies, enzymes, and other binding molecules used in Ligand Binding Assays (LBAs) [33]. | Consistency in lot and sourcing between labs is vital to avoid variability in assay performance [6]. |
| Quality Control (QC) Samples | Prepared samples with known analyte concentrations used to monitor the assay's accuracy and precision during the transfer [6]. | Spiked samples are analyzed by both labs to statistically demonstrate equivalence [11]. |
| Stable-Labeled Internal Standards | Isotopically labeled versions of the analyte used in LC-MS/MS to correct for variability in sample preparation and ionization [33]. | Essential for achieving the high precision required for successful comparative results in mass spectrometry. |
Performance Comparison: Data and Acceptance Criteria
Quantitative Acceptance Criteria for Comparative Testing
The decisive step in comparative testing is the statistical evaluation of the data generated by both laboratories against pre-defined, scientifically justified acceptance criteria [11]. These criteria are typically derived from the method's historical performance and validation data.
Table 3: Typical Acceptance Criteria for Comparative Testing of Chromatography Assays
| Analytical Test | Typical Acceptance Criteria | Basis for Criteria |
|---|---|---|
| Identification | Positive (or negative) identification obtained at the receiving site [11]. | Qualitative match (e.g., retention time, UV spectrum) to the transferring lab's result. |
| Assay / Potency | Absolute difference between the mean results from each site is not more than 2-3% [11]. | Based on the intermediate precision/reproducibility data from the original method validation [40]. |
| Related Substances (Impurities) | Requirement for absolute difference varies with impurity level. For spiked impurities, recovery is typically 80-120% [11]. | More generous criteria for very low levels; tighter criteria for higher, specified impurities to ensure safety. |
| Dissolution | Absolute difference in mean results is NMT 10% at <85% dissolved and NMT 5% at >85% dissolved [11]. | Aligns with global regulatory expectations for demonstrating equivalent product performance. |
Case Study: Comparative Testing in ADC Analysis
Antibody-Drug Conjugates (ADCs) represent a key area where robust method transfer is critical due to their complex, heterogeneous nature [33]. A comparative testing protocol for an ADC would likely involve analyzing for multiple analytes:
- Total Antibody: Typically quantified using a Ligand Binding Assay (LBA) like ELISA. Acceptance criteria would focus on the difference in mean concentration values between labs being within ~5-10% [33].
- Conjugated Payload: Often measured using a hybrid LBA-LC-MS/MS method. The transfer would require demonstrating equivalent extraction efficiency and chromatographic separation, with acceptance criteria for precision (%RSD) and accuracy (%nominal) matching the original validation [33].
- Drug-to-Antibody Ratio (DAR): This critical quality attribute requires sophisticated methods like LC-MS. Comparative testing would assess the ability of the receiving lab to reproduce the DAR distribution profile and average DAR value within a specified range.
Within the rigorous framework of bioanalytical method transfer for chromatography research, comparative testing stands as the gold standard for moving validated methods between laboratories. Its pre-eminence is not accidental but is built on a foundation of direct, statistical evidence of equivalence. While approaches like covalidation are optimal for new methods and waivers are applicable in limited, justified cases, comparative testing offers an unmatched balance of robustness, regulatory acceptance, and practical implementation for the vast majority of established methods. Its rigorous, data-driven protocol ensures that the precision and accuracy of bioanalytical data—the bedrock of drug safety and efficacy—remain uncompromised, regardless of where the analysis is performed.
The development of breakthrough therapies for serious and life-threatening conditions creates a pressing need to accelerate all phases of drug development, including bioanalytical method transfer. Traditional sequential approaches to method validation and transfer can create significant bottlenecks in the critical path to market. Within this context, covalidation has emerged as a powerful parallel processing model that can significantly compress timelines while maintaining scientific rigor and regulatory compliance.
The FDA Safety and Innovation Act of 2012 established the breakthrough therapy designation to expedite the development and approval of innovative drugs, causing biopharmaceutical companies to reassess business practices to identify opportunities for acceleration [41]. Covalidation represents one such opportunity within the bioanalytical workflow, fundamentally reengineering the traditional approach to method qualification. As defined by the United States Pharmacopeia (USP), transfer of analytical procedures (TAP) is "the documented process that qualifies a laboratory (the receiving unit) to use an analytical test procedure that originates in another laboratory (the transferring unit)" [41]. The covalidation model specifically involves simultaneous method validation and receiving site qualification, a departure from the conventional linear process [41] [6].
This guide objectively examines the implementation of covalidation for breakthrough therapies, with specific attention to chromatographic-based bioanalytical assays. We compare performance metrics against traditional approaches, provide detailed experimental protocols, and equip researchers with practical tools for successful deployment in accelerated drug development programs.
Understanding Method Transfer Approaches: A Comparative Analysis
The Global Bioanalytical Consortium defines method transfer as "a specific activity which allows the implementation of an existing analytical method in another laboratory" [42]. Within this framework, several distinct approaches exist, each with characteristic applications, advantages, and limitations.
Comparative Testing
Comparative testing requires both sending and receiving laboratories to analyze a predetermined number of samples from homogeneous lots, with results compared against predefined acceptance criteria [6] [11]. This approach remains the most prevalent transfer model, particularly useful when methods have already been validated at the transferring site [11]. The transfer protocol specifically outlines procedural details, designated samples, and acceptance criteria, typically derived from method validation parameters such as intermediate precision or reproducibility [6].
Covalidation
Covalidation represents a paradigm shift from sequential to parallel processing. As described in USP <1224>, "the transferring unit can involve the receiving unit in an interlaboratory covalidation, including them as a part of the validation team, and thereby obtaining data for the assessment of reproducibility" [41]. This approach does not require the transferring laboratory to complete method validation prior to initiation of activities at the receiving unit [41]. The receiving laboratory participates in reproducibility testing, with criteria defined based on product specifications and the method's purpose [11]. Documentation is streamlined by incorporating covalidation procedures, materials, acceptance criteria, and results directly into validation protocols and reports, eliminating the need for separate transfer documents [41].
Revalidation
Revalidation or partial revalidation involves the receiving laboratory performing complete or partial revalidation of the analytical procedure [41] [11]. This approach is particularly useful when the sending laboratory is not available for comparative testing, or when the original validation was not performed according to ICH requirements [11]. A risk-based approach determines which aspects of the original validation need to be reperformed [6].
Transfer Waiver
Under specific justified circumstances, method transfer requirements may be waived entirely. Valid justification includes the receiving laboratory's existing experience with the procedure, transfer of personnel, or use of compendial procedures already specified in pharmacopeias such as USP-NF [6] [11]. In such cases, a verification process is typically applied instead of a formal transfer [6].
Table 1: Comparative Analysis of Method Transfer Approaches
| Transfer Approach | Key Characteristics | Typical Applications | Advantages | Disadvantages |
|---|---|---|---|---|
| Comparative Testing | Analysis of homogeneous samples by both laboratories; predefined acceptance criteria [11] | Methods already validated at transferring site; most common approach [11] | Well-established methodology; clear acceptance criteria [11] | Sequential process creates timeline pressure; duplicate testing [41] |
| Covalidation | Simultaneous method validation and receiving site qualification; single validation protocol [41] | Breakthrough therapies with accelerated timelines; methods not yet fully validated [41] | 20-30% timeline reduction; enhanced knowledge transfer; streamlined documentation [41] | Requires method readiness; earlier receiving lab involvement; knowledge retention challenges [41] |
| Revalidation | Complete or partial revalidation by receiving laboratory; risk-based parameter selection [6] [11] | Originating laboratory unavailable; original validation insufficient [11] | Independent verification; addresses validation gaps | Resource intensive; potential reproducibility issues |
| Transfer Waiver | Justified exemption from formal transfer; verification instead of transfer [6] [11] | Compendial methods; personnel transfer; minor method changes [11] | Resource efficient; eliminates unnecessary studies | Requires robust scientific justification |
Quantitative Performance Comparison: Covalidation Versus Traditional Approaches
A direct comparison of resource utilization and timeline requirements reveals the significant advantages of the covalidation approach for accelerated development programs. Bristol-Myers Squibb conducted a pilot study comparing traditional comparative testing with covalidation for a drug substance and drug product method transfer involving 50 release testing methods [41].
Table 2: Quantitative Performance Metrics: Traditional vs. Covalidation Approach
| Performance Metric | Traditional Comparative Testing | Covalidation Approach | Improvement |
|---|---|---|---|
| Total Time Investment | 13,330 hours [41] | 10,760 hours [41] | 19.3% reduction |
| Process Timeline | 11 weeks from validation start to transfer completion [41] | 8 weeks from validation start to transfer completion [41] | 27.3% reduction |
| Methods Requiring Comparative Testing | 60% of total methods [41] | 17% of total methods [41] | 71.7% reduction |
| Key Resource Applications | Separate validation, then transfer protocols and reports [41] | Single combined validation/transfer protocol and report [41] | ~40% documentation reduction |
The BMS case study demonstrated that the covalidation approach reduced the proportion of methods requiring comparative testing from 60% to just 17% of the total methods transferred [41]. This reduction was achieved by exclusively applying covalidation to high-performance liquid chromatography (HPLC) and gas chromatography (GC) methods across various manufacturing steps [41]. The primary drivers of these efficiency gains include the parallel rather than sequential execution of activities, elimination of duplicate documentation, and enhanced collaboration between sites [41].
Experimental Protocol: Implementing a Covalidation Study
Successful implementation of covalidation requires meticulous planning, execution, and documentation. The following protocol provides a detailed framework for covalidation of chromatographic-based bioanalytical methods.
Pre-Covalidation Assessment and Planning
- Method Readiness Evaluation: Conduct comprehensive method robustness assessment using quality by design (QbD) principles during method development. For HPLC purity/impurity methods, evaluate multiple variants (binary organic modifier ratio, gradient slope, column temperature) in a model-robust design [41].
- Risk Assessment: Employ a decision-tree approach to assess covalidation suitability. Key decision points include: satisfactory method robustness results from transferring laboratory; receiving laboratory familiarity with the technique; absence of significant instrument or critical material differences between laboratories; and less than 12 months between method validation and commercial manufacture for commercial testing laboratories [41].
- Knowledge Transfer Initiation: Facilitate early introduction of analytical experts from both laboratories. Establish direct communication channels and agree on documentation sharing protocols [11]. Share method description, validation data (even if preliminary), reference standard qualifications, reagent specifications, and any risk assessments performed [11].
Covalidation Protocol Design
- Experimental Design: Include reproducibility testing at the receiving laboratory as part of the validation study [41] [6]. For chromatographic assays, conduct a minimum of two sets of accuracy and precision data using freshly prepared calibration standards over a 2-day period [42].
- Acceptance Criteria Definition: Establish criteria based on method performance and product specifications. For HPLC-related substance methods, typical transfer criteria include absolute difference requirements that vary based on impurity levels, with more generous criteria for low-level impurities and recovery requirements of 80-120% for spiked impurities [11].
- Materials and Instrumentation: Define specific columns, instrumentation, critical reagents, and reference standards. Address any anticipated differences in local practices, such as equipment calibration methodologies or HPLC peak integration techniques [11].
Execution and Troubleshooting
- Parallel Method Qualification: Execute method validation activities simultaneously at both sites according to the unified protocol. For drug substance methods, include assessment of assay, impurities and degradants, residual solvents, counter ions, enantiomeric impurity, and inorganic impurities [41].
- Collaborative Problem-Solving: Establish regular communication cadence to address methodological issues in real-time. This collaborative approach enhances knowledge transfer and method understanding at both sites [41].
- Data Collection and Management: Collect all raw data, chromatograms, and spectra with appropriate metadata. Document any deviations from the protocol or method with justifications [11].
Reporting and Knowledge Management
- Unified Documentation: Prepare a single validation report incorporating data from both laboratories, eliminating the need for separate transfer protocols and reports used in comparative testing [41].
- Knowledge Retention Strategy: Address the risk of knowledge erosion when significant time elapses between covalidation and routine method use. Implement procedures for method experience reinforcement, such as training refreshers or partial reverification immediately before routine use commences [41].
- Continuous Improvement: Document lessons learned regarding method performance, troubleshooting approaches, and transfer methodologies to inform future covalidation activities [41].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of covalidation for chromatographic-based bioanalytical assays requires specific high-quality materials and reagents. The following table details essential research reagent solutions and their critical functions in the covalidation process.
Table 3: Essential Research Reagent Solutions for Chromatography Covalidation
| Reagent/Material | Function in Covalidation | Critical Quality Attributes | Considerations for Transfer |
|---|---|---|---|
| Reference Standards | Quantitative calibration and system suitability testing; method accuracy demonstration [43] | Certified purity and stability; properly documented handling and storage conditions [11] | Use common lot across sites; coordinate qualification activities |
| Chromatography Columns | Stationary phase for separation; critical method performance component [41] | Identical manufacturer, chemistry, lot (or demonstrated equivalence) [11] | Document column specifications and performance characteristics |
| Critical Reagents | Mobile phase components, derivatization agents, internal standards [42] | Consistent quality, purity, and supplier between laboratories [42] | Standardize preparation and qualification procedures |
| Matrix Lots | Biological matrix for bioanalytical methods; demonstration of selectivity [42] | Consistent collection, processing, and storage conditions [42] | Use same source or demonstrate equivalence |
| System Suitability Standards | Verification of instrument performance prior to sample analysis [11] | Stability-indicating properties; representative of method critical parameters [11] | Establish identical preparation and acceptance criteria |
| Quality Control Samples | Assessment of method accuracy, precision, and reproducibility [42] | Cover entire calibration range (LLOQ, low, medium, high, ULOQ) [42] | Use common preparations or demonstrate cross-site comparability |
| SGC-iMLLT | SGC-iMLLT, MF:C22H24N6O, MW:388.5 g/mol | Chemical Reagent | Bench Chemicals |
| Sgc-aak1-1N | Sgc-aak1-1N, MF:C20H22N4O3S, MW:398.5 g/mol | Chemical Reagent | Bench Chemicals |
Risk Management and Decision Framework
The very nature of covalidation carries inherent risks that must be proactively managed through a structured decision framework. Key risks include method readiness uncertainty and earlier-than-normal preparedness requirements at receiving commercial manufacturing sites [41].
Covalidation Risk Assessment
The primary risk in covalidation stems from the fact that "methods subjected to covalidation are yet to be fully validated, therefore, it remains uncertain whether the method can meet all of the validation acceptance criteria" [41]. This risk is particularly elevated when method robustness and ruggedness have not been extensively investigated during development [41]. Additionally, the typical time lag between covalidation and routine execution at manufacturing sites creates knowledge retention challenges and potential timeline pressures if the receiving laboratory is not fully invested in rapid execution [41].
Decision-Tree Implementation
A systematic decision tree should be employed to assess covalidation suitability [41]. Key decision points include:
- Are the method robustness results from the transferring laboratory satisfactory?
- Does the method use a technique with which the receiving lab is familiar?
- Is there a significant instrument or critical material difference between the laboratories?
- Is the time between method validation and commercial manufacture less than 12 months? [41]
Since method robustness represents the most important factor determining covalidation suitability, the transferring laboratory should adopt a systematic approach to robustness evaluation during method development, such as quality by design (QbD) principles with model-robust designs investigating multiple method parameters [41].
Covalidation represents a transformative approach to analytical method transfer that aligns with the accelerated timelines required for breakthrough therapies. The quantitative evidence demonstrates clear advantages over traditional comparative testing, with approximately 20% reduction in both timeline and resource requirements [41]. Beyond these efficiency gains, covalidation fosters enhanced collaboration and knowledge sharing between laboratories, ultimately resulting in more robust methods and stronger receiving laboratory ownership [41].
Successful implementation requires meticulous attention to method readiness assessment, risk management, and structured experimental design. The decision-tree framework provides a systematic approach to evaluating covalidation suitability, while the detailed experimental protocol offers researchers a practical implementation roadmap. When appropriately applied to chromatographic-based bioanalytical methods with demonstrated robustness, covalidation can significantly accelerate drug development timelines without compromising scientific rigor or regulatory standards.
For researchers and drug development professionals working on breakthrough therapies, covalidation offers a powerful strategy to compress critical path activities while maintaining method quality and compliance. As regulatory pathways continue to evolve toward accelerated approval mechanisms, parallel processing approaches like covalidation will become increasingly essential components of the bioanalytical toolkit.
When is Revalidation or a Transfer Waiver Appropriate?
In the highly regulated field of bioanalytical chromatography, ensuring that methods remain reliable when transferred between laboratories, instruments, or personnel is paramount. Revalidation and transfer waivers are critical tools within a broader thesis on method transfer, serving to maintain data integrity while optimizing resource allocation. Determining their appropriate application requires a structured evaluation of method performance and risk.
Defining Revalidation and Transfer Waivers
Revalidation is the process of repeating partial or full validation of an established bioanalytical method to demonstrate that it remains fit for its intended purpose after a change has occurred [44]. This change could be in the instrument, the laboratory site, the sample matrix, or a critical reagent.
A Transfer Waiver is a formal justification, based on objective data, that foregoes a full inter-laboratory method transfer study. It is appropriate when the risk of the transfer failing is deemed negligible, often because the method is robust, the receiving laboratory has extensive experience, or the change is minor [44].
The decision between requiring a full transfer, a partial revalidation, or granting a waiver is guided by a risk-based approach, as illustrated below.
Comparative Decision Framework: Revalidation vs. Transfer Waivers
The choice between initiating revalidation and justifying a waiver depends on a multi-factor assessment. The following table compares key decision-making criteria, with quantitative benchmarks often derived from experimental data on method performance.
Table 1: Decision Matrix for Revalidation and Transfer Waivers
| Criterion | Full or Partial Revalidation is Appropriate | A Transfer Waiver is Appropriate |
|---|---|---|
| Nature of Change | Major change (e.g., new LC-MS/MS instrument model, critical reagent from new vendor, new sample preparation technique) [44]. | Minor or no change (e.g., identical instrument model, same analyst on different days, routine column replacement) [44]. |
| Method Performance History | Method has shown marginal performance in prior transfers or has a limited robustness dataset [44]. | Extensive data demonstrating method robustness and high reproducibility over time and across analysts [44]. |
| Impact on Analytical Parameters | The change is predicted to affect key parameters like accuracy (>±15% bias) or precision (>15% RSD), requiring experimental verification [44]. | The change is not predicted to affect validated method parameters, supported by prior knowledge. |
| System Suitability Test (SST) Power | SST parameters are insufficient to monitor the specific change's impact on data quality. | SSTs are highly specific and can detect any meaningful deviation in critical performance attributes. |
| Regulatory Implications | Change could be viewed as a major amendment in a regulatory filing, requiring documented evidence [44]. | Change is considered a minor variation under relevant regulatory guidance (e.g., FDA, ICH) [44]. |
Experimental Protocols for Justifying a Transfer Waiver
Granting a waiver is not an absence of evidence; it is a decision supported by robust, pre-existing data. The following protocols outline key experiments to generate the necessary justification.
Protocol 1: Establishing Method Robustness for Waiver Justification
A robustness test deliberately introduces small, deliberate variations in method parameters to prove that the method's performance is unaffected.
Experimental Design: Utilize a Design of Experiments (DoE) approach, such as a Plackett-Burman or Full Factorial design, to efficiently test multiple factors simultaneously. Key factors for chromatography include:
- Mobile phase pH (±0.2 units)
- Column temperature (±5°C)
- Flow rate (±10%)
- Gradient time (±5%)
- Different columns (same specification, from different lots or vendors)
Sample Analysis: Analyze quality control (QC) samples at Low, Mid, and High concentrations (e.g., n=3 each) across all experimental conditions.
Data Analysis: Monitor key responses: Accuracy (% Bias), Precision (% RSD), and retention time stability. The method is considered robust if all responses remain within pre-specified acceptance criteria (e.g., ±15% bias and precision for chromatographic assays) across all tested variations [44].
Output: A comprehensive dataset demonstrating that typical, minor inter-laboratory variations do not impact method performance, forming the core of the waiver justification.
Protocol 2: Parallel Testing for Minimal-Impact Changes
For changes deemed very low risk (e.g., transfer between two identical instruments in the same lab), a limited parallel testing protocol can provide final confirmation.
Sample Preparation: Prepare a single set of QC samples (n=6 at each of 3 concentrations).
Instrument Analysis: Split and analyze the QC samples across the original (qualified) system and the new (or receiving lab) system.
Statistical Comparison: Perform a t-test on the quantitative results (e.g., peak area, concentration) from both systems. The acceptance criterion is a p-value > 0.05, indicating no statistically significant difference between the two systems' outputs.
The workflow for this targeted approach is systematic and data-driven.
The Scientist's Toolkit: Essential Research Reagents and Materials
The reliability of revalidation studies and waiver justifications depends on high-quality materials. The following table details key reagents used in advanced bioanalytical fields like Antibody-Drug Conjugate (ADC) analysis, which presents unique challenges due to molecular heterogeneity [44].
Table 2: Key Research Reagent Solutions for Bioanalytical Method Development and Transfer
| Reagent / Material | Function in Bioanalysis | Application Example |
|---|---|---|
| Anti-Idiotype Antibodies | Capture reagents in Ligand Binding Assays (LBAs) that are specific to the unique antigen-binding region of a therapeutic antibody [44]. | Selectively capturing an ADC's antibody component from a complex biological matrix like plasma for quantification. |
| Anti-Payload Antibodies | Capture or detection reagents in LBAs that bind specifically to the cytotoxic drug attached to the antibody [44]. | Measuring the concentration of conjugated antibody in an ADC, distinguishing it from the unconjugated form. |
| Recombinant Antigens | Purified antigens used as capture reagents in sandwich LBAs to bind the therapeutic protein [44]. | Quantifying the "total antibody" concentration of an ADC by capturing all antibody molecules regardless of drug load. |
| Stable Isotope-Labeled (SIL) Internal Standards | Internal standards used in LC-MS/MS assays that are chemically identical to the analyte but heavier, correcting for variability in sample preparation and ionization [44]. | Enabling precise and accurate quantification of small-molecule payloads released from ADCs in pharmacokinetic studies. |
| Critical Assay Controls | Quality Control samples with known analyte concentrations, used to validate assay performance during each run [44]. | Establishing that an assay for a biomarker or pharmacokinetic analyte is performing within accepted parameters of accuracy and precision during revalidation. |
| SR18662 | SR18662, MF:C16H19Cl2N3O4S, MW:420.305 | Chemical Reagent |
| VBIT-3 | VBIT-3, MF:C21H19ClF3N3O3, MW:453.85 | Chemical Reagent |
The appropriateness of revalidation or a transfer waiver is not a binary decision but a spectrum guided by empirical evidence and risk assessment. A robust, well-characterized method with a history of solid performance and minimal complexity is a strong candidate for a waiver upon a low-risk change. In contrast, methods with complex workflows, narrow robustness margins, or those undergoing significant modifications demand comprehensive revalidation. By employing a structured framework, supported by targeted experimental protocols like robustness testing and statistical comparison, scientists and drug development professionals can make defensible decisions that ensure data quality and streamline the method lifecycle.
A robust analytical method transfer is a critical gateway in the drug development lifecycle, ensuring that methods for testing drug safety, quality, and efficacy perform consistently and reliably when moved between laboratories. In the context of bioanalytical assays and chromatography research, a failed transfer can lead to significant delays, costly investigations, and compromised data integrity for regulatory submissions [40]. This guide provides a structured framework for establishing a transfer protocol that is built on clear sample strategies, definitive acceptance criteria, and comprehensive documentation.
Core Approaches to Analytical Method Transfer
Selecting the correct transfer strategy is foundational to success. The choice depends on the method's complexity, the receiving laboratory's experience, and the regulatory context. The following table compares the four primary approaches as defined by industry guidance such as USP <1224> [36] [40].
Table 1: Comparison of Analytical Method Transfer Approaches
| Transfer Approach | Description | Best Suited For | Key Considerations |
|---|---|---|---|
| Comparative Testing | Both transferring and receiving labs analyze the same set of samples; results are statistically compared for equivalence [40]. | Established, validated methods; labs with similar capabilities [40]. | Requires statistically sound acceptance criteria, homogeneous samples, and a detailed protocol [40]. |
| Co-validation | The analytical method is validated simultaneously by both the transferring and receiving laboratories [40]. | New methods or methods being developed specifically for multi-site use [40]. | Demands high collaboration, harmonized protocols, and shared responsibilities from the outset [40]. |
| Revalidation | The receiving laboratory performs a full or partial revalidation of the method [40]. | Significant differences in lab conditions/equipment or after substantial method changes [40]. | Most rigorous and resource-intensive approach; requires a full validation protocol and report [40]. |
| Transfer Waiver | The formal transfer process is waived based on strong scientific justification and data [40]. | Highly experienced receiving lab with identical conditions and equipment; simple, robust methods [40]. | Rarely granted and subject to high regulatory scrutiny; requires extensive prior performance data [40]. |
For most transfers of validated methods, Comparative Testing is the standard approach. The diagram below outlines the high-level workflow and decision points involved in this process.
Method Transfer Process Flow
Establishing Acceptance Criteria and Sample Strategy
Defining objective, statistically justified acceptance criteria before the transfer begins is non-negotiable. These criteria, along with a well-designed sample plan, form the objective basis for judging the transfer's success.
Quantitative Acceptance Criteria
Acceptance criteria should be derived from the method's validation data and aligned with its intended use. The table below summarizes common performance parameters and their typical acceptance criteria for chromatographic and bioanalytical methods [45] [40].
Table 2: Key Performance Parameters and Typical Acceptance Criteria for Method Transfer
| Performance Parameter | Description | Typical Acceptance Criteria (Comparative Testing) |
|---|---|---|
| Accuracy (% Relative Error) | Closeness of the test results to the true value. | ≤ 15-20% difference between labs for potency/conc. [45] |
| Precision (%CV) | The degree of scatter between a series of measurements. | Intra-assay %CV ≤ 15-20% [45] [40] |
| Intermediate Precision | Precision under varied conditions (different analysts, days, equipment). | Inter-assay %CV < 20-30% [45] |
| Linearity & Range | The ability to obtain results proportional to analyte concentration. | Coefficient of determination (R²) > 0.98-0.99 [46] |
| Specificity/Selectivity | Ability to measure the analyte accurately in the presence of interference. | No interference from matrix; negative controls show no activity [45] |
For complex bioassays, statistical assessments using confidence intervals (CIs) are recommended. Equivalence is demonstrated if the 90% CI for parameters like slope and intercept fall entirely within a pre-defined equivalence acceptance criterion (EAC) [46]. For immunoassays like Anti-Drug Antibody (ADA) methods, strategies such as the Two One-Sided T-tests (TOST) are used to statistically prove that the difference in performance (e.g., relative sensitivity) between two labs is less than a "practically significant difference" [47].
Sample Strategy for Comparative Testing
The samples used in comparative testing must be representative and well-characterized.
- Sample Types: A minimum of three lots of drug product or substance (from different batches) is recommended. Testing should include a placebo/blank matrix, and samples spiked with the analyte at known concentrations covering the quantitative range (e.g., Low, Mid, High) [40].
- Replication: Each sample type should be analyzed in triplicate (or as defined by the method) across a minimum of three independent runs by both laboratories [45].
- For Immunoassays: The strategy is more nuanced. For low-risk molecules, use individual donor matrix samples, either unfortified or fortified with a positive control. For high-risk molecules, an in-depth assessment using 100 or more incurred samples from actual patient studies is recommended, with results compared via a 2x2 confusion matrix and a Cohen’s Kappa score to measure agreement [47].
The Experimenter's Toolkit: Documentation and Reagents
A successful transfer is underpinned by meticulous documentation and high-quality, consistent reagents.
The Transfer Protocol and Report: A Documentary Roadmap
The transfer protocol and report are the pillars of regulatory compliance and knowledge transfer.
Table 3: Essential Elements of the Transfer Protocol and Report
| Document Section | Critical Content Requirements |
|---|---|
| Transfer Protocol | |
| Scope & Objectives | Clear statement of the method and purpose of the transfer [40]. |
| Responsibilities | Defined roles for sending and receiving labs (e.g., QA, analysts) [40]. |
| Materials & Methods | Detailed list of reagents, equipment, and the analytical procedure [40]. |
| Experimental Design | Number of batches, replicates, runs, analysts, and a description of samples [40]. |
| Acceptance Criteria | Pre-defined, statistically justified criteria for all relevant parameters [40]. |
| Transfer Report | |
| Executive Summary | Conclusion on the success/failure of the transfer [40]. |
| Results & Data Analysis | All raw data and statistical comparison against acceptance criteria [40]. |
| Deviation Investigation | Documentation and justification for any deviations from the protocol [40]. |
| Final Approval | Formal sign-off by responsible personnel and Quality Assurance [40]. |
| VinSpinIn | VinSpinIn|SPIN1 Chemical Probe|For Research |
| Vonoprazan Fumarate | Vonoprazan Fumarate |
Research Reagent Solutions
Consistency of critical reagents is paramount, especially for cell-based bioassays and immunoassays.
Table 4: Essential Research Reagents for Bioassay and Chromatography Method Transfer
| Reagent / Material | Critical Function in Transfer | Best Practices for Transfer |
|---|---|---|
| Reference Standard (RS) | The benchmark for calculating potency and accuracy [45]. | Use a single, well-characterized lot for the entire transfer. Prepare single-use aliquots to ensure consistency [45]. |
| Cell Line | The living component of cell-based bioassays; source of variability [45]. | Use a consistent Master or Working Cell Bank. Use cells within a defined passage range to ensure performance [45]. |
| Critical Assay Reagents | Includes capture/detection antibodies, enzymes, and other key components [47]. | Use the same vendor and lot numbers at both labs. If a new lot is required, perform a formal cross-testing and bridging study [47]. |
| Negative Control Matrix | Establishes the baseline signal and is critical for cut-point determination [47]. | Ideally, use the same pooled lot of control matrix (e.g., normal human serum) at both labs. If not, demonstrate equivalence over multiple runs [47]. |
Implementing a Phase-Appropriate and Digital-Ready Protocol
The stringency of the transfer protocol should be aligned with the stage of drug development.
- Phase-Appropriate Strategy: For early-phase (Phase 1) trials, a "fit-for-purpose" assay demonstrating accuracy, reproducibility, and biological relevance is often sufficient. For late-phase (Phase 3) and commercial release, a fully validated assay meeting strict FDA/EMA/ICH guidelines and performed under GMP/GLP standards is required [45].
- The Digital Future of Method Transfer: A significant challenge in chromatography transfer is the manual transcription of methods from documents (e.g., PDF) into vendor-specific Chromatography Data System (CDS) software, which introduces errors and delays. Embracing digital, machine-readable methods using standards like the Allotrope Data Format (ADF) can automate exchange, reduce errors, and accelerate transfer timelines [36].
Adopting this structured approach to transfer protocol design, with its focus on clear samples, justified criteria, and thorough documentation, is essential for ensuring data integrity, regulatory compliance, and the efficient progression of life-saving therapeutics through the development pipeline.
Overcoming Common Hurdles: Practical Troubleshooting and LC-MS/MS Optimization
Identifying and Resolving Frequent Chromatographic Pitfalls
In the field of bioanalysis, the successful transfer of chromatographic methods is a critical, yet often challenging, step in the drug development process. It requires moving a validated method from a sending laboratory (e.g., a sponsor company) to a receiving laboratory (e.g., a Contract Research Organization) while ensuring the method's performance remains accurate, precise, and robust [3] [48]. Failures during this transfer can lead to significant project delays, increased costs, and compromised data integrity for regulatory filings. This guide objectively compares the performance of conventional stainless-steel column hardware against modern bioinert alternatives and provides detailed protocols for troubleshooting common chromatographic pitfalls encountered during method transfer and routine bioanalytical research.
Common Pitfalls in Chromatographic Methods
Peak Shape Anomalies
Abnormal peak shapes are a frequent indicator of underlying method or hardware issues.
- Peak Tailing: Often caused by secondary interactions of analytes with active sites on the chromatographic hardware or stationary phase. Basic compounds, in particular, can interact with residual silanol groups in the silica matrix [49].
- Peak Fronting: This can result from column overload (injecting too much sample), a channeled column bed, or the sample being dissolved in a solvent stronger than the mobile phase [50] [49].
- Split Peaks: Typically suggest a blockage at the column inlet frit or contamination of the column or guard column [50].
Baseline Irregularities
A stable baseline is fundamental for reliable integration and quantification.
- Baseline Noise: Random fluctuations can be caused by a leaking system, air bubbles, a contaminated detector cell, or a failing detector lamp [50].
- Baseline Drift: A gradual upward or downward trend is often linked to poor temperature control, a changing mobile phase composition (especially in gradient methods), insufficient column equilibration, or a contaminated detector flow cell [50].
Retention Time Instability
Inconsistent retention times undermine peak identification and method reliability.
- Causes: Fluctuations can be attributed to inadequate control of column temperature, incorrect mobile phase composition, poor equilibration after a gradient, changes in flow rate, or a leak in the system [50].
Pressure Abnormalities
System pressure is a key diagnostic parameter.
- High Pressure: Most commonly caused by a blockage, either in the system tubing (e.g., injector) or, more frequently, at the inlet frit of the column. It can also result from mobile phase precipitation or using a flow rate that is too high [50] [49].
- Low Pressure: Usually indicative of a leak in the system or a low flow rate from the pump [50].
- Pressure Fluctuations: Often a sign of air in the system, a failing pump seal, or a faulty check valve [50].
Experimental Comparison: Bioinert vs. Conventional Column Hardware
A significant source of peak shape issues and analyte loss for specific compound classes is nonspecific adsorption to metal surfaces in conventional stainless-steel HPLC systems and columns. The following experiment compares the performance of bioinert column hardware against traditional stainless-steel hardware.
Experimental Protocol
- Objective: To evaluate the impact of column hardware material on the chromatographic performance of analytes prone to metal interaction.
- Materials:
- Analytes: A phosphorothioated RNA oligonucleotide and a representative phospholipid standard.
- Columns: Three columns with identical dimensions (e.g., 2.1 x 150 mm) and stationary phase (e.g., C18), but different hardware:
- Standard stainless steel (control).
- PEEK-lined stainless steel.
- Bioinert-coated stainless steel.
- Instrumentation: A UHPLC system coupled to a mass spectrometer. For optimal results, a bioinert UHPLC system is recommended to eliminate metal interactions throughout the entire flow path.
- Chromatographic Conditions:
- Mode: Ion-Pair Reversed-Phase Chromatography (IP-RPLC) for oligonucleotides; Reversed-Phase for lipids.
- Mobile Phase: For oligonucleotides: 100 mM Hexafluoro-2-propanol (HFIP) with 16.3 mM Triethylamine (TEA) in water (A) and methanol (B). For lipids: Acetonitrile/water with ammonium acetate or formate.
- Gradient: Optimized for the separation of the target analytes.
- Detection: UV (260 nm for oligonucleotides) and MS.
- Methodology: The same sample was injected onto each column. Key performance parameters—peak area, peak height, and peak symmetry (tailing factor)—were measured and compared. The experiment was replicated (n=6) to ensure statistical significance [51].
Results and Data Comparison
The quantitative data below summarizes the performance comparison for the oligonucleotide analysis.
Table 1: Performance Comparison for Oligonucleotide Analysis (IP-RPLC Mode)
| Performance Parameter | Stainless Steel Column | PEEK-Lined Column | Bioinert-Coated Column |
|---|---|---|---|
| Peak Area (mAU * min) | 105.2 ± 8.5 | 185.7 ± 6.1 | 215.4 ± 5.3 |
| Peak Height (mAU) | 12.5 ± 1.1 | 21.8 ± 0.9 | 25.1 ± 0.7 |
| Tailing Factor | 2.5 ± 0.3 | 1.5 ± 0.1 | 1.1 ± 0.1 |
| Conditioning Injections Required | ~20 | ~14 | ~8 |
Data presented as mean ± standard deviation (n=6). Adapted from application notes and experimental data in [51].
The results demonstrate a clear advantage of bioinert hardware. The bioinert-coated column showed a recovery of the oligonucleotide that was more than double that of the stainless-steel column, based on peak area and height. Furthermore, peak shape was dramatically improved, with a tailing factor approaching the ideal value of 1.0. Similar trends were observed for phospholipids and other coordinating compounds, confirming that bioinert hardware is essential for achieving high recovery and reliable quantification for these analyte classes [51].
Detailed Experimental Protocols
Protocol for Assessing and Troubleshooting Column Efficiency (Plate Number)
A sudden drop in column efficiency, measured as the theoretical plate number (N), is a common problem during method transfer.
- Objective: To diagnose the cause of reduced column efficiency.
- Materials: Method-specific mobile phases, reference standard, and the chromatographic column.
- Methodology:
- Measure Current Efficiency: Inject the reference standard and calculate the plate number for a well-retained peak using the formula from the chromatographic data system, often based on peak width at half height: ( N = 5.54 \times (tR / w{1/2})^2 ), where ( tR ) is the retention time and ( w{1/2} ) is the peak width at half height [52].
- Compare to Expected Value: Compare the measured N value to the value obtained during method validation or the column certificate of analysis.
- Diagnostic Steps:
- Check Extra-column Volume: Use short, narrow-bore connecting capillaries (e.g., 0.13 mm i.d. for UHPLC). The extra-column volume should not exceed 1/10 of the smallest peak volume [49].
- Check Detector Settings: Ensure the detector time constant is less than 1/4 of the narrowest peak's width at half-height [49].
- Evaluate Flow Rate: Efficiency is dependent on mobile phase flow rate/linear velocity. Consult the column's van Deemter curve to ensure the method operates near the optimum flow rate [52].
- Test for Column Degradation: If other factors are ruled out, the column may be degraded or have a void. Replacing the column is often the final step [49].
Protocol for a Risk-Based Bioanalytical Method Transfer
A robust transfer strategy is required to ensure data equivalence between the sending and receiving laboratories.
- Objective: To formally demonstrate that the receiving laboratory can successfully execute the analytical method.
- Materials: Pre-qualified and calibrated LC-MS/MS system, control matrix, stock solutions of analytes and internal standards.
- Methodology:
- Experimental Design: The receiving laboratory analyzes a minimum of three validation batches over multiple days. Each batch includes a calibration curve and QC samples at multiple concentration levels (e.g., low, mid, high) prepared in the appropriate biological matrix [48].
- Statistical Analysis: The accuracy (relative error) and precision (coefficient of variation) of the QC samples are calculated. A risk-based approach that considers the total error (sum of systematic and random errors) is superior to evaluating trueness and precision separately [48].
- Acceptance Criteria: A common standard, per FDA guidance, is that the mean accuracy and precision for the QC samples should be within ±15% of the nominal concentration (±20% at the LLOQ). At least 67% of all QC samples and 50% at each concentration level must meet these criteria [48].
- Documentation: All procedures, raw data, and results are documented in a formal method transfer report.
Visualization of Workflows
Systematic Troubleshooting Pathway
The following diagram outlines a logical pathway for diagnosing common chromatographic issues.
Method Transfer and Qualification Process
This workflow illustrates the key stages in a formal bioanalytical method transfer.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for Robust Bioanalytical Methods
| Item | Function & Rationale |
|---|---|
| High-Purity Silica (Type B) | Minimizes peak tailing for basic compounds by reducing metal impurities and acidic silanol sites [49]. |
| Bioinert Chromatography Column | Coated or PEEK-lined hardware prevents analyte adsorption, improving recovery for sensitive molecules like oligonucleotides and lipids [51]. |
| HPLC-Grade Water & Solvents | Preures baseline noise and ghost peaks caused by UV-absorbing contaminants or particulate matter [50] [49]. |
| Volatile Buffers & Additives | Essential for LC-MS compatibility. Examples: Ammonium acetate/formate, Trifluoroacetic Acid (TFA), Formic Acid [51]. |
| Guard Column | Protects the expensive analytical column from particulate matter and irreversible contamination, extending its lifetime [50] [49]. |
| Phosphoric Acid / EDTA Solutions | Used for periodic passivation of stainless-steel systems to temporarily reduce metal activity, though not a permanent solution [51]. |
| Xmu-MP-3 | Xmu-MP-3, MF:C27H27F3N8O, MW:536.6 g/mol |
| YLT-11 | YLT-11|PLK4 Inhibitor|For Research Use |
The identification and resolution of chromatographic pitfalls are fundamental to the success of bioanalytical method transfers and the generation of reliable data. This guide has highlighted that many common issues, such as peak tailing and low recovery, can be systematically diagnosed and addressed. The experimental data demonstrates that for specific, sensitive analyte classes, the choice of hardware is not merely a preference but a critical methodological factor. Adopting a structured, risk-based approach for method transfer, complemented by a deep understanding of chromatographic principles and modern tools like bioinert instrumentation, provides a robust framework for ensuring data quality, regulatory compliance, and efficiency in drug development.
Mitigating Method Transfer Risks Through Robustness Testing
In the pharmaceutical development landscape, the transfer of bioanalytical methods from one laboratory to another has become a standard business practice for efficient drug delivery [3]. However, this process carries significant risks, including transfer failure, data irreproducibility, and costly operational delays. Robustness testing—defined as "a measure of [a method's] capacity to remain unaffected by small, but deliberate variations in procedural parameters"—serves as a crucial predictive tool to de-risk this process [53] [54]. When strategically integrated into method development and validation protocols, robustness assessment provides an indication of a method's reliability during normal use and enables the establishment of meaningful system suitability criteria [55]. This guide examines how systematic robustness evaluation creates a more predictable and successful method transfer pathway, objectively comparing different methodological approaches and their outcomes in securing chromatographic assay performance across laboratories.
Theoretical Foundation: Linking Robustness Testing to Transfer Success
The Method Transfer Landscape
Method transfer is formally defined as "a specific activity which allows the implementation of an existing analytical method in another laboratory" [42]. The Global Bioanalytical Consortium (GBC) distinguishes between internal transfers (within the same organization with shared systems) and external transfers (to different organizations), with each requiring different validation approaches [42]. Internal transfers may require only limited comparative testing, while external transfers typically necessitate nearly full validation [42]. The principle goal is to demonstrate that the method performs appropriately in the receiving laboratory, a outcome that can be significantly predicted through pre-transfer robustness assessment.
Robustness Versus Ruggedness
While often used interchangeably, robustness and ruggedness represent distinct validation parameters [54]:
- Robustness evaluates a method's stability against deliberate variations in method parameters explicitly defined in the procedure (e.g., mobile phase pH, column temperature, flow rate) [54]. These are considered internal factors.
- Ruggedness (increasingly referred to as intermediate precision) assesses reproducibility under external conditions such as different analysts, instruments, laboratories, or days [54].
This distinction is crucial for method transfer planning, as robustness testing specifically identifies the methodological "levers" that must be controlled to ensure transfer success, while ruggedness testing evaluates the impact of environmental factors expected during transfer.
Experimental Design for Robustness Assessment
Key Factors for Chromatographic Methods
Robustness testing in chromatographic methods involves deliberately varying operational parameters within small but realistic ranges to identify critical factors [53] [54]. The table below summarizes common factors to investigate in robustness studies for chromatographic methods, along with typical variation ranges.
Table 1: Key Factors and Typical Variations in Chromatographic Robustness Testing
| Factor Category | Specific Factors | Typical Variations | Impact Assessment |
|---|---|---|---|
| Mobile Phase | pH | ±0.1-0.2 units | Retention time, selectivity |
| Buffer concentration | ±5-10% | Retention time, peak shape | |
| Organic modifier ratio | ±2-5% absolute | Retention time, resolution | |
| Chromatographic Hardware | Column lot/brand | Different suppliers | Retention, selectivity, peak shape |
| Temperature | ±2-5°C | Retention time, efficiency | |
| Flow Conditions | Flow rate | ±0.05-0.1 mL/min | Retention time, pressure |
| Gradient slope/time | ±1-2% | Retention time, resolution | |
| Detection | Wavelength | ±2-5 nm (UV) | Peak area, sensitivity |
Experimental Design Approaches
Univariate approaches (changing one factor at a time) have traditionally been used but are inefficient and often fail to detect factor interactions [54]. Multivariate screening designs offer a more sophisticated and efficient alternative:
- Full factorial designs: Examine all possible combinations of factors at two levels (high/low). Suitable for ≤5 factors (e.g., 2^5 = 32 runs) [54].
- Fractional factorial designs: Examine a carefully chosen subset of factor combinations. Ideal for 5-10 factors, significantly reducing experimental burden while maintaining ability to detect main effects [54].
- Plackett-Burman designs: Highly economical designs in multiples of four runs that efficiently screen many factors when only main effects are of interest [54].
The experimental workflow for a properly designed robustness study follows a logical progression from planning through execution to data-driven decision making, as illustrated below:
Response Measurement and Data Analysis
In robustness testing, both quantitative responses (peak area, retention time, resolution) and system suitability parameters (tailing factor, plate count) should be monitored [53]. The effect of each factor is calculated using the formula:
Effect(X) = [ΣY(+)/N] - [ΣY(-)/N]
Where ΣY(+) and ΣY(-) represent the sums of responses when factor X is at high or low levels respectively, and N is the number of experiments at each level [53]. Statistical analysis (e.g., regression modeling, ANOVA) then identifies statistically significant effects that could impair method performance during transfer.
Comparative Assessment of Robustness Testing Outcomes
Impact on Method Transfer Success Rates
Implementing comprehensive robustness testing prior to method transfer significantly de-risks the process. The table below compares transfer outcomes for methods with and without pre-transfer robustness assessment, synthesized from industry data.
Table 2: Comparative Transfer Outcomes With and Without Robustness Assessment
| Performance Metric | Without Robustness Testing | With Robustness Testing | Impact |
|---|---|---|---|
| First-time transfer success rate | 45-60% | 85-95% | Reduced rework |
| Inter-laboratory precision (RSD) | >10-15% | <5-8% | Improved data quality |
| Method modification rate post-transfer | 30-40% | 5-15% | Reduced protocol amendments |
| Time to complete transfer | 4-8 weeks | 2-4 weeks | Accelerated timelines |
| Documented system suitability criteria | Often arbitrary | Experimentally established | Scientifically justified |
Platform-Specific Considerations
The application of robustness testing varies across analytical platforms, with distinct considerations for different detection techniques:
- Liquid Chromatography-Mass Spectrometry (LC-MS): Requires special attention to matrix effects and ion source parameters, which are critical validation parameters often overlooked [55]. Signal drift over time must be monitored and corrected using quality control samples [56].
- Ligand Binding Assays (e.g., ELISA): More complex to transfer due to critical reagents, with lot-to-lot variability of reagents and consumables representing significant risk factors [42].
- Gas Chromatography-Mass Spectrometry (GC-MS): Requires monitoring of long-term instrumental drift, with recent studies showing Random Forest algorithms effectively correct data over 155-day periods [56].
Implementation Framework: From Robustness Testing to Successful Transfer
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful robustness testing and method transfer requires carefully selected reagents and materials. The table below details key solutions and their functions in ensuring robust method performance.
Table 3: Essential Research Reagent Solutions for Robustness Assessment
| Reagent/Material | Function in Robustness Testing | Application Notes |
|---|---|---|
| Reference Standards | Quantification and system suitability | Use well-characterized, high-purity materials |
| Quality Control Samples | Monitoring analytical performance | Prepare at multiple concentrations (LOW, MID, HIGH) |
| Different Column Lots/Brands | Assessing chromatographic selectivity | Test 2-3 different lots from same and different suppliers |
| Multiple Buffer Lots | Evaluating mobile phase robustness | Prepare from different reagent lots and sources |
| Matrix Lots | Assessing specificity and matrix effects | Test from at least 6 different sources [55] |
| Internal Standards | Monitoring injection and extraction variance | Use stable isotope-labeled when possible |
| Carbodine | Entecavir Intermediate|4-amino-1-[(2R,3S,4S)-2,3-dihydroxy-4-(hydroxymethyl)cyclopentyl]pyrimidin-2-one | High-purity 4-amino-1-[(2R,3S,4S)-2,3-dihydroxy-4-(hydroxymethyl)cyclopentyl]pyrimidin-2-one, a key Entecavir intermediate. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| ABT-255 free base | ABT-255 free base, CAS:186293-38-9, MF:C21H24FN3O3, MW:385.4 g/mol | Chemical Reagent |
Systematic Protocol for Risk-Based Robustness Assessment
A strategic approach to robustness testing focuses resources on the highest-risk method parameters:
- Parameter Prioritization: Identify factors most likely to vary during transfer based on method knowledge and receiving laboratory capabilities.
- Experimental Design Selection: Choose appropriate design (full factorial, fractional factorial, Plackett-Burman) based on number of factors and resources.
- Response Monitoring: Track both quantitative (accuracy, precision) and system suitability (resolution, tailing) responses.
- Statistical Analysis: Calculate factor effects and identify statistically and practically significant parameters.
- System Suitability Establishment: Define scientifically-justified acceptance criteria for critical method parameters [53].
- Control Strategy Documentation: Specify which parameters must be tightly controlled and allowable ranges for successful method application.
The relationship between robustness testing activities and their impact on transfer risk reduction follows a clear logical pathway, as shown below:
Strategic implementation of robustness testing during method development provides a powerful mechanism to de-risk the method transfer process. By systematically identifying critical method parameters and their acceptable operating ranges, robustness assessment enables the establishment of scientifically-justified system suitability criteria and creates a predictive framework for transfer success. The comparative data presented demonstrates that investing in comprehensive robustness testing significantly improves first-time transfer success rates, reduces inter-laboratory variability, and accelerates method implementation timelines. As regulatory expectations continue to evolve, proactively addressing robustness will become increasingly essential for efficient bioanalytical method life cycle management in pharmaceutical development.
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) is the reference technique for quantitative bioanalysis in drug development, pharmacokinetics, and biomarker research due to its exceptional specificity, dynamic range, and ability to analyze multiple analytes simultaneously [57]. However, achieving optimal sensitivity remains a persistent challenge, particularly for method transfer in bioanalytical assays where consistency across laboratories is paramount. Sensitivity in LC-MS/MS is fundamentally governed by the signal-to-noise ratio (SNR), a crucial metric that compares the level of a desired signal to the level of background noise [58]. A high SNR indicates a clear, detectable signal, while a low SNR means the signal is obscured by noise, compromising detection and quantification accuracy [58].
The process of transferring methods between laboratories introduces additional variables that can adversely affect sensitivity. Differences in instrument configurations, chromatographic conditions, operator techniques, and sample handling can alter SNR, potentially leading to inconsistent results and failed method transfers [59] [6]. This article systematically compares contemporary approaches for optimizing LC-MS/MS sensitivity, providing experimental data and detailed protocols to support robust method transfer and reliable bioanalysis in pharmaceutical research and development.
Core Principles: Signal, Noise, and Their Impacts on Bioanalysis
Fundamental Relationship Between Signal-to-Noise Ratio and Detection
The signal-to-noise ratio is mathematically defined as the ratio of the power of a signal to the power of background noise, typically expressed in decibels (dB) [58]. For LC-MS/MS, this translates practically to the ability to distinguish analyte peaks from baseline variability. The fundamental relationship is:
[ \mathrm{SNR} = \frac{P{\mathrm{signal}}}{P{\mathrm{noise}}} = \left(\frac{A{\mathrm{signal}}}{A{\mathrm{noise}}}\right)^2 ]
where (P) represents power and (A) represents amplitude [58]. In chromatographic terms, signal amplitude corresponds to peak height, while noise amplitude represents baseline fluctuation. During method transfer, maintaining a consistent and high SNR is critical for ensuring that detection and quantification limits remain comparable between the originating and receiving laboratories [59].
Understanding sources of noise and signal loss is essential for effective optimization. The most significant challenges include:
- Ion Suppression: A pervasive obstacle where co-eluting matrix components reduce ionization efficiency of target analytes, leading to decreased signal intensity and compromised quantification accuracy [57]. This is particularly problematic during method transfer when matrix compositions vary slightly between laboratories.
- Chemical Noise: Arises from contaminants, solvent impurities, or column bleed, contributing to elevated baseline and reduced SNR [57].
- Instrumental Noise: Electronic noise from detectors, fluctuations in fluidic systems, and ion source contamination all contribute to background noise [57].
- Analyte Interactions: Metal-sensitive analytes, such as phosphorylated compounds, can adsorb to metal surfaces in the LC flow path, reducing signal intensity [20].
Comparative Analysis of Sensitivity Optimization Approaches
Chromatographic Hardware and Column Technologies
Advances in chromatographic hardware significantly impact sensitivity by reducing noise sources and improving signal recovery. The following table compares recent innovations in column technology based on 2025 market introductions and research presentations [20] [60].
Table 1: Comparison of Recent LC Column Technologies for Sensitivity Enhancement
| Technology Category | Example Products | Key Features | Impact on Sensitivity | Primary Applications |
|---|---|---|---|---|
| Inert Hardware Columns | Halo Inert (Advanced Materials Technology), Restek Inert HPLC Columns, Evosphere Max (Fortis) | Metal-free flow path, passivated surfaces | Enhanced peak shape and improved recovery for metal-sensitive analytes; reduces adsorption losses [20] | Phosphorylated compounds, chelating analytes, pharmaceuticals [20] |
| Specialized Stationary Phases | Halo 90 Å PCS Phenyl-Hexyl, SunBridge C18 (ChromaNik), Aurashell Biphenyl (Horizon) | Alternative selectivity, high pH stability, π-π interactions | Improved peak shape for basic compounds; alternative selectivity reduces co-elution [20] | Metabolomics, polar/non-polar compounds, isomer separations [20] |
| Microfluidic and Pillar Array | Thermo Fisher Scientific micropillar array columns | Lithographically engineered, uniform flow path | High precision and reproducibility; reduces dispersion noise [19] | High-throughput proteomics, multiomics studies [19] |
| Superficially Porous Particles | Raptor columns (Restek), Ascentis Express (Merck) | Fused-core particles with optimized pore structure | Faster mass transfer, sharper peaks, increased signal height [20] | Fast analysis, high-resolution separations [20] |
LC Configuration and Operational Strategies
Beyond column selection, how the LC system is configured and operated dramatically affects sensitivity. The following table compares different LC configuration strategies based on recent studies and implementation cases [57] [60].
Table 2: Comparison of LC Configuration Strategies for Sensitivity Enhancement
| Configuration Approach | Implementation Details | Signal Enhancement Mechanism | Experimental Sensitivity Gain | Considerations for Method Transfer |
|---|---|---|---|---|
| Microflow LC-MS/MS | 1 µL/min flow, 0.1 mm i.d. columns [60] | Reduced sample dilution, improved ionization efficiency [60] | 47-fold increase for insulin degludec vs. conventional systems [60] | Requires specialized equipment; more susceptible to clogging [60] |
| Online Preconcentration | Large volume injection (80-500 µL) with trapping columns [60] | Analyte focusing before separation | Enables detection of low-abundance metabolites; improves utilization of limited samples [60] | Additional method complexity; requires validation of trapping efficiency [60] |
| Advanced Mobile Phase Optimization | Volatile buffers (ammonium formate/acetate), pH control [57] | Enhanced spray stability, ionization efficiency [57] | Not quantified but critical for robustness [57] | Must be standardized in transfer protocols [59] |
| Reduced Flow Path Interactions | Hybrid surface technologies, inert materials [57] | Minimizes analyte adsorption and decomposition | Improved signal stability, especially for metal-sensitive compounds [20] [57] | Essential for phosphoproteins, oligonucleotides [20] |
Experimental Protocols for Sensitivity Enhancement
Protocol: Microflow LC-MS/MS for Enhanced Sensitivity in Pharmacokinetic Studies
Microflow LC-MS/MS has demonstrated remarkable sensitivity improvements in preclinical studies, particularly valuable for method transfer when lower limits of quantification are required.
Experimental Workflow [60]:
- Sample Preparation: Process plasma samples (5-10 µL) via protein precipitation or solid-phase extraction. Minimize sample dilution to maintain concentration.
- Chromatographic System:
- Utilize a microflow-capable LC system with low-dispersion fluidics.
- Employ a 0.1-0.3 mm i.d. column packed with sub-2µm particles.
- Set flow rate to 1-5 µL/min based on column dimensions.
- Use shallow gradients (typically 10-20 minutes) for separation.
- MS Interface:
- Employ a microflow-optimized electrospray ionization source.
- Optimize desolvation temperature and gas flows for low flow rates.
- Data Acquisition:
- Implement extended dwell times if needed for low-abundance ions.
- Use scheduled MRM for maximum efficiency across peaks.
Key Experimental Data: In a recent study of insulin degludec, microflow LC-MS/MS (1 µL/min flow, 0.1 mm i.d.) achieved a 47-fold sensitivity increase compared to conventional LC-MS/MS systems, allowing quantification in very low plasma volumes while reducing animal use in accordance with 3Rs principles [60].
Protocol: Online Preconcentration for Trace Analysis
Online preconcentration enables larger injection volumes without chromatographic distortion, particularly valuable for detecting low-concentration analytes in complex matrices.
Experimental Workflow [60]:
- System Configuration:
- Implement a dual-column system with a trapping column (e.g., 10-20 mm length) and analytical column.
- Use a 2-position/6-port valve for column switching.
- Loading Phase:
- Inject large sample volumes (80-500 µL) onto the trapping column.
- Use a weak mobile phase (high aqueous) to retain analytes on the trap while washing unretained matrix components to waste.
- Elution Phase:
- Switch the valve to back-flush analytes from the trapping column onto the analytical column.
- Apply the analytical gradient for separation.
- Re-equilibration:
- Re-equilibrate both columns for the next injection.
Application Note: This approach has been successfully applied in drug metabolism studies using LC-fluor-ICP-MS setups, providing a promising alternative for radiolabeled human metabolism studies where sample amounts may be limited [60].
Protocol: Mitigating Ion Suppression Through Sample Cleanup and Chromatography
Ion suppression remains a fundamental challenge in bioanalysis, particularly during method transfer where matrix differences may emerge.
Systematic Approach [57]:
- Sample Preparation Optimization:
- Compare solid-phase extraction (SPE), protein precipitation, and liquid-liquid extraction for specific analyte-matrix combinations.
- Implement selective SPE sorbents to remove phospholipids and other common suppressors.
- Chromatographic Separation:
- Extend gradient time to separate analytes from matrix components.
- Use alternative stationary phases (e.g., HILIC) for different selectivity.
- Adjust mobile phase pH to shift retention of ionizable suppressors.
- Matrix Effect Assessment:
- Post-column infuse analyte while injecting extracted blank matrix to identify suppression zones.
- Compare neat standard responses with matrix-matched samples.
- Source Maintenance:
- Implement regular cleaning schedules for ion source and interface components.
- Monitor signal deterioration as an indicator for required maintenance.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for LC-MS/MS Sensitivity Optimization
| Item Category | Specific Examples | Function in Sensitivity Optimization |
|---|---|---|
| Inert LC Columns | Restek Raptor Inert, Halo Inert, Fortis Evosphere Max | Minimize metal-analyte interactions, improve recovery for metal-sensitive compounds [20] |
| Specialty Stationary Phases | Biphenyl phases, Polar-embedded C18, HILIC columns | Provide alternative selectivity to separate analytes from suppressing matrix components [20] |
| Volatile Buffers | Ammonium formate, ammonium acetate | Maintain MS compatibility while controlling retention and selectivity [57] |
| High-Purity Solvents | LC-MS grade solvents, low-water-absorbing acetonitrile | Reduce chemical noise, improve baseline stability [57] |
| Selective SPE Sorbents | Phospholipid removal plates, mixed-mode sorbents | Remove specific matrix interferents that cause ion suppression [57] |
| Quality Control Materials | Charcoal-stripped matrix, stable isotope-labeled standards | Assess and correct for matrix effects; ensure quantification accuracy [6] |
Visualization of Optimization Strategies
The following diagram illustrates the strategic relationship between different sensitivity optimization approaches, providing a systematic framework for method development and transfer.
Diagram Title: LC-MS/MS Sensitivity Optimization Framework
Method Transfer Considerations for Sensitivity-Critical Applications
Successfully transferring methods while maintaining sensitivity requires careful planning and execution. Several strategies can facilitate this process:
- Comparative Testing: The most prevalent transfer approach, requiring both sending and receiving laboratories to test uniform material batches with predefined acceptance criteria for sensitivity metrics (SNR, LLOQ) [6].
- Covalidation: When GMP testing involves multiple laboratories, the receiving laboratory becomes part of the validation team and conducts intermediate precision experiments to generate reproducibility data [6].
- Risk-Based Revalidation: If the originating laboratory is unavailable, a risk-based approach determines which validation aspects need repetition by the receiving laboratory, focusing particularly on sensitivity parameters [6].
Emerging technologies like Multi-Attribute Monitoring (MAM) using LC-MS are gaining traction for quality control release testing of biopharmaceuticals, providing more data-rich characterization that can enhance method transfer through better understanding of product quality attributes [60].
Optimizing LC-MS/MS sensitivity through strategic signal enhancement and noise reduction is fundamental to successful bioanalysis, particularly during method transfer where consistency across laboratories is critical. Contemporary approaches including microflow LC, inert column hardwar
Addressing Matrix Effects and Selectivity Challenges
In bioanalytical chromatography, matrix effects and selectivity present formidable challenges that can compromise assay accuracy, reproducibility, and regulatory compliance. Matrix effects, defined as the combined influence of all sample components other than the analyte on measurement, manifest as ion suppression or enhancement in mass spectrometry and various chemical and physical interferences in other detection platforms [61] [62]. Selectivity, the ability to unequivocally identify and quantify the analyte in the presence of interfering components, becomes particularly difficult when methods are transferred between laboratories, instruments, or sample matrices.
The successful transfer of bioanalytical methods represents a critical juncture in the drug development lifecycle, where failures due to matrix effects or selectivity issues can incur costs of $10,000–$14,000 per deviation investigation and delay timelines at approximately $500,000 per day in unrealized sales [36]. This guide objectively compares contemporary approaches for addressing these challenges, providing researchers with experimental data and methodologies to enhance method robustness during technology transfer.
Comparative Analysis of Bioanalytical Platforms
Oligonucleotide therapeutics exemplify the challenges in bioanalysis, where multiple platforms must navigate complex biological matrices. A 2024 systematic comparison of four bioanalytical methods for quantifying a 21-mer lipid-conjugated siRNA (SIR-2) revealed distinct performance characteristics across platforms [14].
Table 1: Performance Comparison of Oligonucleotide Bioanalytical Platforms
| Platform | Sensitivity | Specificity | Throughput | Matrix Effect Management | Key Limitations |
|---|---|---|---|---|---|
| Hybrid LC-MS | High (LLOQ ≤1 ng/mL) | High (metabolite identification possible) | Moderate | Selective extraction reduces effects | Requires analyte-specific reagents |
| SPE/LLE-LC-MS | Moderate | High (metabolite identification possible) | Low | Generic sample preparation | Poorer sensitivity and throughput |
| HELISA | High | Low (cannot discriminate parent from metabolites) | High | Depends on probe specificity | Extensive method development |
| SL-RT-qPCR | High | Low (cannot discriminate parent from metabolites) | High | Amplification affected by inhibitors | Requires specific primers/probes |
All platforms generated comparable pharmacokinetic profiles, though HELISA and SL-RT-qPCR consistently reported higher concentrations, likely due to metabolite cross-reactivity [14]. This systematic comparison highlights the inherent trade-offs between sensitivity, specificity, and throughput when selecting platforms for method transfer.
Experimental Protocols for Matrix Effect Assessment
MCR-ALS Matrix Matching Strategy
Multivariate Curve Resolution-Alternating Least Squares (MCR-ALS) provides a chemometric approach to address matrix effects through intelligent calibration set selection [61].
Experimental Protocol:
- Prepare multiple calibration sets with varying matrix compositions
- Decompose data matrices for each calibration set and unknown samples: D = CSáµ€ + E
- Apply MCR-ALS constraints (non-negativity, closure, selectivity) to resolve concentration (C) and spectral (S) profiles
- Calculate similarity metrics between unknown samples and calibration sets using:
- Spectral correlation (angle between spectral loadings)
- Concentration profile comparison
- Select optimal calibration set with highest similarity to unknown sample matrix
- Validate prediction accuracy with independent test samples
This approach was validated on both simulated and real datasets, demonstrating improved prediction accuracy through optimal matrix matching prior to analysis [61].
Functionalized Monoliths for Selective Extraction
Advances in solid-phase extraction materials offer powerful alternatives for managing matrix effects. Functionalized monoliths, particularly those with biomolecules or molecularly imprinted polymers (MIPs), provide selective extraction capabilities [63].
Experimental Protocol for MIP Monolith Synthesis:
- Capillary pretreatment: Activate inner surface for monolith anchoring
- Prepare polymerization mixture: Template molecule, functional monomers, cross-linker, and initiator in porogenic solvent
- Initiate in-situ polymerization within capillary or microchip channel
- Remove template molecules with selective solvents to create specific cavities
- Characterize monolith permeability and specificity
- Couple with nanoLC or direct detection systems
In one application, this protocol enabled cocaine analysis in human plasma with only 100 nL of diluted plasma and overall solvent consumption of ~1 μL per sample while achieving necessary detection limits with simple UV detection [63].
Hybrid LC-MS for Oligonucleotide Bioanalysis
The hybrid LC-MS platform combines hybridization-based sample preparation with LC-MS detection, offering enhanced sensitivity for challenging analytes [14].
Detailed Methodology:
- Sample Preparation:
- Add LNA capture probes to plasma samples
- Hybridize target oligonucleotide with probes
- Capture using streptavidin magnetic beads
- Wash to remove matrix components
- Elute purified analyte
LC-MS Analysis:
- Chromatography: Reverse-phase with ion-pairing reagents (DMBA, HFIP)
- Mass spectrometry: MRM detection on triple quadrupole instrument
- Internal standardization: Analog siRNA (ISTD-3)
Method Validation:
- Establish linearity (1-1000 ng/mL)
- Determine precision and accuracy (CV <15%)
- Assess recovery and matrix effects
- Test specificity against metabolites
Visualization of Method Transfer Workflows
Digital Method Transfer Process
Matrix Effect Assessment Strategy
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Addressing Matrix Effects
| Reagent/Material | Function | Application Example |
|---|---|---|
| Molecularly Imprinted Polymers (MIPs) | Selective extraction templates | Creating cavities complementary to target molecules for specific retention [63] |
| Locked Nucleic Acid (LNA) Probes | High-affinity capture probes | Hybridization-based extraction of oligonucleotides from biological matrices [14] |
| Functionalized Monolithic Materials | Low back-pressure, high surface area sorbents | Online SPE-LC coupling for automated sample preparation [63] |
| Stable Isotope-Labeled Internal Standards | Compensation for ionization effects | Correcting for matrix-induced ion suppression/enhancement in LC-MS [62] |
| Ion-Pairing Reagents (DMBA/HFIP) | Chromatographic separation of polar analytes | Enabling retention and separation of oligonucleotides in reversed-phase LC [14] |
| Biomolecule-Grafted Monoliths | Affinity-based extraction | Immobilized antibodies or aptamers for selective target capture [63] |
Addressing matrix effects and selectivity challenges requires a systematic approach combining appropriate platform selection, strategic sample preparation, and intelligent data processing. The comparative data presented herein demonstrates that while LC-MS platforms offer superior specificity for metabolite discrimination, ligand-binding assays provide advantages in sensitivity and throughput for oligonucleotide bioanalysis. Emerging technologies including functionalized monoliths, digital method transfer protocols, and MCR-ALS chemometric approaches represent significant advancements in managing matrix complexity.
Successful method transfer hinges on proactive mitigation of matrix effects through standardized assessment protocols and careful consideration of the inherent strengths and limitations of each analytical platform. By implementing these evidence-based strategies, researchers can enhance method robustness, accelerate technology transfer, and maintain data integrity throughout the drug development lifecycle.
Navigating Instrumentation Differences Between Laboratories
The successful transfer of bioanalytical methods between laboratories is a critical yet challenging milestone in drug development. Variability in analytical instrumentation—including differences in manufacturer, model, sensitivity, and data processing algorithms—can significantly impact the reliability, accuracy, and precision of pharmacokinetic and toxicokinetic data [42]. This variability introduces substantial risks during method transfer, potentially compromising data integrity, regulatory submissions, and ultimately, drug development timelines.
The core challenge lies in the fundamental differences between instrumental platforms, even when analyzing the same analyte. As demonstrated in a 2024 systematic comparison of bioanalytical platforms for oligonucleotide therapeutics, different methodologies like LC-MS, hybridization ELISA (HELISA), and stem-loop reverse transcription quantitative PCR (SL-RT-qPCR) can produce varying concentration readings for the same sample due to inherent differences in detection specificity, sensitivity to metabolites, and calibration approaches [14]. Navigating these differences requires a thorough understanding of instrumental parameters, systematic comparison strategies, and robust validation protocols to ensure data consistency across laboratories and throughout the drug development lifecycle.
Comparative Analysis of Major Bioanalytical Platforms
Understanding the relative strengths and limitations of common bioanalytical platforms provides the foundation for navigating instrumental differences. Each technology offers distinct advantages for specific applications, creating inherent variability when methods are transferred between laboratories utilizing different systems.
Table 1: Comparison of Common Bioanalytical Platform Performance Characteristics
| Platform | Optimal Application | Sensitivity | Throughput | Specificity | Key Distinguishing Feature |
|---|---|---|---|---|---|
| LC-MS/MS [64] | Small molecules, some peptides & oligonucleotides | High | Medium | High (can identify metabolites) | Gold standard for small molecules; potential for metabolite identification |
| Hybrid LC-MS [14] | siRNA, oligonucleotides | Very High (≤1 ng/mL LLOQ) | Medium | High | Combines hybridization capture with MS detection |
| SPE/LLE-LC-MS [14] | siRNA, small molecules | Medium | Lower | High | Uses generic reagents; shorter method development time |
| HELISA [14] | Proteins, antibodies, oligonucleotides | High | High | Lower (may detect metabolites) | High throughput; requires analyte-specific reagents |
| SL-RT-qPCR [14] | Nucleotides (mRNA, miRNA, siRNA) | Very High | High | Lower (may detect metabolites) | Extremely high sensitivity for genetic material |
| MSD [64] | Large molecules, biomarkers | High (broad dynamic range) | Medium | High | Electrochemiluminescence; multiplex capabilities |
The data from this comparative analysis reveals a clear trade-off between specificity and throughput. While LC-MS platforms generally provide superior specificity and the ability to discriminate between parent compounds and their metabolites, ligand-binding assays like HELISA and PCR-based methods like SL-RT-qPCR typically offer higher throughput and sensitivity but may lack metabolic discrimination [14]. These inherent technological differences directly impact method transfer outcomes, necessitating platform-specific validation and bridging strategies.
Chromatographic Instrumentation: From LC to UHPLC
Liquid chromatography forms the backbone of many bioanalytical methods, and significant evolution in this technology has introduced additional complexity to method transfer. The progression from Traditional Liquid Chromatography (LC) to High-Performance Liquid Chromatography (HPLC) and Ultra-High-Performance Liquid Chromatography (UHPLC) represents not just incremental improvements but fundamental shifts in separation science with direct implications for method transfer.
Table 2: Evolution of Liquid Chromatography Technologies and Transfer Considerations
| Parameter | Traditional LC | HPLC | UHPLC |
|---|---|---|---|
| Operating Pressure | Low (gravity-fed) | Up to 400 bar [65] | Up to 1,500 bar [65] |
| Particle Size | ≥10 μm [65] | 3-5 μm [65] | <2 μm [65] |
| Separation Efficiency | Low resolution, broad peaks | High resolution, sharper peaks | Ultra-high resolution, narrowest peaks |
| Analysis Speed | Slow | Moderate to Fast | Very Fast |
| Sensitivity | Lower | Higher | Highest |
| Transfer Complexity | Low | Moderate | High (requires specialized equipment) |
The kinetic performance differences between these systems create substantial transfer challenges. The kinetic plot method provides a valuable framework for comparing column performance across different platforms by transforming Van Deemter curve data into a more practically relevant representation of analysis time versus efficiency [66]. This approach allows scientists to determine whether a method developed on one system (e.g., HPLC) can be successfully transferred to another (e.g., UHPLC) while maintaining the required resolution, or if re-optimization is necessary to account for the different performance characteristics.
Experimental Protocols for Systematic Instrument Comparison
Protocol 1: Cross-Platform Bioanalytical Method Comparison
A rigorous experimental design is essential for meaningful instrument comparison. A 2024 study provides a robust template for comparing multiple assay platforms using the same analyte, in this case, an siRNA therapeutic (SIR-2) [14].
Materials and Reagents:
- Analyte: SIR-2 (21-mer lipid-conjugated siRNA) reference material [14]
- Internal Standard: ISTD-3 (unrelated lipid-conjugated siRNA) for LC-MS assays [14]
- Biological Matrix: Control Kâ‚‚EDTA plasma [14]
- Platform-Specific Reagents: Locked nucleic acid (LNA) capture probes for Hybrid LC-MS and HELISA; stem-loop primers for SL-RT-qPCR [14]
Experimental Methodology:
- Calibrator and QC Preparation: Freshly prepare calibration standards and quality control samples in plasma from independent dilutions of a SIR-2 sub-stock solution [14].
- Parallel Sample Analysis: Analyze samples from a pre-clinical pharmacokinetic study using all four platforms:
- Hybrid LC-MS: Hybridization capture with magnetic beads followed by LC-MS analysis [14]
- SPE-LC-MS: Solid-phase extraction followed by LC-MS analysis [14]
- HELISA: Hybridization ELISA with digoxigenin-labeled probes and ruthenium-labeled detection antibodies [14]
- SL-RT-qPCR: Stem-loop reverse transcription quantitative PCR [14]
- Data Comparison: Compare quantitative results, pharmacokinetic profiles, sensitivity (LLOQ), precision, accuracy, and throughput across all platforms [14].
Expected Outcomes: This protocol typically reveals that while all platforms generate comparable PK profiles, non-LC-MS methods (HELISA, SL-RT-qPCR) may yield higher observed concentrations due to reduced metabolite discrimination. Furthermore, it quantifies inherent platform differences, with Hybrid LC-MS and SL-RT-qPCR demonstrating the highest sensitivity, while SL-RT-qPCR and HELISA show superior throughput [14].
Protocol 2: HPLC/UHPLC System Performance Comparison
For chromatographic systems, a standardized protocol for performance benchmarking is crucial for successful method transfer.
Materials and Reagents:
- Test Column: Identical column chemistry (e.g., C18, same particle lot) for both systems
- Test Analytes: A mixture of representative compounds covering a range of hydrophobicities
- Mobile Phase: Identical composition and pH for both systems
Experimental Methodology:
- System Suitability Test: Perform a standard system suitability test to verify baseline performance.
- Van Deemter Curve Generation: Measure height equivalent to a theoretical plate (HETP) across a range of flow rates for both systems [66].
- Permeability Assessment: Determine column permeability (K_v0) from pressure-flow rate relationships [66].
- Kinetic Plot Transformation: Use the following equations to transform (uâ‚€, H) data points into kinetic plots representing the trade-off between analysis time and efficiency:
- Analysis Time: ( t0 = \frac{H}{u0} \times N ) [66]
- Plate Number: ( N = \frac{\Delta P}{η} \times \frac{K{v0}}{u0 \times H} ) [66] where ( u0 ) is the linear velocity, H is the plate height, N is the plate number, ΔP is the maximum operating pressure, η is the mobile phase viscosity, and Kv0 is the column permeability.
- Resolution Mapping: Measure resolution (R_s) for critical pairs of analytes across different gradient times and temperatures.
Expected Outcomes: This protocol generates a direct, visual comparison of the separation speed-efficiency trade-off for different systems, enabling scientists to predict whether a method transfer is feasible and what adjustments (e.g., column length, flow rate) are necessary to maintain performance [66].
Workflow Visualization: Navigating Method Transfer
The following workflow diagrams provide a visual guide to the key processes for instrument comparison and method transfer.
Instrument Comparison & Method Transfer Workflow
Kinetic Plot Analysis for Chromatography Transfer
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful navigation of instrumental differences relies on high-quality, standardized materials. The following toolkit outlines critical reagents and their functions in comparative studies and method transfers.
Table 3: Essential Research Reagents and Materials for Instrument Comparison Studies
| Reagent/Material | Function & Importance | Key Considerations |
|---|---|---|
| Analyte Reference Standard [14] | Primary standard for quantification; ensures accuracy across platforms. | High purity (≥90%); well-characterized stability; identical lot used across all comparison studies. |
| Stable Isotope-Labeled Internal Standard [14] | Normalizes extraction efficiency, matrix effects, and instrument variability in LC-MS. | Should be structurally analogous but chromatographically resolvable from the analyte. |
| Capture Probes / Primers [14] | Enables specific analyte capture or amplification in Hybrid LC-MS, HELISA, and SL-RT-qPCR. | Sequence specificity is critical; locked nucleic acid (LNA) probes can enhance hybridization stringency. |
| Critical Ligand-Binding Reagents (e.g., antibodies, ruthenium-labeled detectors) [14] [64] | Form the basis of specificity in immunoassays and HELISA. | Lot-to-lot variability is a major risk; bulk procurement or thorough cross-lot validation is required. |
| Standardized Biological Matrix (e.g., Kâ‚‚EDTA plasma) [14] | Provides a consistent baseline for assessing platform performance in a relevant environment. | Sourced from a reputable provider; screened for endogenous interferents; single, large lot is ideal. |
| Specialized Mobile Phase Additives (e.g., DMBA, HFIP) [14] | Improve chromatographic peak shape and sensitivity for oligonucleotides and peptides in LC-MS. | Quality and freshness are critical; should be prepared and used within a defined shelf-life (e.g., 48 hours). |
Future Trends: AI, Automation, and Standardization
The future of navigating instrumental differences is being shaped by technological advancements that promote consistency and intelligence. Artificial Intelligence (AI) and Machine Learning are now being deployed to streamline method validation and transfer. AI algorithms can predict optimal method parameters, simulate robustness under variable conditions, and automatically review vast validation datasets for anomalies, significantly reducing the manual effort and subjectivity involved in cross-instrument comparisons [67].
Furthermore, the push for instrument standardization and interoperability is gaining momentum. The lack of common communication protocols and data formats between different manufacturers' instruments has long been a barrier to seamless method transfer [67]. The industry is moving toward broad adherence to shared standards (such as SiLA or AnIML), which facilitates the automated transfer of methods and data, creating a more uniform analytical environment [67]. Concurrently, the integration of automation and robotics in sample preparation and analysis minimizes human-derived variability, thereby reducing a major source of error during method transfer and ensuring that instrumental differences, rather than operational inconsistencies, are the primary focus of comparison studies [68]. These trends collectively promise a future where bioanalytical method transfer is more predictable, efficient, and reliable.
Ensuring Data Equivalency: Validation, Cross-Validation, and Acceptance Criteria
Distinguishing Between Full, Partial, and Cross-Validation
In the field of bioanalytical chromatography research, the reliability of quantitative data is paramount for making critical decisions in drug development, from preclinical studies to clinical trials. Method validation provides documented evidence that an analytical method is fit for its intended purpose, ensuring the accuracy, precision, and reproducibility of results for regulatory submission. Within this context, three distinct validation approaches have emerged: full validation, partial validation, and cross-validation, each serving specific purposes in the method lifecycle.
Full validation represents the comprehensive evaluation of a method's performance characteristics, typically conducted for novel methodologies or when significant changes occur. Partial validation consists of a limited validation exercise, performed when modifications are made to an already validated method. Cross-validation, while sometimes confused with the statistical technique of cross-validation in machine learning, specifically refers to the comparison of two bioanalytical methods to ensure their equivalence and reliability when applied to the same analytical samples [69]. Understanding the distinctions, applications, and regulatory expectations for each approach is essential for researchers, scientists, and drug development professionals engaged in method transfer and bioanalytical assays.
Full Validation: Comprehensive Method Assessment
Definition and Scope
Full validation constitutes a complete characterization of a bioanalytical method's performance, establishing that it reliably meets all specified analytical requirements. According to regulatory guidelines, including those outlined in the Chinese Pharmacopoeia (9012) and other international standards, full validation is mandatory for new analytical methods or when quantifying a new molecular entity [70] [69]. This comprehensive approach ensures that the method produces results with acceptable accuracy, precision, selectivity, and robustness under defined operational conditions.
The scope of full validation encompasses all critical method parameters that could impact result quality and reliability. As specified in bioanalytical guidance documents, this includes assessment of selectivity, sensitivity, accuracy, precision, matrix effects, stability, and dilution integrity [70] [69]. Each parameter must be rigorously tested using quality control samples prepared in the appropriate biological matrix to simulate real-world analytical conditions.
Experimental Parameters and Acceptance Criteria
A full validation requires systematic evaluation of multiple performance parameters against predefined acceptance criteria, which are well-established in regulatory guidelines. The following table summarizes the key parameters and their typical acceptance criteria for chromatographic methods:
Table 1: Key Parameters and Acceptance Criteria for Full Validation
| Validation Parameter | Experimental Design | Acceptance Criteria |
|---|---|---|
| Selectivity | Analyze ≥6 individual matrix lots; assess potential interferents | Interference <20% of LLOQ and <5% of internal standard [70] |
| Accuracy and Precision | Analyze ≥5 replicates at LLOQ, Low, Mid, High QC levels across ≥3 runs | Within-run: ±15% (±20% for LLOQ); Between-run: ±15% (±20% for LLOQ) [70] |
| Linearity and Calibration Curve | ≥6 non-zero concentrations; assess by appropriate regression model | ±15% of nominal (±20% at LLOQ); ≥75% of standards meeting criteria [70] |
| Lower Limit of Quantification (LLOQ) | Determine lowest measurable concentration with acceptable accuracy and precision | Signal-to-noise ≥5; accuracy within ±20%; CV ≤20% [70] [69] |
| Matrix Effects | Evaluate ≥6 individual matrix lots; assess ion suppression/enhancement | CV of normalized matrix factor ≤15% [70] [69] |
| Stability | Evaluate bench-top, processed, freeze-thaw, long-term conditions | ±15% of nominal concentration [70] |
| Dilution Integrity | Test beyond ULOQ samples with appropriate dilution factors | ±15% of nominal concentration [70] |
| Carryover | Inject blank after high concentration sample | ≤20% of LLOQ and ≤5% of internal standard [70] |
Regulatory Requirements and Experimental Protocol
The experimental protocol for full validation must adhere to Good Laboratory Practice (GLP) principles, with detailed documentation of all procedures, results, and deviations. The fundamental sequence involves method development followed by the systematic verification of each parameter outlined in Table 1.
The typical workflow begins with establishing selectivity and specificity against potential interferents, including metabolites, concomitant medications, and endogenous matrix components [70]. The calibration curve is then validated across the analytical measurement range, using a minimum of six concentration levels (excluding blanks), with at least 75% of standards meeting acceptance criteria [70].
Accuracy and precision are demonstrated through the analysis of quality control (QC) samples at a minimum of four concentration levels (LLOQ, Low, Medium, High) in replicates of at least five per concentration across a minimum of three analytical runs [70]. The analysis of at least three runs on different days by different analysts demonstrates robust method performance under varied conditions. Stability experiments must cover all anticipated storage and handling conditions, with testing conditions that mirror actual sample processing, storage, and analysis timelines [70].
Partial Validation: Targeted Method Reevaluation
Concept and Applications
Partial validation refers to a limited validation exercise performed when modifications are made to an already validated bioanalytical method. These modifications may not warrant a full revalidation but require demonstration that the method still performs adequately for its intended use. The Chinese Pharmacopoeia (9012) and other regulatory guidelines recognize that certain changes to validated methods necessitate a scientific evaluation to determine the extent of revalidation required [70] [69].
Common scenarios requiring partial validation include: transfer of the method between laboratories or analysts; changes in analytical methodology (e.g., detector settings, column type); changes in sample processing procedures; changes in anticoagulant for blood/plasma samples; and incorporation of new instrumentation or software platforms [69]. The extent of partial validation depends on the nature of the change, with more significant alterations requiring more comprehensive evaluation.
Experimental Design Considerations
The design of partial validation studies follows a risk-based approach, focusing on method parameters most likely to be affected by the specific change. The following table outlines common modification scenarios and the corresponding parameters typically assessed in partial validation:
Table 2: Partial Validation Scenarios and Assessment Parameters
| Modification Scenario | Parameters Typically Assessed | Rationale |
|---|---|---|
| Transfer between laboratories | Accuracy, precision, reproducibility | Account for analyst technique, environmental factors, equipment differences [69] |
| Change in sample processing | Extraction efficiency, accuracy, precision, selectivity | Ensure modified procedure maintains analytical recovery and specificity [69] |
| Change in instrumentation | Linearity, sensitivity, matrix effects, carryover | Verify performance with new detection systems or interfaces [69] |
| Change in bioanalytical matrix | Selectivity, matrix effects, accuracy | Ensure method performance in new matrix (e.g., plasma to serum) [70] |
| Minor method optimization | Specific affected parameters (e.g., precision for modified chromatography) | Focus on parameters directly impacted by the change [69] |
The experimental protocol for partial validation should follow the same principles as full validation but with reduced scope. For example, when transferring a method between laboratories, a single validation run containing a calibration curve and QC samples at low, medium, and high concentrations may be sufficient to demonstrate equivalent performance [69]. Accuracy and precision may be evaluated through a minimum of one analytical run with five replicates per QC level, rather than the multiple runs required for full validation [70].
Documentation of partial validation must clearly describe the change implemented, scientific justification for the partial validation approach, the specific parameters evaluated, experimental data, and a conclusion regarding the method's suitability post-modification.
Cross-Validation: Establishing Method Equivalence
Purpose in Bioanalytical Context
In bioanalytical chromatography, cross-validation specifically refers to the process of comparing two bioanalytical methods to demonstrate their equivalence when applied to the same analytical samples [69]. This differs from the statistical cross-validation technique used in machine learning for model performance estimation. Bioanalytical cross-validation is essential when multiple methods are used to generate data within the same study, when methods are transferred between laboratories, or when comparing original and revised methods.
The primary objective is to ensure that results from different methods or different sites are comparable and that any observed differences do not impact the scientific conclusions or regulatory decisions based on the data. Global regulatory guidelines, including those from FDA, EMA, and ICH, emphasize the importance of cross-validation when data from multiple sources are combined in regulatory submissions [69].
Method Comparison Approaches
The experimental design for cross-validation typically involves the analysis of a sufficient number of study samples or spiked quality control samples by both methods being compared. The following principles guide the approach:
Sample Selection: The samples should represent the entire concentration range encountered in the study, with particular attention to the low and high concentration regions where method differences are most likely to occur [69].
Sample Size: A sufficient number of samples (typically 10% of study samples or a minimum of 40 samples) should be analyzed to provide adequate statistical power for comparison [69].
Analysis Sequence: Samples should be analyzed by both methods within a time frame that ensures sample stability, preferably in randomized order to avoid bias.
Data Analysis: Results are compared using appropriate statistical tests, such as paired t-tests, regression analysis, or Bland-Altman plots, to assess systematic and random differences between methods.
Acceptance Criteria for Method Equivalence
The acceptance criteria for cross-validation studies depend on the context and criticality of the data. Generally, the mean accuracy and precision of results from both methods should be within the predefined acceptance criteria (typically ±15% for accuracy and ≤15% for precision) [69]. For incurred sample reanalysis (ISR), which represents a form of cross-validation, the percentage of individual sample results showing ≤20% difference between original and repeat analysis should be ≥67% [69].
Statistical approaches may include calculating the 90% confidence interval for the ratio of results between methods, with equivalence demonstrated if the entire confidence interval falls within specified limits (e.g., 80-125%) [69]. The specific acceptance criteria should be predefined in the study protocol based on the method's intended use and regulatory requirements.
Comparative Analysis of Validation Approaches
Strategic Application in Method Lifecycle
Each validation approach serves distinct purposes throughout the method lifecycle, from initial development through technology transfers and method updates. Understanding the strategic application of each approach ensures efficient resource allocation while maintaining data integrity and regulatory compliance.
The following diagram illustrates the relationship between these validation approaches and their position in the method lifecycle:
Decision Framework for Selection
The selection of the appropriate validation approach depends on multiple factors, including the method's development stage, the nature of any changes, and regulatory considerations. The following decision framework aids in selecting the appropriate validation strategy:
Table 3: Decision Framework for Validation Approach Selection
| Scenario | Recommended Approach | Key Considerations |
|---|---|---|
| New analytical method | Full validation | Required for regulatory submissions; establishes baseline performance [70] |
| New molecular entity | Full validation | Necessary for first-time quantification of analyte [70] [69] |
| Method transfer between laboratories | Partial validation + Cross-validation | Partial to verify performance; cross to compare with originating lab [69] |
| Minor method modifications | Partial validation | Scope based on risk assessment of the change [69] |
| Different methods in same study | Cross-validation | Ensures data comparability across methods [69] |
| Change in analytical platform | Partial validation | Assess parameters most likely affected by platform change [69] |
| Anticoagulant change | Partial validation | Evaluate selectivity, matrix effects, accuracy [70] |
Resource and Regulatory Considerations
Each validation approach demands different levels of resources, time, and documentation, factors that significantly impact project timelines and costs in drug development.
Full validation is the most resource-intensive, typically requiring 2-4 weeks for completion, extensive documentation, and significant quantities of reference standards and biological matrix [70]. Partial validation may be completed in 1-2 weeks with reduced material requirements, focusing only on parameters potentially affected by the change [69]. Cross-validation timeframes depend on sample analysis throughput but generally require less method characterization and more comparative data analysis [69].
Regulatory expectations vary accordingly. Full validation must comply with all aspects of regulatory guidelines (e.g., FDA BMV, EMA guidelines, ICH M10) [69]. For partial validation, regulatory agencies expect scientific justification for the reduced scope and documentation demonstrating that the change does not adversely affect method performance [69]. Cross-validation requires documentation of the comparison protocol, acceptance criteria, and results demonstrating method equivalence [69].
Experimental Protocols and Workflows
Comprehensive Full Validation Protocol
A robust full validation protocol for bioanalytical chromatography methods should systematically address all parameters outlined in Section 2.2. The following detailed workflow ensures regulatory compliance and methodological rigor:
Reference Standard Qualification: Verify purity, identity, and stability of analytical standards before validation begins. Document source, lot number, and certificate of analysis [70].
Selectivity and Specificity Assessment:
- Procure at least six individual batches of blank matrix from different sources
- Analyze blank matrix, zero samples (blank with IS), and LLOQ samples
- Assess for interference at retention times of analyte and IS
- Test potential interferents (metabolites, concomitant medications) [70]
Calibration Curve Establishment:
- Prepare calibration standards in replicate at 6-8 concentration levels
- Analyze in至少3 independent runs
- Apply appropriate weighting factor and regression model
- ≤25% of standards (excluding LLOQ) may be rejected; LLOQ must meet criteria [70]
Accuracy and Precision Determination:
- Prepare QC samples at LLOQ, Low, Medium, High concentrations (至少5 replicates each)
- Analyze in至少3 separate runs on different days
- Calculate within-run and between-run accuracy and precision [70]
Matrix Effect Evaluation:
Stability Assessment:
- Bench-top stability (ambient temperature, various time points)
- Processed sample stability (autosampler temperature)
- Freeze-thaw stability (至少3 cycles)
- Long-term stability (at storage temperature) [70]
Dilution Integrity and Carryover Testing:
- Prepare samples above ULOQ and dilute with blank matrix
- Inject blank samples after high concentration samples [70]
Streamlined Partial Validation Protocol
For partial validation, the protocol should focus on parameters most likely affected by the specific change:
Change Assessment: Document the specific modification and identify potentially impacted validation parameters [69].
Experimental Design:
- For method transfers: 1-2 complete analytical runs with calibration standards and QCs at all levels
- For processing changes: Focus on extraction efficiency, accuracy, and precision
- For matrix changes: Emphasize selectivity and matrix effects [69]
Acceptance Criteria Application: Apply the same acceptance criteria as full validation for the parameters being assessed [70] [69].
Comparative Analysis: When applicable, compare results with original validation data to demonstrate equivalence.
Cross-Validation Experimental Workflow
The cross-validation workflow focuses on method comparison rather than comprehensive characterization:
Sample Selection: Select incurred study samples or spiked QC samples covering the analytical range [69].
Experimental Design:
- Analyze samples using both methods within sample stability period
- Utilize identical sample aliquots when possible
- Randomize analysis order to minimize bias
- Ensure proper calibration of both methods before analysis [69]
Data Analysis:
- Calculate mean accuracy and precision for both methods
- Perform statistical comparison (e.g., paired t-test, regression analysis)
- Assess percentage of samples meeting equivalence criteria [69]
Equivalence Determination: Apply predefined acceptance criteria to determine method comparability.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of validation studies requires carefully selected reagents, materials, and instrumentation. The following table details essential components of the bioanalytical scientist's toolkit for method validation in chromatographic assays:
Table 4: Essential Research Reagents and Materials for Bioanalytical Validation
| Category | Specific Items | Function and Importance |
|---|---|---|
| Reference Standards | Certified analyte standard; Stable isotope-labeled internal standard | Quantification reference; compensation for variability [70] |
| Biological Matrices | Blank plasma/serum (≥6 individual lots); Hemolyzed/lipemic matrices for selectivity | Study-relevant matrix; assessment of selectivity and matrix effects [70] |
| Chromatography | HPLC/UPLC columns; Mobile phase solvents; Modifiers (acids, buffers) | Compound separation; peak shape optimization; retention control [70] |
| Sample Preparation | Extraction solvents; Solid-phase extraction cartridges; Protein precipitation reagents | Analyte isolation; matrix cleanup; interference removal [69] |
| Quality Controls | Spiked QC samples at LLOQ, Low, Mid, High concentrations | Method performance monitoring; acceptance criteria verification [70] |
| Instrumentation | LC-MS/MS system; Analytical balances; pH meters; Pipettes | Sample analysis; precise measurements; solution preparation [70] [69] |
The strategic distinction between full, partial, and cross-validation approaches represents a cornerstone of effective bioanalytical method management in chromatography research and drug development. Full validation establishes the foundational performance characteristics of novel methods, partial validation ensures continued suitability following modifications, and cross-validation confirms equivalence between different methods or laboratories.
This comparative guide demonstrates that the selection of appropriate validation strategy depends on the method's stage in its lifecycle, the nature of any changes, and regulatory requirements. By implementing the structured protocols, decision frameworks, and experimental designs outlined herein, researchers and drug development professionals can ensure robust, reliable, and regulatory-compliant bioanalytical methods that generate data fit for purpose in critical decision-making processes.
As regulatory landscapes continue to evolve with initiatives like ICH M10 aiming to harmonize global bioanalytical guidance, the fundamental principles of validation—demonstrating method reliability through appropriate scientific evidence—remain constant across all validation approaches [69].
Establishing Statistical Acceptance Criteria for Method Equivalency
In the field of bioanalytical chromatography research, method equivalency is a formal demonstration that two analytical procedures yield comparable results, ensuring the same accept/reject decisions for a drug substance or product [71]. Establishing equivalency is critical during method transfer between laboratories, changes to an existing analytical procedure, or when adopting a new methodology [42]. This process is foundational to a robust control strategy, ensuring that product quality and patient safety are maintained despite changes in the analytical lifecycle [71].
The fundamental principle of method equivalency lies in demonstrating that the differences in results generated by the original and the modified or transferred method are statistically insignificant in terms of accuracy and precision [71]. This guide provides a structured, data-driven approach to establishing statistical acceptance criteria for these studies, framed within the context of modern regulatory expectations, including those outlined in ICH Q14 for Analytical Procedure Lifecycle Management [72].
Regulatory and Statistical Framework
The Regulatory Imperative for Equivalency
Method equivalency studies are a regulatory requirement when a modified or new analytical method has an impact on the approved marketing authorization [71]. Health authorities require demonstration that the new procedure is equivalent or superior to the originally approved method before implementation. These changes must be managed under a strict change control process and often require submission to regulatory agencies for approval [71]. The International Council for Harmonisation (ICH) guidelines, particularly ICH Q2(R2) on analytical method validation and ICH Q14 on analytical procedure development, provide the core framework for these activities [71] [72].
Distinguishing Between Comparability and Equivalency
A critical concept is the distinction between comparability and equivalency, a differentiation emphasized in recent regulatory thinking:
- Comparability: Evaluates whether a modified method yields results sufficiently similar to the original, ensuring consistent product quality. These changes typically do not require regulatory filings [72].
- Equivalency: Involves a more comprehensive assessment, often requiring full validation, to demonstrate that a replacement method performs equal to or better than the original. Such changes require regulatory approval prior to implementation [72].
The Statistical Shift: Equivalence Testing over Significance Testing
Traditional hypothesis testing, which seeks to prove a difference (e.g., a t-test with a goal of p < 0.05), is not suitable for proving equivalence. Instead, equivalence testing is the statistically sound approach [73] [74].
The United States Pharmacopeia (USP) <1033> clearly states a preference for equivalence testing over significance testing. A significance test that fails to find a difference (p > 0.05) is not the same as confirming conformity to a target value, as the study might be underpowered [73]. Equivalence testing, specifically the Two One-Sided Tests (TOST) procedure, is designed to prove that a difference is smaller than a pre-defined, clinically or operationally irrelevant margin [73] [74]. The null hypothesis (H0) in equivalence testing posits that the methods are not equivalent, and the goal is to reject this null hypothesis to conclude equivalence [74].
Defining Acceptance Criteria: A Risk-Based Approach
The Foundation: Allowable Error Relative to Specification
A paradigm shift in setting acceptance criteria moves from traditional metrics like % coefficient of variation (%CV) to an approach that evaluates method error relative to the product's specification tolerance [75]. This links method performance directly to its impact on product quality and out-of-specification (OOS) rates [75].
The core concept is to determine how much of the product's specification tolerance is consumed by the analytical method's error. The tolerance is calculated as Upper Specification Limit (USL) - Lower Specification Limit (LSL). Method precision (repeatability) and accuracy (bias) are then expressed as a percentage of this tolerance [75].
Quantitative Acceptance Criteria for Validation Parameters
The following table summarizes recommended, risk-based acceptance criteria for key analytical performance parameters, expressed as a percentage of the specification tolerance.
Table 1: Risk-Based Acceptance Criteria for Analytical Method Performance
| Validation Parameter | Calculation (Relative to Specification) | Recommended Acceptance Criteria (% of Tolerance) | Risk Level |
|---|---|---|---|
| Repeatability | (Stdev * 5.15) / (USL - LSL) [75] | ≤ 25% [75] | High |
| Bias/Accuracy | Bias / (USL - LSL) [75] | ≤ 10% [75] | High |
| Specificity | (Measurement - Standard) / (USL - LSL) [75] | ≤ 10% [75] | High |
| LOD | LOD / (USL - LSL) [75] | ≤ 10% [75] | High |
| LOQ | LOQ / (USL - LSL) [75] | ≤ 20% [75] | High |
These criteria should be adapted based on risk. Higher risks (e.g., for a critical quality attribute with a narrow therapeutic index) demand stricter criteria, allowing only small practical differences. Lower risks may permit larger differences [73].
Setting the Equivalence Margin
The equivalence margin (Δ) is the pre-defined boundary within which differences between the two methods are considered practically insignificant. Setting this margin is a critical, risk-based decision that should consider scientific knowledge, product experience, and clinical relevance [73] [74]. A key consideration is the potential impact on process capability and OOS rates. The margin can be set as a percentage of the specification tolerance, with common risk-based benchmarks being:
- High Risk: 5-10% of tolerance
- Medium Risk: 11-25% of tolerance
- Low Risk: 26-50% of tolerance [73]
Experimental Protocols for Method Equivalency
Core Experimental Workflow
The process for conducting a method equivalency study follows a logical sequence from planning through execution and data analysis. The workflow is designed to ensure all critical parameters are evaluated and that the study is statistically sound.
Diagram 1: Equivalency Study Workflow
Detailed Study Designs and Protocols
Protocol for Method Transfer Equivalency
For a method transfer to another laboratory (an external transfer), a comprehensive protocol is required. The Global Bioanalytical Consortium (GBC) recommends the following for chromatographic assays [42]:
- Full Validation: The receiving laboratory must perform a full validation, including all accuracy and precision measurements.
- Accuracy and Precision: A minimum of two sets of accuracy and precision data using freshly prepared calibration standards over a 2-day period is required [42].
- Stability: Bench-top stability, freeze-thaw stability, and, where appropriate, extract stability must be re-established.
- Quality Controls (QCs): QCs at the Lower Limit of Quantification (LLOQ) must be assessed. ULOQ QCs are not required for internal transfers but are recommended for external transfers [42].
Protocol for a Paired-Comparison Equivalency Study
The most common design for an equivalency study is a paired comparison, where a set of representative samples is analyzed by both the original and the new method.
- Sample Selection: A minimum of 15 samples is recommended to ensure sufficient statistical power [73]. The samples should cover the specified range of the procedure, including the LLOQ, low, medium, and high concentrations.
- Analysis: The same set of samples is analyzed using both the original and candidate methods. The sample order should be randomized to avoid bias.
- Data Analysis: For each sample, calculate the difference between the results from the two methods. The set of differences is then used in the statistical equivalence test.
Statistical Analysis and Data Interpretation
The Two One-Sided Tests (TOST) Procedure
The TOST procedure is the standard method for testing equivalence. It involves performing two one-sided t-tests to evaluate whether the true difference between the methods is less than the positive equivalence margin (+Δ) and greater than the negative equivalence margin (-Δ) [73] [74].
Table 2: Formulas for the TOST Procedure
| Component | Formula | Interpretation |
|---|---|---|
| Null Hypothesis (H₀) | The difference between the two methods is outside the equivalence margin (i.e., μ₠- μ₂ ≤ -Δ OR μ₠- μ₂ ≥ +Δ) | |
| Alternative Hypothesis (Hâ‚) | The difference between the two methods is within the equivalence margin (i.e., -Δ < μ₠- μ₂ < +Δ) | |
| First One-Sided Test | t₠= (X̄ - (-Δ)) / (s/√n) | Tests if the difference is significantly greater than the lower margin (-Δ) |
| Second One-Sided Test | t₂ = (+Δ - X̄) / (s/√n) | Tests if the difference is significantly less than the upper margin (+Δ) |
| Decision Rule | If p-valueâ‚ < 0.05 AND p-valueâ‚‚ < 0.05 | Reject Hâ‚€ and conclude equivalence |
Visualization of the TOST Outcome
The result of a TOST analysis is best interpreted using confidence intervals. For equivalence to be concluded, the entire confidence interval for the mean difference between the two methods must lie entirely within the equivalence margin [-Δ, +Δ] [73].
Diagram 2: TOST Outcome Interpretation
The Scientist's Toolkit: Essential Reagents and Materials
Successful execution of a bioanalytical equivalency study requires carefully selected and qualified materials. The following table details key research reagent solutions and their critical functions.
Table 3: Essential Research Reagent Solutions for Method Equivalency Studies
| Reagent / Material | Function & Importance | Key Considerations |
|---|---|---|
| Reference Standard | Serves as the benchmark for quantifying the analyte; essential for determining accuracy/bias [75]. | Must be of known identity, purity, and stability. Traceability to a primary reference standard is critical. |
| Control Matrix | The biological fluid (e.g., plasma, serum) free of the analyte, used to prepare calibration standards and QCs [42]. | Should be as similar as possible to the study sample matrix. Source and lot-to-lot variability must be considered. |
| Critical Reagents | Antibodies, enzymes, or other binding molecules specific to ligand binding assays (LBAs) [42]. | Reagent lot changes can significantly impact method performance. Sufficient quantity from a single lot should be secured for the entire study. |
| Stable Isotope Labeled Internal Standard (SIL-IS) | Used in LC-MS/MS assays to correct for variability in sample preparation and ionization efficiency. | Should ideally be the stable isotope-labeled analog of the analyte. Purity and stability must be verified. |
| Mobile Phase Components | The solvent system used to elute analytes from the chromatographic column. | Buffer pH, ionic strength, and organic modifier ratio are critical method parameters. High-purity reagents are required. |
Establishing statistical acceptance criteria for method equivalency is a multifaceted process that integrates regulatory science, analytical chemistry, and robust statistics. Moving from traditional significance testing to a risk-based equivalence testing framework, using tools like the TOST procedure, provides a more scientifically sound and defensible approach. By linking method performance characteristics directly to the product's specification tolerance and its potential impact on OOS rates, scientists can set justified acceptance criteria that truly ensure the method remains fit-for-purpose. As the industry advances under ICH Q14, this lifecycle approach to analytical procedures, with equivalency at its core, will be crucial for ensuring continuous product quality and facilitating efficient regulatory compliance.
The Role of Intermediate Precision (Ruggedness) in Demonstrating Reproducibility
In the pharmaceutical industry, the successful transfer of bioanalytical methods for chromatographic assays relies on demonstrating that methods produce reliable results across different environments. Intermediate precision (often termed ruggedness) and reproducibility are complementary validation parameters that fulfill this need, assessing a method's variability under different conditions [76] [77]. Intermediate precision measures consistency within a single laboratory under varying conditions, such as different analysts, instruments, or days, serving as a robust predictor of a method's performance in a new setting [78] [79]. Reproducibility, in contrast, confirms this performance between different laboratories [77]. A thorough understanding of intermediate precision is therefore foundational to proving a method is truly reproducible and fit for successful technology transfer.
Defining the Scope: Precision in Method Validation
Precision in analytical method validation is stratified into three tiers to quantify variability at different operational scales. The following table clarifies the distinctions:
| Precision Parameter | Testing Environment | Variables Assessed | Primary Goal |
|---|---|---|---|
| Repeatability [76] [78] | Same lab, short time | Same analyst, instrument, and conditions | Establish the best-case scenario, or minimal variability, of the method. |
| Intermediate Precision (Ruggedness) [76] [77] [80] | Same lab, extended time | Different analysts, instruments, days, reagent batches, etc. | Evaluate the method's real-world robustness and consistency under expected within-lab variations. |
| Reproducibility [76] [77] | Different laboratories | Different labs, equipment, analysts, and environmental conditions | Demonstrate method transferability and global robustness for collaborative studies. |
The relationship between these concepts and their role in method transfer can be visualized as a reliability cascade.
Experimental Protocol for Assessing Intermediate Precision
A well-designed intermediate precision study is critical for providing conclusive evidence of a method's ruggedness. The following workflow outlines a comprehensive, risk-based approach.
Step 1: Risk Assessment and Experimental Design
Before experimentation, use risk assessment tools like Failure Mode and Effects Analysis (FMEA) and cause-and-effect (fishbone) diagrams to identify "noise factors" most likely to impact method results [81]. These typically include the analyst, HPLC instrument, day, column batch, and reagent lots. The experimental design should then deliberately vary these high-risk factors. A full or partial factorial design is often employed to efficiently study their effects [81] [80].
Step 2: Sample Preparation and Analysis
Prepare samples as per the analytical procedure. The ICH guideline recommends data from a minimum of nine determinations over a minimum of three concentration levels covering the specified range (e.g., 80%, 100%, 120% of target), or a minimum of six determinations at 100% of the test concentration [76]. These analyses are then conducted across the varied conditions defined in the design (e.g., by two analysts using two different HPLC systems over several days) [76] [80].
Step 3: Data Analysis and Interpretation
While the relative standard deviation (%RSD) of all results is a common metric, Analysis of Variance (ANOVA) is a more powerful statistical tool for intermediate precision [80]. ANOVA separates the total variability in the data into components, such as:
- Variance within runs (repeatability)
- Variance between analysts, instruments, or days (contributors to intermediate precision)
This allows for a precise estimate of intermediate precision standard deviation: σIP = √(σ²within-run + σ²between-run) [79]. The resulting %RSD from the overall data or the ANOVA model is then compared against pre-defined acceptance criteria. For assay methods, an RSD of ≤ 2.0% is typically expected for the major analyte, while for impurities, 5-10% RSD might be acceptable for low-level components [80].
Case Study Data: HPLC Assay Intermediate Precision
The following table summarizes representative data from a simulated intermediate precision study for an Active Pharmaceutical Ingredient (API) assay, comparing the overall %RSD approach with an ANOVA-based analysis.
| Statistical Metric | Analyst 1 (HPLC 1) | Analyst 2 (HPLC 2) | Combined Data (Overall) |
|---|---|---|---|
| Mean AUC (mV*sec) | 1826.15 | 1901.73 | 1856.47 |
| Standard Deviation (SD) | 19.57 | 14.70 | 36.88 |
| %RSD | 1.07% | 0.77% | 1.99% |
| ANOVA Outcome | - | - | Significant difference (p < 0.05) between means |
| Post-hoc Test (Tukey) | - | - | Analyst 2/HPLC 2 gives significantly higher results |
Source: Adapted from a case study on ANOVA application [80].
The overall %RSD of 1.99% suggests the method passes a typical ≤2% criterion. However, ANOVA reveals a systematic bias between the analysts or instruments, indicating that the method is susceptible to a specific operational factor. This finding, which would be missed by a simple %RSD calculation, is critical for troubleshooting and ensuring the method is truly rugged before transfer.
The Scientist's Toolkit: Essential Reagents and Materials
The following reagents and materials are critical for conducting a rigorous intermediate precision study for a chromatographic bioanalytical method.
| Item | Function in Intermediate Precision Study |
|---|---|
| Well-Characterized Reference Standard [82] | Serves as the benchmark for preparing calibration standards and spiked samples to ensure accuracy and linearity across all testing conditions. |
| Different Batches of Chromatographic Columns [81] | Used to evaluate the method's sensitivity to variations in stationary phase chemistry, a common source of variability. |
| Multiple Qualified Analysts [76] [77] | Essential for introducing operator-to-operator variability, assessing differences in sample preparation technique and instrument operation. |
| High-Purity Solvents and Reagents | Different lots are intentionally used to challenge the method's consistency against normal supply variations [81]. |
| Multiple, Calibrated HPLC/UPLC Systems [76] [80] | Critical for assessing the impact of instrument-to-instrument variability on retention time, peak area, and detection sensitivity. |
Intermediate precision is the critical bridge between idealized repeatability and full-scale reproducibility. A rigorous assessment of intermediate precision, employing risk-based experimental design and robust statistical analysis like ANOVA, provides deep insight into a method's real-world behavior. This process does not merely fulfill a regulatory requirement, it actively de-risks the method transfer process by building confidence that the method will perform consistently in any qualified laboratory's hands, thereby ensuring the continued reliability of data supporting drug development and quality control.
In both computational modeling and pharmaceutical laboratory science, validation serves as the critical bridge between method development and reliable real-world application. In machine learning, cross-validation techniques provide robust estimates of model performance on unseen data, guarding against the pitfalls of overfitting. A parallel challenge exists in the bioanalytical laboratory, where methods for chromatographic assays must be rigorously validated and transferred between sites to ensure consistent, reliable results in drug development. This guide explores this conceptual synergy, comparing cross-validation (CV) techniques used for machine learning models with method validation and transfer processes used for bioanalytical assays, with a specific focus on chromatographic applications in pharmaceutical research.
The fundamental principle connecting these domains is the need to demonstrate reliability through structured testing protocols. Just as k-fold cross-validation assesses a model's generalizability across different data subsets, comparative testing in method transfer evaluates an analytical method's consistency across different laboratories, instruments, and analysts. Both processes aim to provide statistical confidence in performance, whether for predictive accuracy or measurement precision.
Cross-Validation Techniques: A Machine Learning Toolkit
Cross-validation is a cornerstone of machine learning model evaluation, with several techniques offering different trade-offs between bias, variance, and computational cost [83].
Core Cross-Validation Methods
K-Fold Cross Validation: This method partitions the dataset into k equal-sized folds. The model is trained on k-1 folds and tested on the remaining fold, repeating this process k times, each time with a different fold as the test set [83]. The final performance metric is the average across all k iterations. A common choice is k=10, as lower values can increase bias, while higher values approach the computational intensity of Leave-One-Out Cross Validation [83].
Leave-One-Out Cross Validation (LOOCV): A special case of k-fold CV where k equals the number of data points. The model is trained on all data except one single point, which is used for testing, repeating this for every data point [83]. While this approach utilizes maximum data for training (low bias), it can produce high variance estimates, particularly with outliers, and becomes computationally prohibitive with large datasets [83] [84].
Stratified Cross-Validation: This technique preserves the original class distribution within each fold, making it particularly valuable for imbalanced datasets [83]. By ensuring each fold represents the overall population proportions, it provides more reliable performance estimates for classification tasks on skewed data distributions.
Holdout Validation: The simplest approach, involving a single split of data into training and testing sets, typically using 50-80% for training and the remainder for testing [83]. While computationally efficient, this method's performance estimates can vary significantly based on a single, potentially lucky or unlucky, data partition.
Specialized Cross-Validation Approaches
Time Series Cross-Validation: For temporal data, standard random splitting is inappropriate. Approaches like
hv-block CV use rolling windows of consecutive observations for validation, respecting the temporal ordering of data points [85]. The size of the validation window impacts model selection performance, with unequal validation set sizes sometimes offering improvements over equal-sized blocks in finite samples [85].Cluster-Based Cross-Validation: This technique uses clustering algorithms to create folds, aiming to ensure each fold adequately represents the dataset's underlying structure [86]. A hybrid approach combining Mini-Batch K-Means with class stratification has shown promise for balanced datasets, though traditional stratified cross-validation remains superior for imbalanced data [86].
Table 1: Comparison of Common Cross-Validation Techniques
| Technique | Key Mechanism | Best Use Cases | Advantages | Disadvantages |
|---|---|---|---|---|
| K-Fold | Splits data into k equal folds | Small to medium datasets [83] | Balanced bias-variance tradeoff | Computationally intensive for large k |
| LOOCV | Uses single sample as test set | Very small datasets [83] | Low bias, uses all data | High variance, computationally expensive |
| Stratified K-Fold | Preserves class distribution in folds | Imbalanced datasets [83] | Better representation of minority classes | Added complexity |
| Holdout | Single train-test split | Very large datasets, quick evaluation [83] | Fast execution | High variance in estimates |
| Time Series CV | Uses consecutive observation blocks | Temporal data [85] | Respects data chronology | Complex implementation |
Laboratory Method Validation: Bioanalytical Framework
In pharmaceutical development, bioanalytical method validation establishes that a quantitative analytical method is suitable for its intended purpose, with method transfer ensuring consistency when methods move between laboratories.
Method Transfer Approaches
Method transfer is defined as "a specific activity which allows the implementation of an existing analytical method in another laboratory" [42]. The Global Bioanalytical Consortium identifies several transfer strategies:
Comparative Testing: The most prevalent approach, where both originating and receiving laboratories test identical sample batches using a predefined protocol with specific acceptance criteria [42] [6].
Covalidation: When multiple laboratories must perform GMP testing, the receiving laboratory participates as part of the validation team, conducting intermediate precision experiments to generate reproducibility data [6].
Revalidation: Applied when the originating laboratory is unavailable, this risk-based approach determines which aspects of the original validation need repetition by the receiving laboratory [6].
Transfer Waiver: Permitted when the receiving laboratory has substantial experience with the procedure, or when the method is already specified in recognized pharmacopeia, typically requiring only verification [6].
Validation Levels and Requirements
The extent of validation required depends on the transfer context and method type:
Internal Transfer (within same organization with shared systems): For chromatographic assays, this requires minimum two sets of accuracy and precision data over two days with freshly prepared calibration standards, including lower limit of quantification (LLOQ) quality controls [42]. For ligand binding assays with shared critical reagents, four inter-assay accuracy and precision runs on different days are needed, including QCs at LLOQ and ULOQ [42].
External Transfer (between different organizations): Requires full validation including accuracy, precision, benchtop stability, freeze-thaw stability, and extract stability where appropriate [42]. Long-term stability data may be referenced from the originating laboratory if sufficient for the expected sample storage period.
Partial Validation: Applied when modifying a previously validated method, ranging from limited testing to nearly full validation based on a risk assessment of the change's impact [42].
Table 2: Method Transfer Requirements for Chromatographic Assays
| Transfer Type | Accuracy & Precision | LLOQ QC | ULOQ QC | Stability Tests | Additional Tests |
|---|---|---|---|---|---|
| Internal Transfer | 2 runs over 2 days [42] | Required [42] | Not required [42] | Not required | None |
| External Transfer | Full validation [42] | Required | Required | Benchtop, freeze-thaw, extract [42] | Specificity, recovery |
| Partial Validation | Based on risk assessment [42] | Situation-dependent | Situation-dependent | Based on modification impact [42] | Based on risk |
Experimental Protocols and Data
Cross-Validation Experimental Protocol
A typical k-fold cross-validation experiment follows this workflow [83]:
Dataset Preparation: Load and preprocess data. For the Iris dataset example (150 samples, 3 classes), features are standardized and labels encoded.
Model Initialization: Select algorithms for evaluation (e.g., Support Vector Machine with linear kernel, Logistic Regression, Random Forest).
Fold Generation: Configure k-fold splitting (typically k=5 or 10), with optional shuffling and stratification.
Iterative Training/Validation: For each fold:
- Train model on k-1 folds
- Validate on the held-out fold
- Record performance metrics (accuracy, precision, recall, F1-score)
Performance Aggregation: Calculate mean and standard deviation of metrics across all folds.
Python implementation for k-fold CV using scikit-learn appears as follows [83]:
Method Transfer Experimental Protocol
For chromatographic method transfer, a typical comparative testing protocol includes [42]:
Pre-Transfer Preparation:
- Document the validated method in detail
- Identify and address facility/equipment differences
- Ensure critical reagents are available and qualified
- Develop transfer protocol with acceptance criteria
Experimental Execution:
- Prepare calibration standards and quality control samples
- Both laboratories analyze identical sample sets in replicates
- Conduct analysis over multiple days with different analysts
Data Analysis and Comparison:
- Calculate accuracy (% nominal) and precision (%CV) for QCs
- Compare results between laboratories using statistical tests
- Evaluate against predefined acceptance criteria
Acceptance Criteria (example for chromatographic assays):
- Accuracy: Within ±15% of nominal value (±20% at LLOQ)
- Precision: ≤15% CV (≤20% at LLOQ)
- No significant difference between laboratories by statistical testing
Experimental Data on Cross-Validation Performance
Recent research highlights important considerations for cross-validation application:
Statistical Flaws in Model Comparison: A 2025 study demonstrated that comparing models using paired t-tests on CV accuracy scores can be fundamentally flawed, as the outcome significantly depends on CV setup (number of folds and repetitions) [87]. Despite applying classifiers with identical predictive power, the likelihood of detecting "significant" differences increased with more folds and repetitions, creating potential for p-hacking.
LOOCV in Designed Experiments: Contrary to traditional warnings, empirical evidence suggests leave-one-out cross-validation can be useful for analyzing small, structured experiments, particularly in response surface settings where prediction is primary and screening where factor selection matters [88].
Stratified CV for Imbalanced Data: On imbalanced datasets, traditional stratified cross-validation consistently outperforms cluster-based alternatives, showing lower bias, variance, and computational cost [86].
Table 3: Cross-Validation Performance Comparison Across Datasets
| Dataset Characteristics | Recommended CV Technique | Reported Accuracy | Variance | Computational Efficiency |
|---|---|---|---|---|
| Balanced datasets | Mini Batch K-Means with stratification [86] | High | Low | Moderate |
| Imbalanced datasets | Traditional Stratified CV [86] | High | Low | High |
| Small, structured designs | LOOCV [88] | Context-dependent | Context-dependent | Low for small N |
| Neuroimaging data (N<1000) | K-fold CV [87] | Dependent on K and M repetitions | Dependent on K and M repetitions | Moderate |
Visualization of Workflows
Cross-Validation to Method Transfer Conceptual Bridge
The following diagram illustrates the conceptual parallels between machine learning validation and bioanalytical method transfer:
K-Fold Cross-Validation Workflow
The mechanics of k-fold cross-validation (with k=5) are visualized below:
Essential Research Reagent Solutions
Successful implementation of both computational and laboratory validation requires specific tools and reagents. The following table details key components for these workflows:
Table 4: Essential Research Reagents and Tools
| Item | Function | Application Context |
|---|---|---|
| scikit-learn Library | Provides cross-validation implementations | Machine Learning [83] |
| Calibration Standards | Establish analytical response relationship | Chromatographic Methods [42] |
| Quality Control Samples | Monitor method accuracy and precision | Bioanalytical Validation [42] |
| Critical Reagents | Specific antibodies, enzymes, or binding agents | Ligand Binding Assays [42] |
| Stratified K-Fold Splitter | Maintains class distribution in data splits | Imbalanced Classification [83] [86] |
| Reference Standards | Certified materials for method qualification | Bioanalytical Method Transfer [6] |
This comparison reveals a fundamental unity in validation philosophy across computational and laboratory domains. Both fields face similar challenges: ensuring reliability, demonstrating generalizability across different contexts (data subsets or laboratory environments), and providing statistical evidence of performance.
The cross-pollination of ideas between these fields offers promising directions for future research. Machine learning approaches, particularly around stratified sampling and cluster-based validation, could inform more sophisticated method transfer strategies in bioanalysis. Conversely, the rigorous regulatory framework governing bioanalytical method validation may offer insights for standardizing machine learning validation practices, particularly in high-stakes applications like healthcare.
As both fields continue to evolve, the shared emphasis on robust validation methodologies will remain essential for scientific progress and practical application. By recognizing these connections, researchers in both domains can leverage insights from parallel fields to strengthen their own validation frameworks.
Generating the Final Transfer Report and Documenting Success
This guide objectively compares the performance of a new bioanalytical chromatographic assay against established alternatives, providing a framework for documenting a successful method transfer within pharmaceutical research and development.
Experimental Design for Method Comparison
A rigorous method comparison study is the foundation of a reliable transfer report. The goal is to assess whether the new (transferee) method and the established (transferor) method can be used interchangeably without affecting patient results or medical decisions [89].
Key design considerations include [89]:
- Sample Size: A minimum of 40, and preferably 100, patient samples should be used to ensure statistical power and identify potential errors from interferences or sample matrix effects.
- Measurement Range: Samples must cover the entire clinically meaningful measurement range to evaluate method performance across all relevant concentrations.
- Replication: Duplicate measurements for both methods are recommended to minimize the effects of random variation.
- Sample Handling: Analysis should be performed within a short time frame (e.g., 2 hours) and on the day of blood sampling to ensure sample stability. Measurements should be carried out over multiple days (at least 5) and multiple runs to mimic real-world laboratory conditions.
The table below outlines the core parameters for a method comparison study.
Table 1: Experimental Design Parameters for Method Transfer
| Parameter | Specification | Rationale |
|---|---|---|
| Sample Number | Minimum 40, preferably 100 | Provides sufficient statistical power and identifies matrix effects [89]. |
| Concentration Range | Cover clinically reportable range | Assesses method performance across all relevant levels [89]. |
| Replication | Duplicate measurements per method | Minimizes the impact of random analytical variation [89]. |
| Analysis Duration | At least 5 days, multiple runs | Captures inter-day precision and mimics real-world operational conditions [89]. |
| Sample Age | Analyze within stability period (e.g., 2 hours) | Ensures sample integrity and prevents bias due to degradation [89]. |
Statistical Protocols and Data Analysis
The selection of appropriate statistical tests is critical. Commonly misused techniques, such as correlation analysis and t-tests, are inadequate for determining method comparability.
- Correlation vs. Bias: Correlation analysis (e.g., Pearson's r) measures the strength of a linear relationship between two methods but cannot detect constant or proportional bias. Two methods can be perfectly correlated yet produce vastly different absolute values [89].
- Limitations of t-test: A paired t-test may fail to detect a clinically significant difference if the sample size is too small, or it may flag a statistically significant but clinically irrelevant difference if the sample size is very large [89].
The recommended data analysis workflow involves graphical exploration followed by robust regression techniques.
Graphical Data Presentation
Visualization is the first and essential step in data analysis.
- Scatter Plots: A scatter plot displays paired measurements, with the reference method on the x-axis and the comparison method on the y-axis. This helps visualize the variability and relationship across the measurement range. Gaps in the data range, as shown in Figure 2b of the search results, indicate an invalid experiment that requires additional measurements [89].
- Difference Plots (Bland-Altman): This plot graphs the differences between the two methods (y-axis) against the average of the two methods (x-axis). It is the most appropriate tool for assessing agreement and identifying any systematic bias (constant or proportional) across the concentration range [89].
The following diagram illustrates the logical workflow for the statistical analysis of method comparison data.
Quantitative Evaluation Metrics
A benchmarking study should define key quantitative performance metrics a priori [90]. For method transfer, the primary metric is bias. The acceptable bias should be defined before the experiment based on one of three models: the effect on clinical outcomes, biological variation of the measurand, or state-of-the-art performance [89].
Table 2: Key Quantitative Metrics for Method Comparison
| Metric | Calculation | Interpretation |
|---|---|---|
| Mean Bias | Average of differences (Method New - Method Old) | Estimates the constant systematic error between methods. |
| Proportional Bias | Slope from regression analysis - 1 | Indicates a concentration-dependent difference between methods. |
| Standard Deviation of Differences | SD of the differences between methods | Measures the random dispersion of differences around the mean bias. |
| Limits of Agreement | Mean Bias ± 1.96 * SD of Differences | Defines the interval where 95% of differences between the two methods are expected to lie. |
Performance Benchmarking Against Alternatives
A neutral benchmarking study should be as comprehensive as possible, comparing the new method against all relevant alternatives. The selection of methods should be justified, for example, by including current best-performing methods, a simple baseline method, and widely used methods [90]. The results should be summarized to provide clear guidelines for users.
Table 3: Hypothetical Performance Comparison of Chromatographic Assays
| Method | Accuracy (% Nominal) | Precision (%RSD) | Runtime (min) | Linearity (R²) | Key Advantage | Key Limitation |
|---|---|---|---|---|---|---|
| New Transferee Method (HPLC-MS/MS) | 98.5 | 4.2 | 8.5 | 0.998 | High sensitivity and specificity | Requires expensive instrumentation |
| Established Reference Method (HPLC-UV) | 101.2 | 6.8 | 12.0 | 0.995 | Robust and widely available | Lower specificity in complex matrices |
| Alternative Method (UPLC-UV) | 99.8 | 5.1 | 5.0 | 0.997 | Very fast analysis | Higher column backpressure |
This table presents hypothetical experimental data for illustrative purposes.
In this hypothetical comparison, the new HPLC-MS/MS method demonstrates superior precision and good accuracy compared to the established HPLC-UV method, while the UPLC-UV method offers the fastest analysis time.
The Scientist's Toolkit: Research Reagent Solutions
The reliability of a bioanalytical method depends on the quality of its core components. The following table details essential materials and their functions in a chromatographic assay.
Table 4: Essential Reagents and Materials for Chromatographic Assays
| Item | Function & Importance | Example / Specification |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for quantifying the analyte; its purity directly impacts accuracy. | Certified Reference Material (CRM) with >98% purity. |
| Stable Isotope-Labeled Internal Standard (SIL-IS) | Corrects for sample preparation losses and matrix effects during MS analysis, improving precision and accuracy. | Deuterated or 13C-labeled analog of the analyte. |
| Mass-Spectrometry Grade Solvents | Minimize chemical noise and ion suppression in the mass spectrometer, enhancing signal-to-noise ratio. | LC-MS grade Acetonitrile and Methanol. |
| High-Purity Mobile Phase Additives | Facilitate efficient chromatographic separation and optimal ionization; impurities can cause signal suppression. | Optima LC-MS Grade Formic Acid or Ammonium Acetate. |
| Protein Precipitation Solvent | Removes proteins from biological samples (e.g., plasma), clarifying the sample and protecting the analytical column. | Cold Acetonitrile, often in a 3:1 (v/v) ratio to sample. |
| Solid Phase Extraction (SPE) Cartridges | Selectively isolate and concentrate the analyte from a complex biological matrix, reducing background interference. | Mixed-mode C8 or polymeric sorbents. |
Conclusion
Successful bioanalytical method transfer is not a single event but a critical, structured process within the method lifecycle that ensures data reliability and regulatory compliance across laboratories. By mastering the foundational principles, selecting the appropriate transfer strategy—be it comparative testing for complex methods or covalidation for accelerated timelines—and proactively addressing troubleshooting and validation challenges, organizations can significantly de-risk technology transfer. The future of method transfer points towards greater integration of quality-by-design (QbD) principles, increased harmonization of global regulatory standards, and the adoption of more efficient models like covalidation to support the rapid development of advanced therapies. A rigorous, well-documented transfer process is ultimately foundational to delivering safe and effective medicines to the market.
References
- 1. Analytical Method Transfer in Pharmaceuticals | AMT ... [https://www.pharmaguideline.com/2025/09/analytical-method-transfer-in-pharmaceuticals.html]
- 2. Analytical Method Transfer Between Laboratories [https://www.labmanager.com/method-transfer-between-laboratories-challenges-and-solutions-34250]
- 3. Bioanalytical method transfer considerations of ... [https://pubmed.ncbi.nlm.nih.gov/27277876/]
- 4. Types of transfer and transfer strategy - Lösungsfabrik [https://mpl.loesungsfabrik.de/en/q-a/method-transfers-good-to-know/types-of-transfer-and-transfer-strategy]
- 5. Analytical Method Transfer Checklist [https://www.propharmagroup.com/thought-leadership/how-conduct-analytical-method-transfer]
- 6. CRO | Bioanalysis laboratory | Method Development & Transfer [https://www.biotrial.com/solutions-services/bioanalysis/method-development-method-transfer/]
- 7. Comparison of Analytical Procedures in Method Transfer ... [https://pubmed.ncbi.nlm.nih.gov/37468665/]
- 8. ICH Q14 and the Paradigm Shift in Pharmaceutical Analytics [https://www.gmp-journal.com/current-articles/details/ich-q14-and-the-paradigm-shift-in-pharmaceutical-analytics.html]
- 9. Methods on the Move: Addressing Method Transfer ... [https://www.bioprocessintl.com/cmc-forums/methods-on-the-move-addressing-method-transfer-challenges-for-the-biopharmaceutical-industry]
- 10. Analytical Methodology Transfer [https://www.sciencedirect.com/science/article/abs/pii/S0149639501800167]
- 11. Best practices for analytical method transfers [https://medfilesgroup.com/best-practices-for-analytical-method-transfers/]
- 12. Method Transfer [https://www.eurofins.com/biopharma-services/product-testing/services/biopharma-product-testing-services/method-development/method-transfer/]
- 13. Defining Clear Roles and Responsibilities in the Lab [https://labmanageracademy.com/blog/defining-clear-roles-and-responsibilities-in-the-lab]
- 14. Comparison of multiple bioanalytical assay platforms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11389733/]
- 15. Analytical Method Transfer [https://www.chromatographyonline.com/view/analytical-method-transfer-1]
- 16. Bioanalytical method transfer considerations of ... [https://www.bioanalysis-zone.com/bioanalytical-method-transfer-considerations-chromatographic-based-assays/]
- 17. The Impact of Technological Advances on Generic Drug ... [https://www.drugpatentwatch.com/blog/the-impact-of-technological-advances-on-generic-drug-development/?srsltid=AfmBOorNvif5-cxeHltFtRsdPAxuH9yg5ULvn1EfUZVW0zIGcWTXDCls]
- 18. Contract Manufacturing of Medical Devices [https://amt-mat.com/a-deep-dive-into-contract-manufacturing-of-medical-devices/]
- 19. Chromatography 2025: The Trends Transforming ... [https://www.sepscience.com/chromatography-2025-the-trends-transforming-laboratories-11149]
- 20. Innovations in Liquid Chromatography: 2025 HPLC ... [https://www.chromatographyonline.com/view/innovations-in-liquid-chromatography-2025-hplc-column-and-accessories-review]
- 21. FDA Finalizes Guidance On The Advanced Manufacturing ... [https://www.cellandgene.com/doc/fda-finalizes-guidance-on-the-advanced-manufacturing-technologies-designation-program-0001]
- 22. U.S. FDA Publishes Final Guidance and Incentive ... [https://www.sidley.com/en/insights/newsupdates/2025/01/us-fda-final-guidance-and-incentive-designations-for-pharma-manufacturers-using-amts]
- 23. Comparison of VOC measurements made by PTR-MS, ... [https://amt.copernicus.org/articles/11/141/2018/]
- 24. M10 Bioanalytical Method Validation and Study Sample ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/m10-bioanalytical-method-validation-and-study-sample-analysis]
- 25. ICH M10 on bioanalytical method validation - Scientific guideline [https://www.ema.europa.eu/en/ich-m10-bioanalytical-method-validation-scientific-guideline]
- 26. Guidances [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidances]
- 27. USP Reference Standards [https://www.usp.org/reference-standards]
- 28. Compliance: Overview | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/compliance-overview]
- 29. Recent FDA Actions Pose Big Changes and Questions for ... [https://www.hklaw.com/en/insights/publications/2025/07/recent-fda-actions-pose-big-changes-and-questions-for-health]
- 30. New USP-NF Publication Model [https://www.uspnf.com/new-usp-nf-publication-model]
- 31. Quality and Regulatory Predictability: Shaping USP ... [https://www.fda.gov/drugs/news-events-human-drugs/quality-and-regulatory-predictability-shaping-usp-standards-12112025]
- 32. Common challenges in bioanalytical method development [https://www.simbecorion.com/common-challenges-in-bioanalytical-method-development/]
- 33. Recent Advances in Bioanalytical Methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12493022/]
- 34. Life Cycle and Quality by Design for Chromatographic ... [https://www.chromatographyonline.com/view/life-cycle-and-quality-design-chromatographic-methods]
- 35. Bioanalytical method revalidation challenges in pharma R&D [https://www.drugdiscoverytrends.com/bridging-bioanalytical-gaps-examining-validation-methods-across-species/]
- 36. Mastering Chromatography Method Transfer in Today's ... [https://www.chromatographyonline.com/view/mastering-chromatography-method-transfer-in-today-s-connected-world]
- 37. Modernizing Method Transfer: How Digital Transformation ... [https://www.sciy.com/en/blog/modernizing-method-transfer.html]
- 38. Strategic Use of Calibration Transfer to Minimize ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708525005965]
- 39. Analysis of Small-Molecule Drugs and Metabolites in... Bioanalytical [https://www.chromatographyonline.com/view/bioanalytical-analysis-of-small-molecule-drugs-and-metabolites-in-physiological-samples-by-lc-ms-part-2-sample-preparation]
- 40. Analytical Method Transfer: Best Practices and Guidelines [https://www.labmanager.com/analytical-method-transfer-best-practices-and-guidelines-34130]
- 41. Covalidation Strategies to Accelerate Analytical Method ... [https://www.pharmtech.com/view/covalidation-strategies-accelerate-analytical-method-transfer-breakthrough-therapies]
- 42. Method Transfer, Partial Validation, and Cross Validation [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389741/]
- 43. Points to Consider in Quality Control Method Validation ... [https://www.bioprocessintl.com/qa-qc/points-to-consider-in-quality-control-method-validation-and-transfer]
- 44. Recent Advances in Bioanalytical Methods for ... [https://link.springer.com/article/10.1208/s12248-025-01115-9]
- 45. Selecting Bioanalytical Assays for FDA Approved Clinical ... [https://www.marinbio.com/company/selecting-bioanalytical-assays-fda-clinical-trials-commercialization/]
- 46. Statistical Assessments of Bioassay Validation Acceptance ... [https://www.bioprocessintl.com/assays/statistical-assessments-of-bioassay-validation-acceptance-criteria]
- 47. Bioanalytical Method Comparison Strategy for Clinical Anti- ... [https://link.springer.com/article/10.1208/s12248-024-00999-3]
- 48. Risk-based approach for the transfer of quantitative methods [https://www.sciencedirect.com/science/article/abs/pii/S0021967307019607]
- 49. HPLC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/high-performance-liquid-chromatography-hplc-support/hplc-troubleshooting.html]
- 50. HPLC Troubleshooting Guide [https://scioninstruments.com/us/blog/hplc-troubleshooting-guide-2/]
- 51. Solving Key Challenges in (Bio)pharmaceutical Analyses [https://www.chromatographyonline.com/view/solving-key-challenges-in-bio-pharmaceutical-analyses]
- 52. Essentials of LC Troubleshooting, VIII: A Deeper Look Into ... [https://www.chromatographyonline.com/view/essentials-of-lc-troubleshooting-viii-a-deeper-look-into-column-efficiency]
- 53. Guidance for robustness/ruggedness tests in method ... [https://www.sciencedirect.com/science/article/abs/pii/S073170850000529X]
- 54. Method Validation and Robustness [https://www.chromatographyonline.com/view/method-validation-and-robustness]
- 55. Bioanalytical chromatographic method validation according to current regulations, with a special focus on the non-well defined parameters limit of quantification, robustness and matrix effect - PubMed [https://pubmed.ncbi.nlm.nih.gov/24794936/]
- 56. Correction of gas chromatography–mass spectrometry long ... [https://www.nature.com/articles/s41598-025-24794-y]
- 57. Optimizing LC‑MS/MS Sensitivity: Strategies to Overcome ... [https://biotech-spain.com/en/articles/optimizing-lc-ms-ms-sensitivity-strategies-to-overcome-ion-suppression-and-boost-robustness-in-bioanalysis/]
- 58. Signal-to-noise ratio [https://en.wikipedia.org/wiki/Signal-to-noise_ratio]
- 59. Assay Method Transfer [https://www.bioagilytix.com/solutions/capabilities/assay-method-transfer/]
- 60. HPLC 2025 Update Day 2: Pharmaceutical Separations ... [https://www.chromatographyonline.com/view/hplc-2025-update-day-2-pharmaceutical-separations-session]
- 61. Matrix Effect Assessment via Matrix Matching Strategy ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025010864]
- 62. Strategies for the assessment of matrix effect in quantitative ... [https://pubmed.ncbi.nlm.nih.gov/12964746/]
- 63. HPLC 2025 Preview: Functionalized Monoliths as ... [https://www.chromatographyonline.com/view/functionalized-monoliths-as-selective-sample-preparation-materials]
- 64. 7 Most Common Bioanalytical Testing Platforms for Small ... [https://labtesting.wuxiapptec.com/2024/01/11/7-most-common-bioanalytical-testing-platforms/]
- 65. LC vs. HPLC vs. UHPLC: Tracing the Evolution of ... [https://www.metwarebio.com/lc-vs-hplc-vs-uhplc-evolution-chromatography/]
- 66. Comparison Techniques for HPLC Column Performance [https://www.chromatographyonline.com/view/comparison-techniques-hplc-column-performance-2]
- 67. The Future of Analytical Labs: Data, Automation, and AI [https://www.labmanager.com/the-future-of-analytical-labs-data-automation-and-ai-34418]
- 68. A Look at Pharmaceutical Analytical Testing [https://www.americanpharmaceuticalreview.com/Featured-Articles/618346-A-Look-at-Pharmaceutical-Analytical-Testing-Drivers-Fueling-a-Booming-Market/]
- 69. 生物分æžæ³•è§„的解读与展望 [http://www.360doc.com/content/20/1106/23/72280700_944507235.shtml]
- 70. 9012 ç”Ÿç‰©æ ·å“定é‡åˆ†æžæ–¹æ³•éªŒè¯æŒ‡å¯¼åŽŸåˆ™- ä¸å›½è¯å…¸ [https://db2.ouryao.com/yd2020/view.php?id=f3fdf42e6a]
- 71. Specification Equivalence: A Practical Approach to Method ... [https://www.pharmtech.com/view/specification-equivalence-a-practical-approach-to-method-and-acceptance-criteria-equivalence]
- 72. A New Era for Analytical Procedure Lifecycle Management [https://synergbiopharma.com/navigating-analytical-method-comparability-and-equivalency-under-ich-q14-a-new-era-for-analytical-procedure-lifecycle-management/]
- 73. Equivalence Testing for Comparability [https://www.biopharminternational.com/view/equivalence-testing-comparability]
- 74. Equivalence Studies in Statistics: Applications, ... [https://www.linkedin.com/pulse/equivalence-studies-statistics-applications-methodologies-r-ri1pc]
- 75. Establishing Acceptance Criteria for Analytical Methods [https://www.biopharminternational.com/view/establishing-acceptance-criteria-analytical-methods]
- 76. Analytical Method Validation: Back to Basics, Part II [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 77. Difference Between Reproducibility And Intermediate ... [https://pharmaguru.co/difference-between-reproducibility-and-intermediate-precision-in-analytical-method-validation/]
- 78. 4.1. Repeatability, intermediate precision and reproducibility [https://sisu.ut.ee/lcms_method_validation/41-precision-trueness-accuracy/]
- 79. Understanding Intermediate Precision Definition - A How ... [https://altabrisagroup.com/intermediate-precision-definition/]
- 80. a robust statistical tool for determining intermediate ... [https://www.pharmabiz.com/PrintArticle.aspx?aid=175226&sid=9]
- 81. Method ruggedness studies incorporating a risk based ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267011009494]
- 82. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 83. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 84. 5 Cross Validation Techniques Explained Visually [https://blog.dailydoseofds.com/p/5-cross-validation-techniques-explained]
- 85. Time series cross validation: A theoretical result and finite ... [https://www.sciencedirect.com/science/article/abs/pii/S0165176523003944]
- 86. Comparing Cluster-Based Cross-Validation Strategies for ... [https://arxiv.org/html/2507.22299v2]
- 87. Statistical variability in comparing accuracy of ... [https://www.nature.com/articles/s41598-025-12026-2]
- 88. The use of cross validation in the analysis of designed ... [https://arxiv.org/abs/2506.14593]
- 89. Statistical analysis in method comparison studies part one [https://acutecaretesting.org/en/articles/statistical-analysis-in-method-comparison-studies-part-one]
- 90. Essential guidelines for computational method benchmarking [https://pmc.ncbi.nlm.nih.gov/articles/PMC6584985/]