Principles of High-Throughput Screening: A Comprehensive Guide for Accelerating Reaction and Drug Discovery
This article provides a comprehensive overview of the core principles and advanced methodologies of High-Throughput Screening (HTS) for reaction and drug discovery.
Principles of High-Throughput Screening: A Comprehensive Guide for Accelerating Reaction and Drug Discovery
Abstract
This article provides a comprehensive overview of the core principles and advanced methodologies of High-Throughput Screening (HTS) for reaction and drug discovery. Tailored for researchers, scientists, and drug development professionals, it covers the foundational concepts of HTS, including automation, miniaturization, and assay design. It delves into diverse screening approaches—from target-based to phenotypic—and offers practical strategies for assay optimization, robust statistical hit selection, and troubleshooting common pitfalls like false positives. Finally, the guide details rigorous hit validation protocols using counter, orthogonal, and comparative assays to ensure the selection of high-quality leads for further development, synthesizing these elements to highlight future directions in the field.
What is High-Throughput Screening? Core Concepts and Evolution
High-Throughput Screening (HTS) is a rapid assessment approach that utilizes robotic, automated, and miniaturized assays to quickly identify novel lead compounds from large libraries of structurally diverse molecules [1]. It represents a foundational methodology in modern drug discovery and reaction research, enabling the testing of thousands to hundreds of thousands of compounds per day to accelerate the identification of promising chemical starting points [2] [1].
Core Principles and Key Aspects of HTS
The power of HTS stems from the integration of several core technological and methodological components. The process is designed to manage immense complexity while delivering reproducible and reliable data.
Automation and Robotics
At the heart of any HTS system is automation. Automated liquid-handling robots are capable of low-volume dispensing of nanoliter aliquots of sample, which minimizes assay setup times and provides accurate, reproducible liquid dispensing [1]. Modern systems are designed for remarkable versatility and reliability, accommodating both cell and biochemical assays and often functioning continuously for 20-30 hours [2]. Precision dispensing technologies, such as acoustic dispensing, ensure highly accurate compound delivery, which is critical for assay performance and data quality [2].
Assay Development and Miniaturization
HTS assays must be robust, reproducible, and sensitive to be effective [1]. A critical aspect of their design is suitability for miniaturization into 96-, 384-, and 1536-well plate formats, which drastically reduces reagent consumption and cost [1]. These assays undergo rigorous validation according to pre-defined statistical concepts to ensure their biological and pharmacological relevance before being deployed in a full-scale screen [1].
Compound Management and Library Design
The quality of an HTS output is intrinsically linked to the quality of the input. Compound libraries are crucial for generating high-quality starting points for drug discovery [2]. These libraries are stored in custom-built facilities with controlled low humidity and ambient temperature to ensure compound integrity [2]. Library design involves careful curation to insure chemical diversity and quality, often judged by filters such as the Rapid Elimination of SWILL (REOS) or Pan-Assay Interference Compounds (PAINS) filters [3]. Typical industrial screening libraries contain 1-5 million compounds, while academic libraries are often around 0.5 million compounds [3].
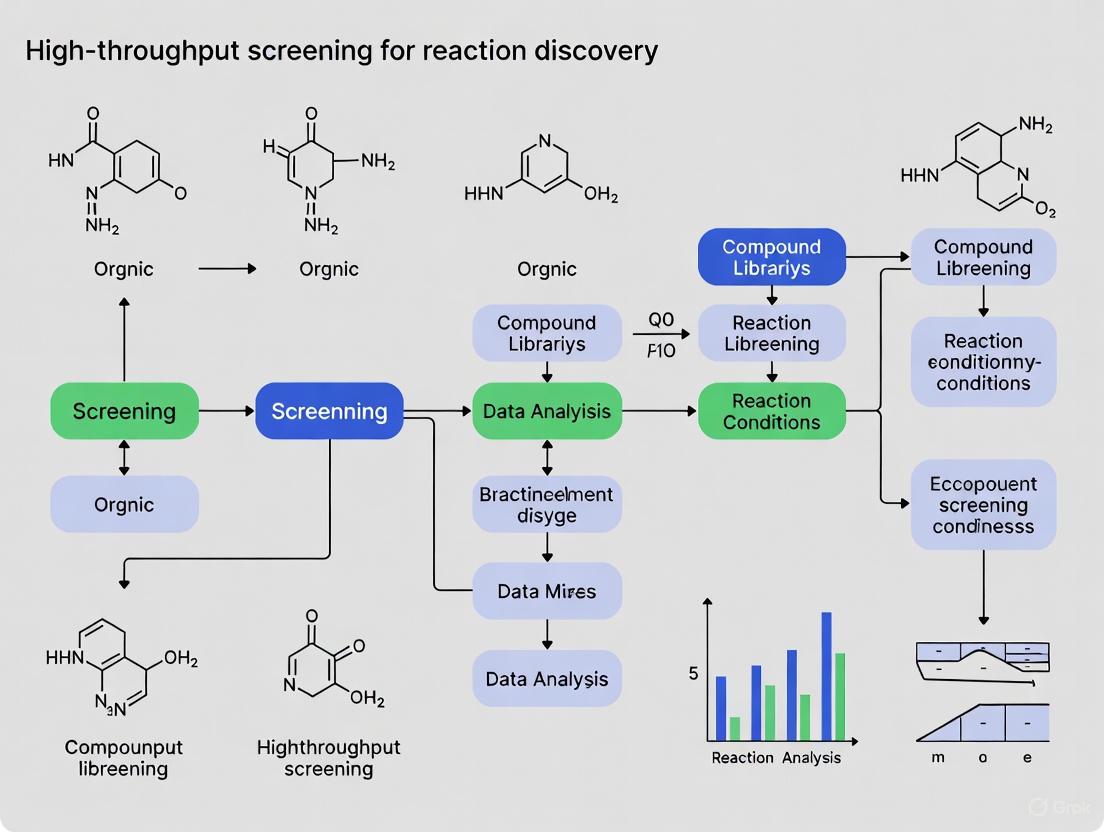
The HTS Workflow: From Assay to Hit
The HTS process is a multi-stage workflow designed to efficiently sift through vast chemical libraries to identify credible "hits" – compounds that show a desired effect on the target. The following diagram illustrates the logical flow and decision points within a standard HTS workflow.
Stages of the HTS Workflow
Assay Development and Validation: The process begins with the development or transfer of a biologically relevant assay [2]. This assay is then meticulously validated in a pilot screen to test automation performance, reproducibility, and to provide an early estimate of hit rates. A common metric for this is the robust Z' factor, which quantifies the assay's quality and suitability for HTS [2].
Primary Screening: In the primary screen, each compound in the library is tested at a single concentration [2]. This phase is designed for speed and efficiency, rapidly surveying the entire chemical library to identify any compound that shows a signal above a predefined threshold.
Hit Confirmation and Cheminformatic Triage: The initial actives from the primary screen are subjected to a first cheminformatic triage [2]. This critical step uses computational tools to identify and filter out compounds likely to be false positives, such as pan-assay interference compounds (PAINS) or promiscuous bioactive compounds [3]. This step requires expertise in medicinal chemistry and cheminformatics to prioritize the more promising chemical matter for follow-up [3].
Hit Profiling and Counter-Screening: The remaining potential hits are then profiled further. This involves testing in counter-screens and orthogonal assays designed to rule out non-specific effects or activity against unrelated targets [2] [1]. Confirmed hits are then advanced to potency assessments, where concentration-response curves (e.g., IC50 or EC50 values) are generated to quantify their activity [2].
Hit Validation and Prioritization: Compounds that advance to this final stage undergo additional quality control processes, such as analytical chemistry checks (e.g., LCMS) to verify compound identity and purity [2]. The final output is a curated list of validated hits with confirmed potency and structure, which serve as the starting points for further medicinal chemistry optimization [2] [3].
Detection Technologies and Data Analysis
HTS assays can be broadly subdivided into biochemical (cell-free) and cell-based methods, each with its own suite of detection technologies [1].
Detection Methodologies
- Biochemical Assays: These typically utilize purified targets like enzymes or receptors [1]. A common example is an enzyme inhibition assay, which might use a peptide substrate coupled to a fluorescent leaving group to quantify activity [1].
- Cell-Based Assays: These use whole cells to evaluate a compound's effect in a more physiologically complex environment. They can measure phenotypes like cell viability, reporter gene expression, or changes in second messengers [1].
- Emerging Methods: Mass spectrometry (MS)-based methods for unlabeled biomolecules are becoming more common, allowing for the direct detection of reaction products [1]. Techniques like Differential Scanning Fluorimetry (DSF) monitor changes in protein thermal stability upon ligand binding, which can indicate direct target engagement [1].
Data Management and Analysis
One of the fundamental challenges in HTS is the generation of false positive data, which can arise from assay interference, chemical reactivity, autofluorescence, or colloidal aggregation [1]. To address this, robust data analysis pipelines are essential.
- Software Platforms: HTS facilities leverage integrated informatics platforms and specialized software like Genedata Screener for processing, managing, and analyzing the large, complex datasets generated [2]. Plate barcodes are typically integrated with sample ID data to guarantee data fidelity [2].
- Triage Methods: Statistical quality control methods and machine learning (ML) models trained on historical HTS data are used to identify and rank HTS output, classifying compounds by their probability of success [1].
Essential Research Reagent Solutions
The following table details key reagents, technologies, and materials essential for executing a successful HTS campaign.
Table 1: Key Research Reagent Solutions and Essential Materials in HTS
| Item/Reagent | Function & Application in HTS |
|---|---|
| LeadFinder Diversity Library [2] | A pre-designed, diverse collection of ~150,000 compounds with lead-like properties, used as a primary source for identifying novel chemical starting points. |
| Microplates (96 to 1536-well) [1] | Miniaturized assay platforms that enable high-density testing and significant reduction in reagent and compound consumption. |
| Fluorescence & Luminescence Kits [1] | Sensitive detection reagents used in a majority of HTS assays due to their high sensitivity, ease of use, and adaptability to automated formats. |
| Echo Acoustic Dispenser [2] | Non-contact liquid handling technology that uses sound energy to transfer nanoliter volumes of compounds with high accuracy and precision. |
| Liquid Chromatography-Mass Spectrometry (LCMS) [2] | An analytical chemistry technique used for rigorous quality control of compound library samples and for confirming the identity and purity of final hit compounds. |
| Genedata Screener Software [2] | A robust data analysis platform specifically designed for processing, managing, and interrogating large, complex HTS datasets. |
| Titian Mosaic SampleBank Software [2] | A compound management system that streamlines the ordering and tracking of assay plates, integrated with automated storage for efficient library management. |
Advanced Concepts: Ultra-High-Throughput Screening (uHTS)
Pushing the boundaries of throughput, Ultra-High-Throughput Screening (uHTS) can achieve throughputs of over 300,000 compounds per day [1]. This requires significant advances in microfluidics and the use of very high-density microwell plates with volumes as low as 1–2 µL [1]. The table below compares the key attributes of HTS and uHTS.
Table 2: Comparison of HTS and uHTS Capabilities [1]
| Attribute | HTS | uHTS | Comments |
|---|---|---|---|
| Speed (assays/day) | < 100,000 | >300,000 | uHTS is significantly faster. |
| Complexity & Cost | High | Significantly Greater | uHTS entails more complex instrumentation and higher costs. |
| Data Analysis Needs | High | Very High | uHTS may require AI to process its larger datasets. |
| Ability to Monitor Multiple Analytes | Limited | Limited | Both require miniaturized, multiplexed sensor systems for this capability. |
| False Positive/Negative Bias | Present | Present | uHTS does not inherently offer enhancements in reducing false results. |
High-Throughput Screening stands as a cornerstone technology in modern reaction discovery and drug development. By integrating automation, miniaturization, sophisticated data analysis, and high-quality compound libraries, HTS enables the systematic and rapid exploration of vast chemical spaces. Its success is not merely a function of scale but depends on a rigorous, multi-stage workflow designed to triage and validate true hits from a sea of potential artifacts. As technologies advance towards uHTS and incorporate more artificial intelligence, the principles of robust assay design, expert chemical triage, and data-quality focus will continue to underpin the effective application of HTS in scientific research.
High-Throughput Screening (HTS) serves as an indispensable engine in modern drug discovery and reaction discovery research, enabling the rapid evaluation of thousands to millions of chemical compounds against biological targets. The power of contemporary HTS rests on three interdependent technological pillars: robotics and automation for precision and reproducibility, miniaturization for efficiency and scale, and sensitive detection for data quality and biological relevance. This whitepaper provides an in-depth technical examination of these core principles, detailing their implementation, synergy, and critical role in advancing discovery research.
Robotics and Automation: The Workhorse of HTS
Robotic systems form the backbone of HTS operations, transforming manual, low-throughput processes into industrialized, automated workflows. The primary objective is unattended, walk-away operation that maximizes throughput while minimizing human error and variability [4].
System Architecture and Key Components
A fully integrated robotic screening system, such as the one implemented at the NIH's Chemical Genomics Center (NCGC), is designed for maximal efficiency and flexibility [4]. Its core components include:
- Robotic Arms: High-precision anthropomorphic arms (e.g., Stäubli) transport plates between system modules.
- Random-Access Plate Storage: Carousels provide on-line storage for thousands of assay and compound plates, enabling true random access for diverse screening protocols.
- Liquid Handling Systems: Multifunctional dispensers using solenoid valve technology handle reagents and compounds with high precision. A 1,536-pin array enables rapid compound transfer for high-density formats.
- Environmental Control: Multiple incubators with independent control of temperature, humidity, and COâ‚‚ are essential for cell-based assays.
- Detection Units: A variety of microplate readers (e.g., ViewLux, EnVision) are integrated to support diverse detection signals.
Enabling Quantitative HTS (qHTS)
The NCGC system was pivotal in pioneering the quantitative HTS (qHTS) paradigm [4]. Unlike traditional single-concentration screening, qHTS tests each compound across a range of seven or more concentrations, generating concentration-response curves (CRCs) for the entire library. This approach:
- Mitigates false positives and negatives common in single-point screens.
- Provides immediate data on compound potency and efficacy.
- Reveals complex biological responses through curve shape analysis. This robust, automated infrastructure has enabled the generation of over 6 million CRCs from more than 120 assays, demonstrating the transformative power of robotics in expanding the scope and quality of screening data [4].
Miniaturization: The Drive for Efficiency
Miniaturization is the practice of downsizing assay volumes to increase throughput and reduce reagent consumption, particularly those that are expensive or precious [5] [6]. It is a continually evolving, historical process that follows the progress of technology [5].
The Evolution of Assay Formats
The transition from 96-well to 384-well and 1536-well plate formats represents the standard trajectory of HTS miniaturization [7] [6]. The 1,536-well format is widely considered the next evolutionary step for primary screening assays, offering a 16-fold reduction in volume and reagent use compared to the 96-well standard [5]. This progression is driven by the need to screen increasingly large compound libraries efficiently.
Benefits and Quantitative Impact
The advantages of miniaturization are both economic and practical, as shown in the table below.
Table 1: Impact of Assay Miniaturization
| Factor | 96-Well Format (Traditional) | 384-Well Format (Miniaturized) | Impact |
|---|---|---|---|
| Cell Usage (Example: iPSC-derived cells) | ~23 million cells for 3,000 data points [6] | ~4.6 million cells for 3,000 data points [6] | ~80% reduction in cell use, saving approximately $6,900 per screen [6] |
| Theoretical Throughput | Baseline | 4x higher than 96-well | Higher data output per unit time |
| Reagent Consumption | High | Significantly lower | Major cost savings, especially for expensive enzymes and antibodies [8] [6] |
Technical Challenges and Solutions
Miniaturization introduces specific technical challenges that require careful management:
- Liquid Handling: Precision is paramount. Issues such as tip clogging, high dead volume, and cross-contamination must be addressed with advanced acoustic dispensing and pressure-driven nanoliter dispensing systems [9].
- Evaporation: Small volumes are highly susceptible to evaporation, leading to edge-effects and variability. Proper use of sealed plates or humidity-controlled environments is critical [6].
- Biology in Small Volumes: Cell-based assays face added challenges in miniaturized formats, including uneven cell distribution, poor viability, and imaging artifacts. These require optimized assay conditions and specialized plates [6].
Sensitive Detection: The Key to Quality Data
Sensitive detection refers to an assay's ability to detect minimal biochemical changes, which directly determines the quality, reproducibility, and cost-effectiveness of a screen [8]. It is the foundation for generating biologically relevant and reliable data.
The Critical Role of Assay Sensitivity
High sensitivity in detection provides multiple interconnected advantages:
- Reduced Reagent Consumption: Sensitive assays can detect product formation at low substrate turnover, allowing researchers to use up to ten times less enzyme than less sensitive methods. This can save tens of thousands of dollars in reagent costs for a single screen [8].
- Accurate Potency Determination (ICâ‚…â‚€): The accurate measurement of a compound's potency relies on keeping the enzyme concentration close to the inhibitor's ICâ‚…â‚€. High-sensitivity assays enable the use of low enzyme concentrations without compromising signal, allowing for accurate determination of sub-nanomolar ICâ‚…â‚€ values, which is vital for ranking compound potency [8].
- Physiologically Relevant Conditions: Sensitive assays enable experiments under initial-velocity conditions (substrate concentrations at or below the enzyme's Km), preserving authentic enzyme kinetics and generating more biologically meaningful data [8].
Table 2: Performance Comparison: Low vs. High-Sensitivity Assays
| Factor | Low-Sensitivity Assay | High-Sensitivity Assay (e.g., Transcreener) |
|---|---|---|
| Enzyme Required | 10 mg | 1 mg |
| Cost per 100,000 wells | Very High | Up to 10x lower |
| Signal-to-Background | Marginal | Excellent (>6:1) |
| Ability to run under Km | Limited | Fully enabled |
| ICâ‚…â‚€ Accuracy | Moderate | High |
Detection Technologies and Metrics
A wide range of fluorescence-based detection technologies are available, each with unique advantages. These include fluorescence polarization (FP), time-resolved FRET (TR-FRET), fluorescence intensity (FI), and AlphaScreen [4] [10]. The performance of these technologies is quantified using key metrics:
- Z'-factor: A statistical measure of assay quality and robustness. Values between 0.5 and 1.0 indicate an excellent assay [8] [7].
- Signal-to-Background (S/B) Ratio: The difference between positive and negative control signals. A higher ratio indicates better detection capability [8].
- Limit of Detection (LOD): The lowest product concentration that can be reliably distinguished from background. For example, advanced HTS methods for virus detection can achieve an LOD of 10â´ genome copies per mL or lower [11].
Integrated Workflow and the Scientist's Toolkit
The three pillars of HTS are not isolated; they function as an integrated system. The following diagram and table outline a generalized HTS workflow and the essential tools that enable it.
Table 3: Essential Research Reagent Solutions for HTS
| Item | Function in HTS |
|---|---|
| Microtiter Plates (384-/1536-well) | The miniaturized vessel for hosting reactions. Choosing the right plate is critical for success, impacting evaporation, optical clarity, and cell adherence [6]. |
| Universal Biochemical Assays (e.g., Transcreener) | Antibody-based detection kits for common products (e.g., ADP, GDP). They offer flexibility across diverse enzyme classes (kinases, GTPases, etc.) and high sensitivity for low reagent consumption [8] [7]. |
| Cell-Based Assay Reagents | Include reporter molecules, viability indicators, and dyes for high-content imaging. Enable phenotypic screening in 2D or 3D culture systems [9] [7]. |
| qHTS Concentration-Response Plates | Pre-spotted compound plates with a serial dilution of each compound. They are fundamental for generating concentration-response curves in primary screening without just-in-time reformatting [4]. |
| Control Compounds | Well-characterized agonists/antagonists and inactive compounds. They are essential for normalizing data (% activity), calculating Z'-factor, and validating assay performance in every plate [12]. |
| Adenosine monophosphate | High-Purity Adenosine 5'-Monophosphate for Research |
| Fortical | Fortical (Calcitonin-salmon) |
The synergy between advanced robotics, relentless miniaturization, and highly sensitive detection defines the cutting edge of high-throughput screening. Robotics provides the unwavering precision and capacity required for complex paradigms like qHTS. Miniaturization delivers the radical efficiency necessary to sustainably leverage biologically relevant but expensive model systems. Finally, sensitive detection underpins the entire endeavor, ensuring that the data generated is of sufficient quality to drive confident decision-making in reaction discovery and drug development. As HTS continues to evolve with AI integration, complex 3D models, and even more sensitive readouts, these three pillars will remain the foundational supports for its progress.
High-Throughput Screening (HTS) and its advanced form, Ultra-High-Throughput Screening (uHTS), represent a foundational paradigm in modern drug discovery and reaction research. This methodology enables the rapid empirical testing of hundreds of thousands of biological or chemical tests per day through integrated automation, miniaturized assays, and sophisticated data analysis [13] [14]. The evolution from simple 96-well plates to uHTS has fundamentally transformed the operational principles of discovery research, shifting the focus from capacity alone to a balanced emphasis on quality, physiological relevance, and cost efficiency [13]. This whitepaper traces the technical history of this evolution, framing it within the core principles that guide contemporary high-throughput reaction discovery research.
The Historical Trajectory of HTS and Microplate Technology
The Origins: Microplate Invention and Early Adoption
The genesis of HTS is inextricably linked to the invention of the microplate. The first 96-well microplate was created in 1951 by Dr. Gyula Takatsy, a Hungarian microbiologist seeking a cost-efficient method to conduct serial dilutions for blood tests during an influenza outbreak [15]. He used calibrated spiral loops and glass plates with wells to perform multiple simultaneous tests. This concept was commercialized in 1953 by American inventor John Liner, who produced the first disposable 96-well plates, founding the company American Linbro and setting the stage for the standardized consumables essential to modern HTS [15]. A significant milestone was reached in 1974 when the microplate was first used for an enzyme-linked immunosorbent assay (ELISA), demonstrating its utility for complex biological assays [15].
The Birth of Modern HTS
The conceptual application of HTS in the pharmaceutical industry began in the mid-1980s. A pivotal development occurred at Pfizer in 1986, where researchers substituted fermentation broths in natural products screening with dimethyl sulfoxide (DMSO) solutions of synthetic compounds, utilizing 96-well plates and reduced assay volumes of 50-100μL [16]. This transition from single test tubes to an array format, coupled with automated liquid handling, marked a fundamental shift. As shown in Table 1, this change dramatically increased throughput while reducing material use and labor [16]. Starting at a capacity of 800 compounds per week in 1986, Pfizer's process reached a steady state of 7,200 compounds per week by 1989 [17] [16]. By 1992, HTS was producing starting points for approximately 40% of Pfizer's discovery portfolio, proving its value as a core discovery engine [17] [16].
Table 1: The HTS Paradigm Shift in the Late 1980s
| Parameter | Traditional Screening | Early HTS |
|---|---|---|
| Format | Single tube | 96-well array |
| Assay Volume | ~1 mL | 50–100 µL |
| Compound Used | 5–10 mg | ~1 µg |
| Compound Source | Dry compounds, custom solutions | Compound file in DMSO solution |
| Throughput | 20–50 compounds/week/lab | 1,000–10,000 compounds/week/lab |
The Push for Higher Throughput and the Rise of uHTS
The 1990s witnessed an accelerated drive for higher throughput, fueled by the sequencing of the human genome and the expansion of corporate compound libraries [13]. The term "Ultra-High-Throughput Screening" was first introduced in a 1994 presentation, and by 1996, 384-well plates were being used in proof-of-principle applications, moving HTS from thousands of compounds per week to thousands of compounds per day [17]. The cut-off between HTS and uHTS is somewhat arbitrary, but uHTS is generally defined by the capacity to generate in excess of 100,000 data points per day [13] [17]. This era saw the development of dedicated uHTS systems, such as the EVOscreen system (Evotek, 1996) and the ANALYST (LJL Biosystems, 1997), which could achieve throughputs of ~70,000 assays per day [17]. By 1998, 384-well plates were widely used, and 1536-well plates were being tested [17]. The subsequent launch of fully integrated platforms, like Aurora Biosciences' system for Merck (2000) and the FLIPR Tetra system for ion channel targets (Molecular Devices, 2004), cemented uHTS as a standard industrial practice [17]. This evolution in throughput is summarized in Table 2.
Table 2: Evolution of Screening Throughput and Miniaturization
| Time Period | Key Development | Typical Throughput | Dominant Microplate Format |
|---|---|---|---|
| Pre-1980s | Manual, tube-based testing | 10-100 compounds/week | Test Tubes |
| Mid-1980s | Birth of HTS with automation | Hundreds-7,000 compounds/week | 96-well |
| Mid-1990s | Adoption of 384-well plates | Tens of thousands of compounds/week | 384-well |
| Late 1990s | Advent of uHTS; 1536-well plates | >100,000 compounds/day | 384-well / 1536-well (emerging) |
| 2000s | Fully integrated robotic uHTS | >1,000,000 compounds/day | 1536-well |
Core Technological Enablers and Methodologies
Assay Formats and Detection Technologies
The success of HTS/uHTS hinges on robust, miniaturizable assay formats. The two primary categories are cell-free (biochemical) and cell-based assays [18].
- Biochemical Assays: These are used to investigate molecular interactions between a target (e.g., an enzyme, receptor) and test compounds. A common format is the competitive displacement fluorescence polarization (FP) assay. For example, in a screen for Bcl-2 family protein inhibitors, a fluorescein-labeled peptide that binds the target protein is used [19]. When bound, the peptide rotates slowly, producing high polarization. If a test compound displaces the peptide, the rotation speed increases, causing a measurable drop in polarization, thus identifying a "hit" [19].
- Cell-Based Assays: These are crucial for understanding cellular processes, transmembrane transport, and cytotoxicity [18] [20]. They allow researchers to investigate whole pathways and phenotypic changes in a more physiologically relevant context. A widely used technology is the FLIPR (Fluorescent Imaging Plate Reader) system, which is particularly adept at measuring fast kinetics in ion channel and GPCR (G-Protein Coupled Receptor) assays by detecting calcium flux or membrane potential changes in real-time [17].
Fluorescence-based techniques remain a primary detection method due to their high sensitivity, diverse range of fluorophores, and compatibility with miniaturization and multiplexing [20]. Luminescence and absorbance are also common readouts.
The Integrated HTS/uHTS Workflow
A modern uHTS campaign is a multi-step, integrated process. The following workflow diagram illustrates the key stages from library management to hit confirmation.
The Scientist's Toolkit: Essential Research Reagent Solutions
The execution of HTS/uHTS relies on a suite of specialized reagents and materials. The following table details key components essential for establishing a robust screening platform.
Table 3: Key Research Reagent Solutions for HTS/uHTS
| Reagent/Material | Function and Role in HTS/uHTS |
|---|---|
| Microplates (96, 384, 1536-well) | The foundational labware for parallel sample processing. Higher density plates (e.g., 1536-well) are critical for uHTS miniaturization [13] [15]. |
| Compound Libraries in DMSO | Standardized collections of small molecules or natural product extracts stored in dimethyl sulfoxide, the universal solvent for HTS. These are the "screening deck" [16] [19]. |
| Fluorescent/Luminescent Probes | Essential reagents for detection. Examples include FITC-labeled peptides for FP assays [19] or dyes for cell viability and caspase activation [20] [19]. |
| Cell Lines (Primary, Immortalized, Stem Cells) | Biological systems for cell-based assays. The trend is toward using more physiologically relevant cells, including stem cell-derived neurons and 3D organoids [18] [20]. |
| Liquid Handling Reagents (Buffers, Enzymes, Substrates) | The core biochemical components of the assay, prepared in bulk and dispensed automatically to initiate reactions [19]. |
| Damascenone | β-Damascenone (2,6,6-Trimethyl-1-crotonyl-1,3-cyclohexadiene) |
| Gomisin A | Gomisin A, MF:C23H28O7, MW:416.5 g/mol |
Contemporary Trends and Future Directions
The field of HTS is currently at a crossroads, with a clear shift from a purely quantitative focus to a qualitative increase in screening content [13]. Key contemporary trends include:
- Quality over Throughput: Greater emphasis is placed on rigorous assay characterization, the use of physiologically relevant models, and early hit validation using orthogonal assay technologies to reduce attrition rates [13].
- The Rise of Phenotypic Screening and 3D Models: There is a growing use of target identification strategies following phenotypic screening and the implementation of more complex screening models, such as three-dimensional (3D) organoids [13] [18]. These 3D models, combined with microfluidic devices, aim to better recapitulate the in vivo microenvironment, narrowing the gap between screening results and clinical outcomes [18].
- Next-Generation Screening Paradigms: Techniques like Quantitative HTS (qHTS), which generates full concentration-response curves for all library compounds, are being adopted to provide richer pharmacological data early in the process [13] [14]. Furthermore, fragment-based screening (FBS) and affinity selection methodologies are being merged with HTS strategies to tackle difficult target classes like protein-protein interactions [13].
- Miniaturization Beyond Microplates: While the trend toward further miniaturization is slowing, advanced platforms like drop-based microfluidics are emerging, enabling millions of reactions in hours using picoliter volumes at a fraction of traditional costs [18] [14].
The journey from the 96-well plate to uHTS represents more than just a history of technological advancement; it reflects an evolving philosophy in reaction discovery research. The initial drive for quantitative increases in throughput has matured into a sophisticated discipline that strategically balances speed, cost, and quality. The core principles of HTS—miniaturization, automation, and parallel processing—remain fundamental, but their application is now more nuanced, project-specific, and integrated with other discovery tools like computational design and fragment-based approaches. As the field continues to evolve with 3D organoid models, microfluidics, and advanced data analytics, HTS/uHTS will undoubtedly remain a cornerstone of biomedical research, continually refining its principles to deliver better chemical starting points for drug discovery and beyond.
High-throughput screening (HTS) represents a fundamental paradigm in modern scientific discovery, enabling the rapid experimental conduct of millions of chemical, genetic, or pharmacological tests [14]. This methodology leverages robotics, sophisticated data processing software, liquid handling devices, and sensitive detectors to identify active compounds, antibodies, or genes that modulate specific biomolecular pathways [14]. Within drug discovery and reaction discovery research, HTS provides the critical starting points for drug design and understanding the interaction roles within biological systems. The efficiency of HTS stems from its highly automated and parallelized approach, with systems capable of testing up to 100,000 compounds per day, and ultra-HTS (uHTS) pushing this capacity beyond 100,000 compounds daily [14]. The core terminology of HTS—encompassing hits, assays, libraries, and hit selection—forms the essential lexicon for researchers and drug development professionals navigating this field. A thorough grasp of these concepts is indispensable for designing effective screening campaigns and interpreting their results within a broader research thesis.
Core Terminology and Definitions
Hits
In HTS, a hit is a compound that exhibits a desired therapeutic or biological activity against a specific target molecule during a screening campaign [21]. Hits are the primary output of the initial screening phase and provide crucial initial information on the relationship between a compound's molecular structure and its biological activity [21]. Following discovery, hits undergo a rigorous confirmation process to verify their activity before advancing to the next stage. It is important to distinguish a "hit" from a "lead" compound. A hit demonstrates confirmed activity in a screening assay, whereas a lead compound is a validated hit that has been further optimized and possesses promising properties for development into a potential drug candidate, including acceptable potency, selectivity, solubility, and metabolic stability [21].
Assays
An assay is the experimental test or method used to measure the effect of compounds on a biological target. In HTS, assays are conducted in microtiter plates featuring grids of small wells, with common formats including 96, 384, 1536, 3456, or 6144 wells [14]. The biological entity under study—such as a protein, cells, or animal embryo—is introduced into the wells, incubated to allow interaction with the test compounds, and then measured for responses using specialized detectors [14]. Assays are designed to be simple, automation-compatible, and suitable for rapid testing. A significant advancement is quantitative HTS (qHTS), which tests compounds at multiple concentrations to generate full concentration-response curves immediately, thereby providing richer data and lower false-positive/negative rates compared to traditional single-concentration HTS [22] [23].
Libraries
A screening library, or compound library, is a curated collection of substances stored in microtiter plates (stock plates) screened against biological targets [14]. These libraries can comprise small molecules of known structure, chemical mixtures, natural product extracts, oligonucleotides, or antibodies [23]. The contents of these libraries are carefully cataloged, and assay plates are created by transferring small liquid volumes from stock plates for experimental use [14]. Libraries serve as the source of chemical diversity for discovering novel active compounds. Beyond chemical libraries, other types include siRNA/shRNA libraries for gene silencing, cDNA libraries for gene overexpression, and protein libraries [24].
Hit Selection
Hit selection is the statistical and analytical process of identifying active compounds (hits) from the vast dataset generated by an HTS campaign [14]. This process involves differentiating true biological signals from background noise and systematic errors. The specific analytical methods depend on whether the screen is conducted with or without replicates. Key metrics used in hit selection include the z-score (for screens without replicates), t-statistic (for screens with replicates), and Strictly Standardized Mean Difference (SSMD) [14]. SSMD is particularly valuable as it directly assesses the size of compound effects and is comparable across experiments [14]. Robust methods accounting for outliers, such as the z*-score and B-score, are also commonly employed [14].
Experimental Protocols and Workflows
Primary Screening Protocol
The primary screening protocol forms the foundational stage of HTS, designed to test all compounds in a library against a target to identify initial hits.
- Assay Plate Preparation: An assay plate is created by transferring nanoliter volumes of compounds from a stock library plate to an empty microtiter plate using robotic liquid handlers [14]. The specific plate format (e.g., 384 or 1536-well) is chosen based on the required throughput and reagent availability.
- Biological Reaction Setup: The biological target (e.g., enzymes, cells) is added to each well of the assay plate in a suitable buffer, often using automated dispensers [14]. Controls are included: positive controls (known activators/inhibitors) and negative controls (no compound or solvent only) are essential for quality control.
- Incubation and Reaction: The assay plate is incubated under optimal conditions (e.g., specific temperature, humidity) for a predetermined time to allow interaction between compounds and the biological target [14].
- Signal Detection: Following incubation, a detection method is applied. This varies by assay design and may involve measuring fluorescence, luminescence, absorbance, or other physical properties using specialized plate readers [23] [24]. The reader outputs a grid of numerical values mapping to the signal from each well.
- Primary Hit Identification: Raw data is processed using hit selection algorithms. For single-concentration screens, simple methods like percent inhibition or z-score are often used initially to flag compounds exhibiting significant activity beyond a predefined threshold [14].
Hit Confirmation and qHTS Protocol
This protocol validates the initial hits and provides quantitative pharmacological data.
- Cherrypicking: Compounds identified as hits in the primary screen are transferred ("cherrypicked") from the stock library into new assay plates for retesting [14].
- Dose-Response Testing (qHTS): In qHTS, cherrypicked hits are tested across a range of concentrations (typically 8-15 points in a serial dilution) instead of a single concentration [22]. This is often performed directly in the primary screen in modern setups.
- Concentration-Response Curve Fitting: The dose-response data for each compound is fitted to a nonlinear model, most commonly the four-parameter Hill equation (Equation 1) [22]: Ri = E0 + (E∞ - E0) / (1 + exp{-h[log Ci - log AC50]}) where Ri is the response at concentration Ci, E0 is the baseline, E∞ is the maximal response, AC50 is the half-maximal effective concentration, and h is the Hill slope [22].
- Hit Confirmation and Prioritization: Compounds that produce robust concentration-response curves, with acceptable estimates for potency (AC50), efficacy (Emax), and curve quality, are confirmed as hits. They are then prioritized for the next stage based on these parameters and early assessment of selectivity and chemical tractability.
Diagram 1: High-Throughput Screening Workflow
Data Analysis and Statistical Methods
Quality Control Metrics
Robust quality control (QC) is critical for ensuring HTS data reliability. Effective QC involves good plate design, selection of effective controls, and development of robust QC metrics [14]. Key metrics for assessing data quality and assay performance include:
Table 1: Key Quality Control Metrics for HTS Data Analysis
| Metric | Formula/Description | Application | Interpretation |
|---|---|---|---|
| Z'-Factor [14] | 1 - (3σpositive + 3σnegative) / |μpositive - μnegative| | Assay Quality | ≥ 0.5: Excellent assay0.5 > Z' > 0: MarginalZ' ≤ 0: Poor assay |
| Signal-to-Background Ratio [14] | μpositive / μnegative | Assay Robustness | Higher values indicate stronger signal detection |
| Signal-to-Noise Ratio [14] | (μpositive - μnegative) / σ_negative | Assay Robustness | Higher values indicate cleaner signal |
| Strictly Standardized Mean Difference (SSMD) [14] | (μpositive - μnegative) / √(σ²positive + σ²negative) | Data Quality | Assesses effect size and degree of differentiation between controls |
Hit Selection Methodologies
Hit selection methodologies vary based on screening design, particularly the presence or absence of replicates.
Table 2: Statistical Methods for Hit Selection in HTS
| Method | Application Context | Key Characteristics | Considerations |
|---|---|---|---|
| z-score [14] | Primary screens (no replicates) | Measures number of standard deviations from the mean; assumes all compounds have same variability as negative reference. | Sensitive to outliers; relies on strong assumptions about data distribution. |
| z*-score [14] | Primary screens (no replicates) | Robust version of z-score; less sensitive to outliers. | More reliable for real-world data with variability. |
| t-statistic [14] | Confirmatory screens (with replicates) | Uses compound-specific variability estimated from replicates. | Suitable with replicates; p-values affected by both sample size and effect size. |
| SSMD [14] | Both with and without replicates (calculations differ) | Directly measures size of compound effect; comparable across experiments. | Preferred for hit selection as it focuses on effect size rather than significance testing. |
| B-score [14] | Primary screens | Robust method that normalizes data for plate-level systematic errors. | Effective for removing spatial artifacts within plates. |
For screens with replicates, SSMD or t-statistics are appropriate as they can leverage compound-specific variability estimates. SSMD is particularly powerful because its population value is comparable across experiments, allowing consistent effect size cutoffs [14]. In qHTS, curve-fitting parameters from the Hill equation (AC50, Emax, Hill coefficient) are used for hit selection and prioritization, though careful attention must be paid to parameter estimate uncertainty, especially when the concentration range does not adequately define asymptotes [22].
Diagram 2: Hit Selection and Prioritization Logic
Essential Research Reagents and Materials
Successful HTS implementation requires specialized materials and reagents designed for automation and miniaturization. The following toolkit details key components essential for establishing a robust HTS platform.
Table 3: The Scientist's Toolkit: Essential Research Reagent Solutions for HTS
| Item | Function/Application | Key Characteristics |
|---|---|---|
| Microtiter Plates [14] | The primary labware for conducting assays in a parallel format. | Available in 96, 384, 1536, 3456, or 6144-well formats; made of optical-grade plastic for sensitive detection. |
| Compound Libraries [14] [23] | Collections of small molecules, natural products, or other chemicals screened for biological activity. | Carefully catalogued in stock plates; contents can be commercially sourced or internally synthesized. |
| Liquid Handling Robots [14] [24] | Automated systems for precise transfer of liquid reagents and compounds. | Enable creation of assay plates from stock plates and addition of biological reagents; critical for reproducibility and throughput. |
| Sensitive Detectors / Plate Readers [14] [23] | Instruments for measuring assay signals from each well in the microtiter plate. | Capable of various detection modes (e.g., fluorescence, luminescence, absorbance); high-speed for processing many plates. |
| Assay Reagents | Biological components and chemicals used to configure the specific test. | Includes purified proteins, enzymes, cell lines, antibodies, fluorescent probes, and substrates specific to the target pathway. |
| qHTS Software [22] | Computational tools for analyzing concentration-response data and curve fitting. | Generate dose-response curves, calculate AC50, Emax, and Hill slope parameters for lead characterization and prioritization. |
The precise understanding of hits, assays, libraries, and hit selection forms the foundation of effective high-throughput screening. These core components create an integrated pipeline that transforms vast compound collections into validated starting points for reaction discovery and drug development. The evolution from traditional HTS to quantitative HTS (qHTS) and the application of robust statistical methods like SSMD have significantly enhanced the reliability and information content of screening data [14] [22]. As HTS technologies continue to advance with ever-greater miniaturization, automation, and computational power, the principles governing these key terminologies remain central to interpreting results and making informed decisions in research. Mastering this vocabulary and the underlying concepts enables scientists to design more effective screens, critically evaluate data quality, and successfully navigate the complex journey from hit identification to lead compound.
High-Throughput Screening (HTS) is an automated, miniaturized approach that enables the rapid assessment of libraries containing thousands to hundreds of thousands of compounds against biological targets [1]. In drug discovery and reaction discovery research, HTS serves as a powerful platform to identify novel lead compounds by rapidly providing valuable cytotoxic, immunological, and phenotypical information [25] [1]. The central workflow encompasses several integrated stages: compound library management, assay development, automated screening execution, and sophisticated data acquisition and analysis. This integrated system allows researchers to quickly identify potential hits (10,000–100,000 compounds per day) and implement "fast to failure" strategies to reject unsuitable candidates as quickly as possible [1]. The following sections provide an in-depth technical examination of each component within this critical pathway, with specific consideration for its application in reaction discovery research.
Compound Management and Library Preparation
Foundation of Screening Operations
An efficient and versatile Compound Management operation is fundamental to the success of all downstream processes in HTS and small molecule lead development [26]. This stage requires reliable yet flexible systems capable of incorporating paradigm changes in screening methodologies. At specialized centers such as the NIH Chemical Genomics Center (NCGC), compound management systems have been uniquely tasked with preparing, storing, registering, and tracking vertically developed plate dilution series (inter-plate titrations) in 384-well format, which are subsequently compressed into 1536-well plates for quantitative HTS (qHTS) applications [26]. This qHTS approach involves assaying complete compound libraries at multiple dilutions to construct full concentration-response profiles, necessitating highly precise compound handling and tracking systems.
Practical Implementation Protocols
For practical implementation, compound libraries are typically prepared in 384-well compound plates ("source plates") [27]. When screening plates are prepared in-house, compounds are generally dissolved in HPLC-grade DMSO or similar solvents at a consistent, high concentration (e.g., 2 mM) [27]. The protocol involves:
- Compound Transfer: Using automated systems such as the BioMek FX pintool to transfer 100 nL of compound from source plates to cell culture plates [27].
- Tool Maintenance: Washing the pintool with solvent and blotting on filter paper three times using a sequence of HPLC grade solvents (DMSO, isopropyl alcohol, methanol) [27].
- Quality Control: Including compounds with known function as additional controls to verify compound transfer efficiency and biological system responsiveness [27].
Automated liquid-handling robots capable of low-volume dispensing of nanoliter aliquots have become essential for minimizing assay setup times while providing accurate and reproducible liquid dispensing [1]. This compound management foundation enables the handling of libraries exceeding 200,000 members as demonstrated in successful screening campaigns [26] [27].
Essential Research Reagent Solutions
Table 1: Key Materials and Equipment for Compound Management and Screening
| Item | Function | Specific Examples |
|---|---|---|
| Automated Liquid Handler | Precise transfer of nanoliter volumes of compounds and reagents [27] | BioMek FX pintool, Labcyte Echo [27] |
| Microplates | Standardized format for miniaturized assays [1] | 384-well and 1536-well plates [26] [27] |
| Plate Washer | Automated aspiration and dispensing for cell washing steps [27] | BioTek ELx405 Plate Washer [27] |
| Reagent Dispenser | Rapid and precise dispensing of reagents to plates [27] | BioTek MicroFlo, Thermo Fisher Multidrop Combi [27] |
| Cell Culture Media | Maintenance and stimulation of cells during screening [27] | RPMI 1640 with FBS and antibiotic-antimycotic [27] |
Assay Development and Experimental Design
Core Principles for Robust Assays
HTS assays must be robust, reproducible, and sensitive to effectively identify true hits amid thousands of data points [1]. The biological and pharmacological relevance of each assay must be rigorously validated, with methods appropriate for miniaturization to reduce reagent consumption and suitable for automation [1]. Contemporary HTS assays typically run in 96-, 384-, and 1536-well formats, utilizing automated liquid handling and signal detection systems that require full process validation according to pre-defined statistical concepts [1]. When adapting the core protocol for different targets, researchers must consider critical parameters including the timing of compound addition relative to stimulus and optimal incubation duration, which must be determined empirically for each biological system [27].
Classification of Screening Assays
HTS assays can be broadly subdivided into two principal categories:
- Biochemical Assays: These typically utilize enzymatic targets and measure changes in enzymatic activity through various detection methods [1]. For instance, HTS methods for novel histone deacetylase (HDAC) inhibitors employ a peptide substrate coupled to a suitable leaving group that allows quantification of the HTS substrate activated by the HDAC enzyme [1].
- Cell-Based Assays: These utilize whole cells to measure phenotypic changes, protein expression, or secretion of biomarkers [25] [27]. For example, a protocol for screening immunomodulatory compounds uses human peripheral blood mononuclear cells (PBMCs) cultured in autologous plasma to model the human immune response, measuring cytokine secretion via AlphaLISA assays and cell surface activation marker expression via flow cytometry [25].
Experimental Design Considerations
When designing a screening campaign, investigators must strategically determine the number of compounds to screen and the number of replicates to include. For flow cytometry-based screens, the protocol is ideal for testing approximately ten to twelve 384-well plates at a time [27]. If two rows and two columns on each edge of the plate are excluded to accommodate controls and minimize edge effects, this allows for 240 test wells per plate, or about 2400 compounds per screen without replicates [27]. Ideally, assays should be performed with three replicates of each plate; however, when screening large compound libraries, replicates may be omitted at the risk of missing potential hits [27]. In such cases, all identified hits must be reanalyzed with three or more replicates at several concentrations for confirmation [27].
Automation and Screening Execution
Integrated Robotic Systems
The execution phase of HTS relies on integrated automation systems that combine robotic liquid handling, plate manipulation, and detection technologies. This automation enables the rapid processing of thousands of samples with minimal manual intervention, significantly reducing human error and increasing reproducibility. Compound management has evolved into a highly automated procedure involving compound storage on miniaturized microwell plates with integrated systems for compound retrieval, nanoliter liquid dispensing, sample solubilization, transfer, and quality control [1]. The precision of these systems is critical, as exemplified by protocols that utilize pintools to transfer 100 nL of compound from source plates to cell culture plates [27].
Detection Technologies and Measurement Approaches
Multiple detection technologies can be employed to measure biological responses in HTS assays:
- Fluorescence-Based Methods: These are among the most common due to their sensitivity, responsiveness, ease of use, and adaptability to HTS formats [1]. For instance, differential scanning fluorimetry (DSF) monitors changes in fluorescence as a function of protein melting temperatures (T
), where ligand binding results in increased T values [1]. - Mass Spectrometry-Based Methods: These approaches for unlabeled biomolecules are becoming more prevalent in HTS, permitting compound screening in both biochemical and cellular settings [1].
- Flow Cytometry: This technology enables quantitative analysis of cell surface protein expression at single-cell resolution in high-throughput formats [27]. The HyperCyt autosampler system, for example, allows rapid sampling from 384-well plates for flow cytometric analysis [27].
Workflow Visualization
The following diagram illustrates the integrated workflow from compound library preparation through data acquisition and hit identification:
HTS Central Workflow from Library to Data
Data Acquisition, Management, and Analysis
Addressing False Positives and Quality Control
One of the most significant challenges in HTS is the generation of false positive data, which can arise from multiple sources including assay interference from chemical reactivity, metal impurities, assay technology limitations, measurement uncertainty, autofluorescence, and colloidal aggregation [1]. To address these issues, several in silico approaches for false positive detection have been developed, generally based on expert rule-based approaches such as pan-assay interferent substructure filters or machine learning models trained on historical HTS data [1]. Statistical quality control methods for outlier detection are essential for addressing HTS variability, encompassing both random and systematic errors [1].
HTS Triage and Hit Prioritization
HTS triage involves the strategic ranking of HTS output into categories based on probability of success: compounds with limited, intermediate, or high potential [1]. This process requires integrated analysis of multiple data parameters, including efficacy, specificity, and cellular toxicity. For example, in a flow cytometry-based screen for PD-L1 modulators, data analysis involves processing through software such as FlowJo or HyperView, followed by statistical analysis in GraphPad Prism to identify significant changes in target expression compared to controls [27]. The application of cheminformatics systems such as Laboratory Information Management Systems (LIMS) is often necessary to manage the substantial data volumes generated [1].
Quantitative Data Parameters
Table 2: Key Quantitative Parameters in HTS Data Analysis
| Parameter | Typical Values/Ranges | Application Context |
|---|---|---|
| Throughput | 10,000–100,000 compounds/day (HTS); >300,000 compounds/day (uHTS) [1] | Screening capacity measurement |
| Assay Formats | 96-, 384-, 1536-well plates [1] | Miniaturization level |
| Volume Dispensing | Nanoliter aliquots [1]; 100 nL compound transfer [27] | Liquid handling precision |
| Incubation Period | 72 hours for PBMC stimulation [25]; 3 days for THP-1 PD-L1 expression [27] | Cellular assay duration |
| Data Quality Threshold | Z' factor > 0.5 [1] | Assay robustness metric |
Advanced Applications and Protocol Adaptations
Specialized Screening Modalities
The core HTS workflow supports various specialized screening modalities with specific protocol adaptations:
- Ultra-High-Throughput Screening (uHTS): This approach achieves throughput of millions of compounds per day through advanced microfluidics and high-density microwell plates with typical volumes of 1–2 µL [1]. The development of miniaturized, multiplexed sensor systems that allow continuous monitoring of parameters like pH and oxygen concentration has addressed previous limitations in monitoring individual microwell environments [1].
- Functional Genomics Screening: HTS is used in functional genomics to identify biological functions of specific genes and metagenes through rapid analysis of large gene sets to identify those affecting specific diseases or biological pathways [1]. This application commonly utilizes RNA sequencing and chromatin immunoprecipitation sequencing with DNA-encoded libraries [1].
- Immunomodulatory Compound Screening: This specialized application involves stimulating human PBMCs for 72 hours and measuring cytokine secretion via AlphaLISA assays alongside cell surface activation marker expression via flow cytometry [25]. This multiplexed readout workflow directly aids in phenotypic identification and discovery of novel immunomodulators and potential vaccine adjuvant candidates [25].
Protocol for Flow Cytometry-Based HTS
The following detailed protocol adapted from Zavareh et al. outlines a specific implementation for high-throughput small molecule screening using flow cytometry analysis of THP-1 cells:
- Plate Preparation: Cell culture microplates (384-well, sterile) are prepared with THP-1 cells suspended in complete media [27].
- Compound Addition: Using a BioMek FX pintool or similar system, transfer 100 nL of compound from source plates to cell culture plates [27].
- Stimulation: Add IFN-γ (or other relevant stimulus) to induce expression of the target protein (e.g., PD-L1) [27].
- Incubation: Incubate plates for three days at 37°C, 5% CO₂ [27].
- Staining: Centrifuge plates, wash cells with FACS buffer, and stain with specific antibodies (e.g., anti-PD-L1-PE) and viability dye [27].
- Fixation: Fix cells with formaldehyde solution [27].
- Data Acquisition: Analyze plates using a flow cytometer with autosampler (e.g., CyAn ADP with HyperCyt) [27].
- Data Analysis: Process data using specialized software (FlowJo, HyperView) and perform statistical analysis in GraphPad Prism [27].
This protocol has been successfully used to screen approximately 200,000 compounds and can be adapted to analyze expression of various cell surface proteins and response to different cytokines or stimuli [27].
The integrated workflow from compound library management to data acquisition represents a sophisticated technological pipeline that enables the rapid assessment of chemical and biological space for reaction discovery research. Each component—from the initial compound handling through the final data analysis—requires specialized equipment, validated protocols, and rigorous quality control measures to ensure reliable results. As HTS technologies continue to evolve toward even higher throughput and more complex multiplexed readouts, the fundamental principles outlined in this technical guide provide a foundation for researchers to implement and adapt these powerful screening methodologies for their specific discovery applications. The continued integration of advanced automation, miniature detection technologies, and sophisticated computational analysis promises to further enhance the efficiency and predictive power of high-throughput screening in both drug discovery and reaction optimization research.
Executing a Screen: Methodologies, Assay Types, and Practical Applications
High-throughput screening (HTS) represents a cornerstone of modern drug discovery, enabling the rapid testing of thousands to millions of compounds to identify potential therapeutic candidates [1]. Within this field, two predominant strategies have emerged: target-based screening and phenotypic screening [28]. These approaches define fundamentally different philosophies for initiating the discovery process. Target-based strategies operate on a reductionist principle, focusing on specific molecular targets known or hypothesized to be involved in disease pathology [29]. In contrast, phenotypic strategies employ a more holistic, biology-first approach, searching for compounds that elicit a desired therapeutic effect in a cell, tissue, or whole organism without preconceived notions of the molecular mechanism [30] [31]. The choice between these pathways has profound implications for screening design, resource allocation, lead optimization, and ultimately, the probability of clinical success. This guide provides an in-depth technical comparison of these methodologies, framed within the broader principles of HTS for reaction discovery research.
Core Principles and Comparative Analysis
Target-Based Screening: A Mechanism-Driven Approach
Target-based screening is founded on the principle of designing compounds to interact with a specific, preselected biological target—typically a protein such as an enzyme, receptor, or ion channel—that has been validated to play a critical role in a disease pathway [28] [32]. This approach requires a deep understanding of disease biology to identify a causal molecular target. The screening process involves developing a biochemical assay, often in a cell-free environment, that can measure the compound's interaction with (e.g., inhibition or activation of) this purified target [29] [33].
A significant advantage of this method is its high efficiency and cost-effectiveness for screening vast compound libraries, as the assays are typically robust, easily miniaturized, and amenable to ultra-high-throughput formats [28] [29]. Furthermore, knowing the target from the outset significantly accelerates the lead optimization phase. Medicinal chemists can use structure-activity relationship (SAR) data to systematically refine the hit compound for enhanced potency, selectivity, and drug-like properties [29]. Prominent successes of this approach include imatinib (which inhibits the BCR-ABL tyrosine kinase in chronic myeloid leukemia) and HIV antiretroviral therapies (such as reverse transcriptase and integrase inhibitors) that were developed based on precise knowledge of key viral proteins [32] [29].
Phenotypic Screening: A Biology-First Approach
Phenotypic screening empirically tests compounds for their ability to induce a desirable change in a disease-relevant phenotype, using systems such as primary cells, tissues, or whole organisms [30] [31]. The specific molecular target(s) and mechanism of action (MoA) can remain unknown at the outset of the campaign [28]. This approach is particularly powerful when the understanding of the underlying disease pathology is incomplete or when the disease involves complex polygenic interactions that are difficult to recapitulate with a single target [32].
A key strength of phenotypic screening is its ability to identify first-in-class medicines with novel mechanisms of action [30]. Because the assay is conducted in a biologically relevant context, hit compounds are already known to be cell-active and must possess adequate physicochemical properties (e.g., solubility, permeability) to elicit the observed effect [28] [34]. This can lead to the discovery of unexpected targets and MoAs, thereby expanding the "druggable genome" [30]. Notable successes originating from phenotypic screens include the cystic fibrosis correctors tezacaftor and elexacaftor, the spinal muscular atrophy drug risdiplam, and the antimalarial artemisinin [30] [32].
Strategic Comparison at a Glance
The table below provides a systematic, point-by-point comparison of the two screening strategies to inform strategic decision-making.
Table 1: Strategic Comparison of Target-Based and Phenotypic Screening Approaches
| Feature | Target-Based Screening | Phenotypic Screening |
|---|---|---|
| Fundamental Principle | Reductionist; tests interaction with a known, purified molecular target [29] [33] | Holistic; tests for a desired effect in a biologically complex system (cells, tissues, organisms) [30] [31] |
| Knowledge Prerequisite | Requires a deep understanding of the disease mechanism and a validated molecular target [32] [29] | Does not require prior knowledge of a specific target; useful for probing complex or poorly understood diseases [28] [32] |
| Typical Assay Format | Biochemical assays using purified proteins (e.g., enzymatic activity, binding) [1] [33] | Cell-based or whole-organism assays (e.g., high-content imaging, reporter gene assays, zebrafish models) [31] [33] |
| Throughput & Cost | Generally very high throughput and more cost-effective per compound tested [28] [34] | Often lower throughput and more resource-intensive due to complex assay systems [28] [34] |
| Hit Optimization | Straightforward; guided by structure-activity relationships (SAR) with the known target [29] | Challenging; requires subsequent target deconvolution to enable rational optimization [30] [34] |
| Key Advantage | Precision, efficiency, and a clear path for lead optimization [32] | Identifies novel targets/MoAs and ensures cellular activity from the outset [28] [30] |
| Primary Challenge | Risk of poor clinical translation if the chosen target is not critically pathogenic [32] [29] | Time-consuming and technically challenging target identification (deconvolution) phase [30] [34] |
| Typical Output | Best-in-class drugs that improve upon existing mechanisms [34] | A disproportionate number of first-in-class drugs [30] [34] |
Experimental Protocols and Workflows
Protocol for a Target-Based Biochemical HTS
This protocol outlines a standard workflow for a target-based high-throughput screen using a purified enzyme.
1. Assay Development and Validation:
- Target Preparation: Purify the recombinant protein (e.g., a kinase) to homogeneity. Confirm activity and stability under assay conditions [1].
- Assay Design: Establish a robust biochemical reaction, such as a kinase reaction transferring a phosphate group from ATP to a peptide substrate. To enable HTS, implement a detection method like fluorescence, luminescence, or mass spectrometry [1] [29]. Fluorescence-based methods are common due to their sensitivity and adaptability to HTS formats [1].
- Miniaturization and Validation: Scale down the assay to a 384-well or 1536-well microplate format. Validate the assay by calculating the Z'-factor (>0.5 is excellent) to confirm robustness and reproducibility, ensuring it is suitable for automation [1] [30].
2. Library Preparation and Screening:
- Compound Management: Prepare the compound library in DMSO and store it in microplates. Use automated liquid-handling robots to dispense nanoliter aliquots of each compound into the assay plates [1].
- Robotic Screening: The automated system adds the purified target, substrate, and cofactors (e.g., ATP) to the plates. After incubation, the detection reagent is added, and signals are read by a microplate reader [1].
3. Hit Triage and Confirmation:
- Data Analysis: Normalize data using controls and apply statistical methods (e.g., Z-score) to identify "hits"—compounds that show significant activity above a defined threshold [33]. Use cheminformatic filters to flag and remove pan-assay interference compounds (PAINS) and other false positives [1] [28].
- Hit Confirmation: Re-test confirmed hits in dose-response experiments to determine potency (IC50 values). Use counter-screens to assess selectivity against related targets [1].
Figure 1: Workflow for a target-based high-throughput screen.
Protocol for a Phenotypic HTS
This protocol describes a phenotypic screen using a high-content, cell-based assay to identify compounds that reverse a disease-associated phenotype.
1. Development of a Disease-Relevant Model:
- Cell System Selection: Choose a physiologically relevant cell system. This could be a genetically engineered cell line, a patient-derived primary cell, or induced pluripotent stem cell (iPSC)-derived cells [31] [34].
- Phenotype and Readout: Define a quantifiable, disease-relevant phenotype. Examples include:
- High-Content Imaging: Measure changes in neurite outgrowth in a neurodegenerative model, organelle morphology, or protein aggregation (e.g., amyloid-β in Alzheimer's models) [31].
- Reporter Gene Assay: Use a luciferase or GFP reporter under the control of a pathway-specific promoter (e.g., an innate immune or fibrotic pathway) [33].
2. Assay Implementation and Screening:
- Assay Optimization: Optimize cell seeding density, compound treatment time, and staining protocols (if applicable) to ensure a robust and reproducible signal-to-background ratio.
- Automated Screening: Seed cells in 384-well plates. Use robotics to transfer compound libraries. For imaging assays, use an automated high-content imager to capture multiple cellular features per well [34] [33].
- Data Acquisition: Extract quantitative data from images (e.g., fluorescence intensity, cell count, morphological parameters).
3. Hit Validation and Target Deconvolution:
- Hit Identification: Apply statistical methods like the B-score to correct for plate positional effects and identify active compounds [33].
- Validation: Confirm hits in secondary assays that model the disease through a different readout.
- Target Deconvolution: This is a critical, post-hoc step. Techniques include:
- Chemical Proteomics: Use immobilized hit compounds as bait to pull down interacting proteins from cell lysates, which are then identified by mass spectrometry [30] [35].
- Functional Genomics: CRISPR or RNAi screens to identify genes whose knockout or knockdown abrogates the compound's phenotypic effect [30] [34].
- Transcriptomics/Profiling: Compare the gene expression signature of the hit compound to signatures of compounds with known MoA [30].
Figure 2: Workflow for a phenotypic high-throughput screen.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for executing the screening protocols described above.
Table 2: Essential Research Reagent Solutions for HTS Campaigns
| Reagent / Material | Function and Description | Application Notes |
|---|---|---|
| Chemical Libraries | Diverse collections of small molecules (e.g., 10,000 - 2,000,000+ compounds) used to identify "hits" [35] [1]. | Includes diverse synthetic compounds, natural products, and focused "chemo-genomic" libraries of known bioactives [35]. Drug-like properties are a key selection criterion. |
| Purified Target Proteins | Recombinant, highly purified proteins (enzymes, receptors) used as the core reagent in target-based biochemical assays [1]. | Requires validation of correct folding and activity. Purity is critical to minimize assay interference. |
| Disease-Relevant Cell Lines | Engineered cell lines, patient-derived cells, or iPSC-derived cells used to model disease phenotypes [31] [34]. | The choice of cell model is the most critical factor for phenotypic screening relevance (e.g., 3D cultures, co-cultures) [34]. |
| Detection Reagents | Probes that generate a measurable signal (fluorescence, luminescence) upon a biological event [1] [33]. | Examples: Fluorescent dyes for cell viability, antibody-based detection, luciferase substrates for reporter assays, and FRET probes for enzymatic activity. |
| Microtiter Plates | Standardized plates with 96, 384, or 1536 wells for performing miniaturized assays [1]. | Assay volume and detection method dictate plate selection (e.g., clear bottom for imaging, white for luminescence). |
| Automated Liquid Handlers | Robotic systems that accurately dispense nano- to microliter volumes of compounds and reagents [1]. | Essential for ensuring reproducibility and throughput in both screening strategies. |
| High-Content Imagers | Automated microscopes coupled with image analysis software for extracting quantitative data from cell-based assays [34]. | Core technology for complex phenotypic screening, allowing multiparametric analysis. |
| MK-0608 | MK-0608, CAS:1001913-41-2, MF:C12H16N4O4, MW:280.28 g/mol | Chemical Reagent |
| AS-252424 | AS-252424, CAS:1138220-19-5, MF:C14H8FNO4S, MW:305.28 g/mol | Chemical Reagent |
Integrated and Future Perspectives
The historical dichotomy between target-based and phenotypic screening is increasingly giving way to a more integrated and synergistic paradigm [28] [34]. A powerful strategy involves using phenotypic screening to identify novel, high-quality hit compounds in a disease-relevant context, followed by target deconvolution to reveal the underlying molecular mechanism. This knowledge can then be used to deploy target-based assays for more efficient lead optimization and the development of subsequent best-in-class drugs [30] [34]. This combined approach leverages the strengths of both methods while mitigating their individual weaknesses.
Future directions in the field are being shaped by several technological advances. The use of more physiologically relevant models, such as 3D organoids, organs-on-chips, and coculture systems that incorporate immune components, is making phenotypic assays more predictive of clinical outcomes [34]. Advances in target deconvolution methods, particularly in chemical proteomics and computational analysis of multi-omics data, are reducing the major bottleneck in phenotypic discovery [30] [31]. Furthermore, the application of functional genomics (CRISPR) and machine learning/artificial intelligence is revolutionizing both approaches, enabling better target validation, library design, and data analysis [30] [34] [1]. For the modern drug discovery professional, mastery of both strategic paradigms—and the wisdom to know when and how to integrate them—is key to navigating the complex landscape of reaction discovery research and delivering transformative medicines.
High-Throughput Screening (HTS) represents a foundational approach in modern drug discovery and reaction discovery research, enabling the rapid testing of hundreds of thousands of compounds against biological targets [1]. The effectiveness of HTS campaigns depends critically on the selection of appropriate assay readout technologies, which transform biological events into quantifiable signals [36]. These readouts provide the essential data for identifying initial "hit" compounds from vast libraries, forming the basis for subsequent medicinal chemistry optimization and lead development [20]. This technical guide examines the four principal readout technologies—fluorescence, luminescence, absorbance, and high-content imaging—within the context of HTS principles, providing researchers with the analytical framework necessary for informed technology selection.
The transition from traditional low-throughput methods to automated, miniaturized HTS has revolutionized early drug discovery [1]. Contemporary HTS implementations typically utilize microplates in 96-, 384-, or 1536-well formats, combined with automated liquid handling systems to maximize throughput while minimizing reagent consumption [36]. The choice of readout technology directly influences key screening parameters including sensitivity, dynamic range, cost, and susceptibility to artifacts [1]. Understanding the fundamental principles, applications, and limitations of each technology platform is therefore essential for designing robust screening campaigns that generate biologically meaningful data with minimal false positives and negatives [1].
Fundamental Principles and Technical Specifications
Fluorescence-Based Detection
Fluorescence detection operates on the principle of molecular fluorescence, where certain compounds (fluorophores) absorb light at specific wavelengths and subsequently emit light at longer wavelengths [20]. The difference between absorption and emission wavelengths is known as the Stokes shift. Fluorescence-based assays offer exceptional sensitivity, capable of detecting analytes at concentrations as low as picomolar levels, and are amenable to homogeneous "mix-and-read" formats that minimize handling steps [36].
Several fluorescence detection modalities have been developed for HTS applications. Fluorescence Intensity (FI) measures the overall brightness of a sample and is widely used in enzymatic assays [36]. Fluorescence Polarization (FP) measures the rotation of molecules in solution by detecting the retention of polarization in emitted light; it is particularly valuable for monitoring molecular interactions such as receptor-ligand binding without separation steps [36]. Time-Resolved Fluorescence (TRF) and Förster Resonance Energy Transfer (FRET) utilize lanthanide chelates with long fluorescence lifetimes to eliminate short-lived background fluorescence, significantly improving signal-to-noise ratios for challenging cellular targets [36]. Fluorescence Resonance Energy Transfer (FRET) measures non-radiative energy transfer between donor and acceptor fluorophores when in close proximity, making it ideal for studying protein-protein interactions and conformational changes [36].
Table 1: Comparison of Major Fluorescence Detection Modalities
| Technology | Detection Principle | Typical Applications | Advantages | Limitations |
|---|---|---|---|---|
| Fluorescence Intensity (FI) | Measures total emitted light | Enzyme activity, cell viability | Simple implementation, low cost | Susceptible to compound interference |
| Fluorescence Polarization (FP) | Measures molecular rotation | Molecular binding, receptor-ligand interactions | Homogeneous format, no separation needed | Limited by molecular size |
| FRET | Energy transfer between fluorophores | Protein interactions, cleavage assays | Highly specific, low background | Requires specific fluorophore pairing |
| TR-FRET | Combines time-resolved and FRET | Kinase assays, protein-protein interactions | Reduced autofluorescence, robust | Higher reagent costs |
The high sensitivity of fluorescence detection makes it particularly suitable for miniaturized formats, including 1536-well plates and beyond, enabling Ultra-High-Throughput Screening (uHTS) campaigns that can exceed 100,000 compounds per day [1]. However, fluorescence-based assays can be susceptible to compound interference through autofluorescence or inner filter effects, particularly with short-wavelength excitation (below 400 nm) [20]. These limitations can be mitigated through careful assay design, including the use of red-shifted fluorophores and appropriate control wells.
Figure 1: Generalized workflow for fluorescence-based HTS showing major detection modalities
Luminescence Detection
Luminescence detection measures light emission generated through biochemical reactions, typically involving the enzymatic conversion of a substrate to a light-producing product [1]. Unlike fluorescence, luminescence does not require an excitation light source, which eliminates problems associated with autofluorescence and light scattering, resulting in exceptionally high signal-to-background ratios [1]. This technology is particularly valuable for detecting low-abundance targets and in complex biological matrices where background interference may compromise fluorescence readings.
The most widely implemented luminescence system utilizes luciferase enzymes, particularly from firefly (Photinus pyralis) and marine organisms (Renilla reniformis) [1]. Firefly luciferase produces light through ATP-dependent oxidation of luciferin, making it ideal for monitoring ATP levels in cell viability and cytotoxicity assays, as well as for reporter gene applications where luciferase expression is linked to promoter activity [1]. Beta-lactamase reporter systems provide an alternative luminescent platform, particularly useful for gene expression studies in live cells [1]. Additionally, chemiluminescence detection methods that generate light through non-enzymatic chemical reactions are employed for immunoassays and nucleic acid detection, offering ultra-sensitive detection of proteins and DNA/RNA targets [1].
Table 2: Luminescence Detection Methods and Applications
| Method | Detection Principle | Common Applications | Sensitivity | Dynamic Range |
|---|---|---|---|---|
| ATP-based Luminescence | Luciferase-mediated ATP detection | Cell viability, cytotoxicity | 1-1000 cells | 4-5 logs |
| Reporter Gene Assays | Luciferase under promoter control | Gene expression, signaling pathways | Attomole levels | 6-8 logs |
| Beta-lactamase Reporter | FRET-based substrate cleavage | Live-cell gene expression | - | 3-4 logs |
| Chemiluminescence Immunoassays | Peroxidase-labeled antibodies | Protein quantification, phosphorylation | Femtogram levels | 4-5 logs |
Luminescence assays typically demonstrate broader dynamic ranges (often spanning 4-8 orders of magnitude) compared to fluorescence-based methods, enabling more accurate quantification of both weak and strong responses within the same assay [1]. The principal limitations include reagent costs and the potential for compound interference through enzyme inhibition, particularly with luciferase-based systems. These challenges can be addressed through counter-screening assays and the implementation of orthogonal validation approaches.
Absorbance Spectroscopy
Absorbance spectroscopy represents one of the oldest and most straightforward detection methods in HTS, measuring the attenuation of light as it passes through a sample [1]. This technique quantifies the concentration of chromophores—molecules that absorb specific wavelengths of light—according to the Beer-Lambert law, which establishes a linear relationship between absorbance and analyte concentration [1]. While generally less sensitive than fluorescence or luminescence methods, absorbance assays offer robustness, simplicity, and cost-effectiveness that maintain their utility in HTS applications.
Common implementations of absorbance detection in HTS include colorimetric enzyme assays that monitor the conversion of substrates to colored products [1]. For example, phosphatase and protease activities are frequently assessed using p-nitrophenol-derived substrates that generate yellow-colored products upon cleavage [1]. Cell viability assays based on tetrazolium dye reduction (such as MTT and XTT) remain widely used for cytotoxicity screening, measuring the metabolic activity of cells through the formation of formazan products with characteristic absorbance spectra [1]. Similarly, resazurin reduction assays provide a fluorescent or colorimetric readout of cellular metabolic capacity, useful for proliferation and toxicity assessments [1].
The main advantages of absorbance detection include methodological simplicity, minimal equipment requirements, and cost-effectiveness, particularly for academic screening centers with limited budgets [1]. However, absorbance assays typically offer lower sensitivity (micromolar to millimolar range) compared to fluorescence or luminescence methods and are more susceptible to interference from colored compounds in screening libraries [1]. These limitations restrict their application in miniaturized formats and for targets requiring high sensitivity.
High-Content Imaging and Analysis
High-Content Screening (HCS) represents an advanced imaging-based approach that combines automated microscopy with multiparametric image analysis to extract quantitative data from cellular systems [37] [38]. Unlike conventional HTS methods that generate single endpoint measurements, HCS provides spatially and temporally resolved information at the single-cell level, enabling detailed characterization of complex phenotypic responses [37]. This technology has become increasingly valuable for drug discovery, particularly in the assessment of complex cellular processes and the screening of more physiologically relevant 3D cell models [37].
HCS implementations typically utilize fluorescence microscopy as the primary imaging modality, often incorporating multiple fluorescent probes to simultaneously monitor different cellular components or processes [37]. Confocal microscopy systems are frequently employed to enhance spatial resolution and reduce out-of-focus light, particularly important for imaging thicker biological samples such as 3D spheroids and organoids [37]. Recent advances include super-resolution microscopy techniques that surpass the diffraction limit of conventional light microscopy, providing unprecedented detail of subcellular structures [37]. Live-cell imaging capabilities enable temporal monitoring of dynamic processes such as protein trafficking, cell migration, and morphological changes in response to compound treatment [37].
Table 3: High-Content Imaging Applications and Analysis Parameters
| Biological System | Common Assays | Typical Stains/Markers | Analysis Parameters |
|---|---|---|---|
| 2D Cell Cultures | Cell cycle, toxicity, translocation | DAPI, phosphorylated proteins, viability dyes | Nuclear intensity, cytoplasmic distribution, cell count |
| 3D Spheroids/Organoids | Invasion, growth, drug penetration | Live/dead stains, extracellular matrix markers | Volume, morphology, viability gradients |
| Primary Neurons | Neurodegeneration, neurite outgrowth | Tau, β-tubulin, synaptic markers | Neurite length, branching, soma size |
| Stem Cell Models | Differentiation, organoid development | Lineage-specific transcription factors | Marker expression, morphological changes |
The implementation of HCS in drug discovery provides significant advantages, including the ability to detect heterogeneous responses within cell populations, monitor subcellular localization, and extract multiple readouts from a single assay [37]. However, HCS presents technical challenges including substantial data storage requirements, complex image analysis workflows, and longer acquisition times compared to plate-based readouts [37]. These limitations are being addressed through advances in computational methods, including machine learning-based image analysis and improved data compression algorithms [37].
Figure 2: High-content screening workflow showing key steps from sample preparation to multiparametric analysis
Experimental Protocols and Methodologies
Fluorescence Polarization Binding Assay
Fluorescence Polarization (FP) assays measure molecular interactions based on changes in rotational diffusion when a small fluorescent ligand binds to a larger macromolecule [36]. This homogeneous, solution-based method is ideal for HTS applications as it requires no separation steps and can be implemented in miniaturized formats [36].
Protocol for FP-Based Receptor-Ligand Binding Assay:
Reagent Preparation:
- Prepare assay buffer (typically PBS or Tris-based with 0.01-0.1% BSA to prevent non-specific binding)
- Dilute receptor protein to appropriate concentration (typically 0.1-10 nM depending on affinity)
- Prepare fluorescent tracer ligand at 2× final concentration (typically 1-10 nM)
Assay Assembly in 384-Well Format:
- Add 10 μL compound solution (in DMSO, final concentration ≤1%) to each well
- Add 10 μL receptor solution to all wells except controls
- Add 10 μL buffer to no-receptor control wells
- Incubate plates for 15-30 minutes at room temperature
- Add 20 μL tracer solution to all wells
- Incubate plates for equilibrium (typically 30-120 minutes)
Detection and Data Analysis:
- Read plates using a fluorescence polarization plate reader
- Calculate polarization values in millipolarization units (mP)
- Determine specific binding by comparing to maximal (no compound) and minimal (no receptor) controls
- Fit dose-response data to determine IC50 values for competing compounds
Critical Parameters for FP Assay Development:
- Tracer ligand should have dissociation constant (Kd) similar to expected compound affinities
- Receptor concentration should be near Kd value for optimal sensitivity
- Molecular weight ratio between bound and free tracer should exceed 2:1 for significant mP change
- DMSO tolerance should be validated, typically not exceeding 1% final concentration
Luminescent Cell Viability Assay
ATP-dependent luminescence assays provide a sensitive method for quantifying cell viability and cytotoxicity in HTS formats [1]. These assays measure cellular ATP levels, which correlate directly with metabolically active cells.
Protocol for ATP-Based Viability Screening:
Cell Culture and Plate Preparation:
- Seed cells in white-walled 384-well plates at optimized density (typically 1,000-5,000 cells/well)
- Incubate cells for 24 hours under appropriate conditions to allow attachment
- Add test compounds using automated liquid handling (pin tool or acoustic dispensing)
Compound Treatment and Incubation:
- Incubate compound-treated plates for desired exposure period (typically 24-72 hours)
- Include controls: no cells (background), no treatment (maximal viability), reference cytotoxic compound (minimal viability)
Luminescence Detection:
- Equilibrate plates to room temperature for 30 minutes
- Add equal volume of ATP-luminescence reagent (containing luciferase and substrate)
- Mix plates by orbital shaking for 2-5 minutes
- Measure luminescence after 10-minute signal stabilization period
Data Analysis and Normalization:
- Subtract background luminescence (no-cell controls)
- Normalize data: 0% viability = cytotoxic control, 100% viability = untreated control
- Calculate Z'-factor for assay quality control: Z' = 1 - (3×SDpositive + 3×SDnegative) / |Meanpositive - Meannegative|
- Determine IC50 values from dose-response curves using four-parameter logistic fit
Validation Parameters for Robust Screening:
- Z'-factor should exceed 0.5 for excellent assay quality
- Signal-to-background ratio should be >10:1
- Coefficient of variation (CV) for controls should be <10%
- Edge effects should be minimized through proper plate handling
High-Content Imaging of 3D Spheroid Models
High-content imaging of 3D cellular models provides more physiologically relevant data compared to traditional 2D cultures, particularly for oncology and toxicity screening [37]. This protocol describes the implementation for multicellular tumor spheroids.
Protocol for 3D Spheroid Imaging and Analysis:
Spheroid Generation:
- Seed cells in ultra-low attachment 384-well plates at 500-2,000 cells/well
- Centrifuge plates at 200×g for 3 minutes to encourage aggregate formation
- Culture spheroids for 3-7 days with periodic medium changes
Compound Treatment and Staining:
- Add test compounds using DMSO vehicle control (final concentration ≤0.5%)
- Incubate for desired treatment period (typically 72-144 hours)
- Add live-cell stains (e.g., Calcein-AM for viability, Hoechst for nuclei)
- For fixed endpoint assays, add paraformaldehyde (4% final) and permeabilization buffer
- Stain with antibodies for specific targets and appropriate fluorescent conjugates
Image Acquisition:
- Acquire z-stack images using automated confocal microscope (typically 10-20 μm depth, 5 μm steps)
- Use 10× or 20× objectives appropriate for spheroid size (typically 200-500 μm diameter)
- Set exposure times to avoid saturation while maintaining adequate signal
- Include flat-field correction for illumination uniformity
Image Analysis and Quantification:
- Perform maximum intensity projection of z-stacks
- Segment spheroids using intensity thresholding and morphological operations
- Quantify spheroid volume, cross-sectional area, and circularity
- Segment individual nuclei within spheroids for viability counting
- Analyze intensity gradients from periphery to core for penetration studies
Technical Considerations for 3D Imaging:
- Light scattering increases with spheroid size, requiring optimized clearing protocols
- Antibody penetration may be limited beyond 100 μm, requiring extended incubation
- Viability stains may not fully penetrate necrotic cores, requiring sectioning validation
- Automated analysis algorithms must account for spatial heterogeneity within spheroids
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents and Materials for HTS Assay Development
| Category | Specific Examples | Function in HTS | Technical Considerations |
|---|---|---|---|
| Microplates | 384-well, 1536-well black/white plates | Assay miniaturization and formatting | Black plates for fluorescence, white for luminescence, U-bottom for 3D cultures |
| Detection Kits | Transcreener ADP², CellTiter-Glo | Biochemical and cellular readouts | Validate Z'-factor >0.5, signal-to-background >5:1 |
| Fluorescent Probes | Fluorescein, Rhodamine, Cyanine dyes | Signal generation in fluorescence assays | Avoid spectral overlap in multiplexing, check compound interference |
| Cell Lines | Reporter lines, primary models (iPSC-derived) | Biologically relevant screening systems | Validate phenotypic stability, passage number effects |
| Liquid Handling | Automated dispensers, pin tools | Assay assembly and compound transfer | Verify precision (CV <10%) at working volumes |
| Enzymes/Receptors | Kinases, GPCRs, ion channels | Primary biological targets | Verify activity lot-to-lot, optimize concentration near Km |
| Cell Culture Matrices | Basement membrane extracts, synthetic hydrogels | 3D culture support for complex models | Optimize concentration for spheroid formation and compound penetration |
| GW9662-d5 | GW9662-d5, MF:C13H9ClN2O3, MW:281.70 g/mol | Chemical Reagent | Bench Chemicals |
| JNJ-38877605 | JNJ-38877605, CAS:1072116-03-0, MF:C19H13F2N7, MW:377.3 g/mol | Chemical Reagent | Bench Chemicals |
Comparative Analysis and Technology Selection Framework
The selection of appropriate readout technology represents a critical decision point in HTS campaign design, with significant implications for data quality, cost, and biological relevance [37] [1]. Each technology platform offers distinct advantages and limitations that must be balanced against specific screening objectives and constraints.
Table 5: Strategic Selection Guide for HTS Readout Technologies
| Parameter | Fluorescence | Luminescence | Absorbance | High-Content Imaging |
|---|---|---|---|---|
| Sensitivity | Picomolar-nanomolar | Femtomolar-picomolar | Nanomolar-micromolar | Single-cell resolution |
| Throughput | High (10^5/day) | High (10^5/day) | Medium (10^4/day) | Lower (10^3-10^4/day) |
| Cost per Well | $$ | $$$ | $ | $$$$ |
| Multiplexing Capability | High (spectral) | Medium (temporal) | Low | Very high (spatial) |
| Complexity | Medium | Medium | Low | High |
| 3D Compatibility | Limited | Good | Poor | Excellent |
| Artifact Susceptibility | Autofluorescence, quenching | Enzyme inhibition | Colored compounds | Segmentation errors |
| Information Content | Single parameter | Single parameter | Single parameter | Multiparametric |
Fluorescence-based methods typically represent the most versatile option for biochemical assays and certain cell-based applications, offering a balance between sensitivity, throughput, and cost [36]. The availability of multiple detection modalities (FI, FP, FRET, TR-FRET) enables adaptation to diverse biological targets, though researchers must remain vigilant about compound interference [36]. Luminescence assays provide superior sensitivity and broader dynamic ranges, making them ideal for targets with low signal output and for reporter gene applications where background must be minimized [1]. The simplified instrumentation requirements of absorbance detection maintain its utility for straightforward enzymatic assays and educational settings, despite limitations in sensitivity and miniaturization potential [1].
High-content imaging occupies a specialized niche in the HTS technology landscape, trading absolute throughput for unparalleled information content [37] [38]. The ability to resolve subcellular localization, morphological changes, and heterogeneous responses within cell populations makes HCS indispensable for phenotypic screening and complex model systems, particularly 3D cultures that more accurately recapitulate tissue physiology [37]. The decision to implement HCS should be driven by biological questions that require spatial or single-cell resolution, with full acknowledgment of the substantial data management and analysis challenges involved [37].
Contemporary HTS campaigns frequently employ orthogonal approaches, using simpler, higher-throughput methods for primary screening followed by secondary confirmation with more information-rich technologies [1]. This tiered strategy maximizes efficiency while ensuring biological relevance, particularly important given the increasing emphasis on physiologically relevant models including 3D cultures, organoids, and patient-derived cells in early drug discovery [37] [1].
High-Throughput Screening (HTS) is an automated methodology that enables the rapid testing of thousands to millions of biological, genetic, chemical, or pharmacological samples [39]. At the core of every HTS system lie two fundamental components: the microplate, which acts as a miniature laboratory for reactions, and liquid handling instruments, which enable the precise manipulation of minute fluid volumes [39] [40]. The synergy between standardized microplates and advanced liquid handling has revolutionized reaction discovery research, allowing scientists to identify promising candidates for further study with unprecedented speed and efficiency [39] [41]. This technical guide explores the principles, specifications, and workflows of these core components within the context of modern HTS.
Microplates: The Foundation of HTS
Historical Development and Standardization
The microplate was invented in 1951 by Hungarian microbiologist Dr. Gyula Takátsy, who sought a cost-effective solution to process a high volume of blood tests during an influenza outbreak [15] [42] [43]. He created the first 96-well microplate by hand, using calibrated spiral loops to handle liquid transfers [42]. The commercialization of microplates began in 1965 with the first molded 96-well plate, and widespread adoption was fueled by the development of the Enzyme-Linked Immunosorbent Assay (ELISA) in the mid-1970s [43]. A critical milestone was reached in the 1990s with the establishment of dimensional standards by the Society for Biomolecular Screening (SBS), now maintained by the Society for Laboratory Automation and Screening (SLAS) [42]. This standardization of footprint dimensions (127.76 mm × 85.48 mm) ensured compatibility with automated handling equipment and readers across manufacturers, solidifying the microplate's role as a ubiquitous consumable in life science laboratories [42] [43].
Microplate Formats and Specifications
The drive for higher throughput and lower reagent costs has led to the development of microplates with increasingly higher well densities. The table below summarizes the key characteristics of standard microplate formats.
Table 1: Standard Microplate Formats and Volumes for HTS Applications
| Well Number | Standard Well Volume (µL) | Low-Volume Variant (µL) | Primary Applications and Notes |
|---|---|---|---|
| 96 | 100 - 300 [42] | 50 - 170 (Half-area) [42] | The most common format; ideal for ELISA, general assay development, and lower-throughput studies [39] [42]. |
| 384 | 30 - 100 [42] | 5 - 25 (Low-volume) [42] | Standard for HTS; offers 4x the throughput of 96-well on the same footprint, significantly reducing reagent costs [39] [43]. |
| 1536 | 5 - 25 [42] | - | Used for Ultra-High-Throughput Screening (uHTS); requires specialized liquid handlers for nanoliter dispensing [39] [43]. |
| 3456 | 1 - 5 [42] | - | Niche applications for extreme miniaturization; not widely adopted due to significant liquid handling challenges [42] [43]. |
Material, Color, and Well Geometry
The choice of microplate is highly application-dependent, with critical considerations extending beyond well count.
- Materials: The most common material is polystyrene, prized for its transparency and cost-effectiveness for most optical assays [42]. For UV light transmission (e.g., nucleic acid quantification), Cyclo-Olefin Copolymer (COC) is required [42]. Polypropylene is used for its chemical resistance and temperature stability in storage and PCR [42].
- Color: The plate color is selected based on the detection mode to optimize the signal-to-noise ratio. Clear plates are used for absorbance assays [42]. Black plates minimize background and cross-talk for fluorescence intensity assays [42]. White plates reflect light to maximize signal output for luminescence and time-resolved fluorescence [42].
- Well Bottom Shape: The well bottom geometry affects liquid behavior. A flat (F) bottom is optimal for absorbance reading and adherent cell culture [42]. A round (U) bottom facilitates mixing and is suited for cell suspension assays [42]. A conical (V) bottom allows for maximal sample retrieval, useful for sample storage [42].
Liquid Handling: The Engine of Automation
Liquid handling instruments are critical for ensuring precision, accuracy, and reproducibility in HTS workflows. They automate the transfer and dispensing of reagents and samples, guarding against pipetting errors and enabling the miniaturization of assays [39] [40].
Types of Liquid Handling Instruments
The evolution of liquid handling technology has kept pace with the increasing density of microplates.
- Automated Pipetting Systems: These programmable systems provide consistent, repeatable liquid transfers for complex tasks like serial dilutions and reagent mixing, making them ideal for large-scale HTS [40].
- Robotic Liquid Handlers: These advanced systems automate entire workflows, transferring microplates between pipetting stations, incubators, and detectors with minimal human intervention. They are essential for ultra-high-throughput screening (uHTS) [39] [40].
- Non-Contact Dispensers: Technologies like acoustic liquid handling use sound waves to transfer nanoliter volumes without physical contact with the liquid, virtually eliminating the risk of cross-contamination [40]. Bulk reagent dispensers are used to quickly add a common reagent to an entire microplate [44].
The Importance of Precision and Accuracy
In HTS, where assays are miniaturized and volumes can be in the nanoliter range, the precision of liquid handling is paramount [40]. Small variations can lead to significant errors, resulting in false positives or negatives [40]. Accurate dispensing is also crucial for optimizing resource use, as it ensures that only the required volumes of valuable reagents and samples are consumed [40]. This precision is the enabling factor for the miniaturization seen in 384-well and 1536-well formats [40].
Integrated HTS Workflow: From Sample to Hit
The following diagram illustrates the logical flow of a typical integrated HTS workflow, highlighting the roles of microplates and liquid handling at each stage.
Diagram 1: Integrated HTS Workflow. The process flows from sample preparation to hit identification, with liquid handling automation (green) and microplates (red) supporting multiple stages.
Experimental Protocol: A Representative HTS Campaign
The following detailed methodology outlines a cell-based HTS campaign to identify compounds that modulate a specific therapeutic target.
Step 1: Sample and Library Preparation
- Objective: Transfer a library of chemical compounds from stock plates to assay-ready plates.
- Procedure: Using an automated liquid handler, dispense nanoliter to microliter volumes of compounds from stored source plates (e.g., in DMSO) into a 384-well or 1536-well assay microplate [39] [40]. The assay plates are often polypropylene to withstand potential temperature changes.
Step 2: Cell Seeding and Treatment
- Objective: Introduce a biologically relevant system into the assay.
- Procedure: A bulk reagent dispenser is used to rapidly add a suspension of cells (e.g., engineered cell lines expressing the target of interest) in media to all wells of the assay plate [44]. The microplate used here is typically tissue-culture treated, clear-bottomed polystyrene to support cell adhesion and allow for microscopic analysis [45]. The plate is then incubated to allow cells to adhere and stabilize.
Step 3: Reagent Addition and Assay Incubation
- Objective: Initiate the biochemical reaction.
- Procedure: After cell stabilization, an automated pipetting system or bulk dispenser adds a specific substrate or reagent to all wells to start the reaction [40]. The plate is then incubated for a predetermined time to allow the reaction to proceed.
Step 4: Assay Readout and Detection
- Objective: Quantify the biological response.
- Procedure: The microplate is transferred via a robotic arm to a microplate reader [39]. The reader measures the assay endpoint, which could be fluorescence intensity, luminescence, or absorbance [39] [41]. The plate color is selected based on the detection mode—black for fluorescence, white for luminescence, and clear for absorbance [42].
Step 5: Data Processing and Hit Identification
- Objective: Identify "hits"—compounds that produced a desired and statistically significant response.
- Procedure: Data processing software analyzes the massive dataset generated by the plate reader. Hits are typically identified by applying a cutoff threshold, such as selecting compounds that exhibit activity three standard deviations above the negative control, or the top 1% of active compounds in the screen [39].
The Scientist's Toolkit: Essential Research Reagent Solutions
The table below catalogs key materials and reagents essential for conducting HTS experiments.
Table 2: Essential Reagents and Materials for HTS
| Item | Function in HTS |
|---|---|
| Assay-Reigned Microplates | Standardized plates (96-, 384-, 1536-well) with surfaces tailored for specific applications (e.g., tissue-culture treated for cells, high-binding for proteins) that serve as the reaction vessel for the entire assay [45] [42]. |
| Compound Libraries | Collections of thousands to millions of small molecules, natural products, or FDA-approved drugs that are screened to find initial "hit" compounds [39]. |
| Cell Lines | Biologically relevant systems, often engineered to report on the activity of a specific drug target or pathway via a detectable signal (e.g., luminescence) [39]. |
| Detection Reagents | Chemical probes (e.g., fluorescent dyes, luminescent substrates) used to generate a measurable signal proportional to the activity or concentration of the target analyte [41]. |
| Bulk Buffers and Media | Aqueous solutions used to reconstitute reagents, maintain cell health, and provide the appropriate chemical environment (pH, ionic strength) for the assay biochemistry to function properly [40]. |
| PPQ-102 | PPQ-102, MF:C22H21N5O3, MW:403.4 g/mol |
| AG1557 | AG1557, MF:C19H16BrNO2, MW:370.2 g/mol |
Microplates and liquid handling systems form the indispensable core of high-throughput screening. The continued evolution of these technologies—from the first handmade 96-well plate to today's high-density formats and sophisticated non-contact dispensers—has been driven by the dual needs for greater throughput and higher efficiency [15] [43]. As HTS continues to advance into more complex areas like 3D cell culture and genomic screening, the demands on these core components will only intensify [45] [43]. Future developments will likely focus on further miniaturization, even greater precision in handling picoliter volumes, and the tighter integration of microfluidics and lab-on-a-chip technologies [40] [43]. For researchers in reaction discovery and drug development, a deep understanding of the principles, capabilities, and limitations of microplates and liquid handling is fundamental to designing robust, successful, and impactful screening campaigns.
High-Throughput Screening (HTS) is a cornerstone of modern drug discovery, enabling the rapid, large-scale testing of chemical libraries against biological targets to identify active compounds, validate drug targets, and accelerate hit-to-lead development [46]. The quality of the initial screening library is a critical determinant of downstream success; a well-curated library provides a powerful path to meaningful hits, whereas a poor-quality library generates false positives and chemically intractable leads, wasting significant time and resources [47]. The evolution of screening libraries has closely followed advances in medicinal chemistry, computational methods, and molecular biology, shifting from quantity-driven collections towards quality-focused, strategically designed sets [47]. This guide outlines the core principles for building a compound library tailored for HTS in reaction discovery research, with a focus on compound quality, diversity, and druggability.
Core Considerations for Library Curation
Compound Quality: Ensuring Chemical Integrity and Utility
Compound quality is paramount to avoid artifacts and false results. Key considerations include:
- Chemical Purity and Integrity: Libraries should consist of compounds with verified high purity and confirmed structural integrity. Impurities can interfere with assay readouts, leading to false positives or negatives.
- Assay Interference Filters: Proactively filter out compounds known to cause assay interference. This includes pan-assay interference compounds (PAINS), which can produce misleading results through non-specific mechanisms, as well as compounds with reactive or promiscuous functionalities that are unlikely to yield viable leads [47].
- Stock Control and Availability: When sourcing compounds from external vendors or aggregators, rigorous stock control and up-to-date inventory tracking are essential to maintain the library's relevance and reliability [47].
Chemical Diversity: Exploring Chemical Space
A diverse library increases the probability of finding novel chemical starting points against a wide array of biological targets.
- Scaffold Diversity: Prioritize libraries that encompass a broad range of core molecular scaffolds. This diversity helps in exploring different regions of chemical space and increases the chances of identifying novel chemotypes with the desired activity [47].
- Natural Product-Inspired Motifs: Incorporate natural product-inspired scaffolds and privileged structures known to interact with certain target classes (e.g., kinases) to explore more complex and biologically relevant regions of chemical space [47].
- 3D Diversity: Beyond flat, aromatic molecules, consider compounds with stereochemical complexity and three-dimensional character, as they may offer better opportunities for interacting with protein targets [47].
Druggability: Optimizing for Drug-Like Properties
Early attention to druggability increases the likelihood that identified hits can progress through optimization and into the clinic.
- Drug-Likeness Criteria: Apply established guidelines like Lipinski's Rule of 5 and additional filters for toxicity and assay interference to define 'drug-likeness' and improve the overall quality of the library [47]. These rules predict favorable absorption, distribution, metabolism, and excretion (ADME) properties.
- Target-Class Relevance: Enrich libraries with structures known to interact with specific target families (e.g., covalent inhibitors, CNS-penetrant chemotypes, macrocyclic fragments) to improve hit rates for particular projects [47].
- Early ADME/Tox Considerations: Integrate early-stage ADME (Absorption, Distribution, Metabolism, Excretion) and toxicity (Tox) profiling to eliminate compounds with obvious pharmacological liabilities early in the discovery process [47].
Experimental Design and Validation for HTS
HTS Assay Formats and Selection
Choosing the appropriate assay format is fundamental to a successful HTS campaign. The two primary approaches are detailed in the table below.
Table 1: Comparison of High-Throughput Screening Assay Formats
| Assay Type | Description | Examples | Key Readouts |
|---|---|---|---|
| Biochemical Assays | Measure direct enzyme or receptor activity in a defined, cell-free system [46]. | Enzyme activity (e.g., kinase, ATPase), receptor binding [46]. | Enzyme velocity (ICâ‚…â‚€), binding affinity (Kd), signal intensity. |
| Cell-Based Assays | Capture pathway effects, phenotypic changes, or viability in living cells [46]. | Reporter gene assays, cell viability, second messenger signaling, high-content imaging [46]. | Phenotypic changes, cell proliferation, fluorescence/luminescence intensity. |
Biochemical assays, such as BellBrook Labs' Transcreener platform, provide highly quantitative, interference-resistant readouts for specific enzyme classes like kinases, ATPases, and GTPases [46]. Cell-based phenotypic screens, on the other hand, are useful for comparing several compounds to find the one that results in a desired phenotype, such as altered cell growth [46].
Key Performance Metrics for HTS Assays
A successful HTS assay must balance sensitivity, reproducibility, and scalability. The following workflow outlines the key stages in library screening and hit validation, incorporating essential validation metrics.
Diagram 1: HTS Screening and Validation Workflow
Critical parameters for assay validation, as shown in the workflow, include [46]:
- Z'-factor: A statistical measure of assay robustness and quality. A value between 0.5 and 1.0 is considered excellent for HTS [46].
- Signal-to-Noise Ratio (S/N): Indicates the strength of the measured signal relative to background noise.
- Coefficient of Variation (CV): Measures the reproducibility of replicates across wells and plates, with lower values indicating higher precision.
- Dynamic Range: The difference between the maximum and minimum signals of an assay, which must be sufficient to distinguish active from inactive compounds clearly.
Detailed Experimental Protocol: Biochemical HTS for Enzyme Inhibitors
The following protocol is adapted from a study that discovered aldolase A (ALDOA) inhibitors via an enzymatic coupling reaction, suitable for HTS [48].
Objective: To identify potent inhibitors of a target enzyme (e.g., ALDOA) from a compound library using a biochemical HTS assay. Key Reagents and Materials:
- Purified target enzyme (e.g., ALDOA).
- Enzyme substrate (e.g., Fructose-1,6-diphosphate (FBP) for ALDOA).
- In-house or commercially sourced compound library.
- Assay plates (384-well or 1536-well format).
- Detection reagents for the enzymatic coupling reaction.
Procedure:
- Assay Miniaturization and Dispensing:
- Dispense assay buffer into low-volume, non-binding surface microplates (384-well or 1536-well format) using automated liquid handlers.
- Transfer nanoliter volumes of compounds from the library into the assay plates using acoustic dispensing or pintool transfer.
- Add the purified target enzyme to all wells except negative controls.
Pre-incubation and Reaction Initiation:
- Centrifuge plates briefly to ensure all liquid is at the bottom of the wells.
- Pre-incubate the enzyme with compounds for a fixed time (e.g., 15-30 minutes) to allow for binding.
- Initiate the enzymatic reaction by adding the substrate. For the ALDOA assay, this involves adding FBP [48].
Coupled Detection System:
- The primary reaction is coupled to a secondary, detectable reaction. In the case of ALDOA, the production of glyceraldehyde-3-phosphate (GAP) is linked to the consumption of NADH, which is monitored by a decrease in fluorescence or absorbance [48].
- Incubate the plate for a predetermined time under optimal temperature conditions (e.g., 37°C) for the reaction to proceed.
Signal Measurement:
- Read the plate using an appropriate HTS-compatible detector (e.g., a plate reader capable of measuring fluorescence polarization (FP), fluorescence intensity (FI), TR-FRET, or absorbance).
- The decrease in NADH signal is directly proportional to ALDOA activity [48].
Data Analysis and Hit Selection:
- Normalize the raw data to positive (no compound) and negative (no enzyme) controls present on each plate.
- Calculate the percentage of inhibition for each compound.
- Set a threshold for hit selection (e.g., >50% inhibition at the test concentration).
- Compounds passing this threshold are selected for the next stage of confirmation.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for HTS
| Item | Function in HTS | Key Features |
|---|---|---|
| Curated Compound Libraries | Source of small molecules to be screened for activity against a target [46] [47]. | Drug-like filters applied, target-class enrichment, available from commercial vendors or aggregators. |
| Microplates | The physical platform for miniaturized, parallel reactions [46]. | Available in 96-, 384-, 1536-well formats; surface chemistry optimized for biochemical or cell-based assays. |
| Automation & Robotics | Enable precise, high-speed liquid handling and plate processing [46]. | Pipetting systems, plate washers, and stackers for unattended operation and increased throughput. |
| HTS-Compatible Detection Kits | Provide the biochemical means to quantify the reaction outcome [46]. | Robust, homogeneous (e.g., "mix-and-read") assays (e.g., Transcreener) using FP, TR-FRET, or luminescence. |
| Plate Reader | Instrument to detect the signal generated in the assay [46]. | Capable of reading one or more modalities (e.g., fluorescence, luminescence, absorbance) in multi-well format. |
| BIO 1211 | BIO 1211, CAS:192390-59-3, MF:C36H48N6O9, MW:708.8 g/mol | Chemical Reagent |
| G-418 disulfate | G-418 disulfate, CAS:49662-05-7, MF:C20H44N4O18S2, MW:692.7 g/mol | Chemical Reagent |
Post-HTS Analysis and Hit Progression
Once a primary HTS is complete, identified "hits" must be rigorously validated and characterized to prioritize leads for further optimization.
Hit Triage and Confirmation
- Dose-Response Analysis: Confirm dose-dependent activity of primary hits by generating concentration-response curves to determine the half-maximal inhibitory concentration (ICâ‚…â‚€), a measure of compound potency [46].
- Counter-Screens: Eliminate false positives by testing hits in orthogonal assays (e.g., a different detection technology) and against unrelated targets to assess selectivity.
- Structure-Activity Relationship (SAR) Analysis: Explore the relationship between the chemical structure of a molecule and its biological activity by testing structurally related analogues. This helps to confirm that the observed activity is specific and can be optimized [46].
Advanced Characterization
- Affinity Measurements: Use techniques like Surface Plasmon Resonance (SPR) to determine the binding affinity (dissociation constant, Kd) between the compound and the target protein, as demonstrated in the ALDOA inhibitor study [48].
- Mechanism of Action Studies: Conduct enzyme kinetics experiments to determine the inhibitor's mode of action (e.g., competitive, non-competitive, uncompetitive) [48].
- Cellular Activity Assessment: Verify that the compound is active in a cellular context, which is crucial for confirming target engagement and functional activity in a more physiologically relevant environment.
Building a high-quality compound library is a strategic investment that lays the foundation for a successful HTS campaign and the entire drug discovery pipeline. By rigorously applying principles of compound quality, chemical diversity, and druggability during library curation, researchers can significantly reduce late-stage attrition and increase the efficiency of bringing new medicines to patients. The integration of well-validated experimental protocols, robust performance metrics, and strategic post-HTS analysis creates a powerful, data-driven framework for identifying and advancing the most promising therapeutic candidates.
High-throughput screening (HTS) represents an automated, robust paradigm for rapidly testing thousands to millions of biological, genetic, chemical, or pharmacological samples [1]. This approach has become indispensable in both basic and translational research, particularly in accelerating the drug discovery process during public health emergencies such as the COVID-19 pandemic [49]. The core of HTS methodology involves leveraging liquid handling devices, robotics, sensitive detectors, and data processing software to conduct miniaturized assays in 96-, 384-, or 1536-well microplates [50] [1]. The ultimate success of HTS depends on developing assays that are robust, reproducible in miniaturized formats, exhibit low false-positive rates, and can identify drugs that offer significant improvements over existing therapies [50]. While HTS offers the distinct advantage of rapidly identifying potential hits (10,000–100,000 compounds per day), it also presents challenges including substantial costs, technical complexity, and the potential for false positives and negatives that require sophisticated triage approaches [1].
Table 1: Key Components of a High-Throughput Screening Workflow
| Component | Description | Common Technologies/Formats |
|---|---|---|
| Sample & Library Preparation | Preparation of combinatorial libraries for testing against biological targets | 96- to 1536-well microplates; split-mix combinatorial libraries [1] |
| Assay Development | Design of biologically relevant, miniaturized assays | Biochemical (e.g., FRET, FCS) and cell-based (e.g., reporter, proliferation) assays [50] [1] |
| Automation & Robotics | Automated systems for liquid handling and plate transfer | Liquid handling robots, nanoliter dispensers, integrated robotic workstations [1] [39] |
| Detection Technologies | Systems for reading assay results | Fluorescence, luminescence, mass spectrometry, differential scanning fluorimetry [1] |
| Data Management & Analysis | Software and algorithms for processing large datasets | Cheminformatics, machine learning models, statistical QC methods for outlier detection [1] |
HTS in Antiviral Drug Discovery: Targeting SARS-CoV-2
Case Study 1: Identification of Novel 3CLpro Inhibitors for COVID-19
The COVID-19 pandemic underscored the critical importance of accelerating drug discovery processes. The 3-chymotrypsin-like protease (3CLpro or Mpro) of SARS-CoV-2, a critical enzyme in viral replication, quickly emerged as a prime target for drug development [49]. A significant HTS study leveraged a library of 325,000 compounds, leading to the discovery of two new chemical scaffolds with selective inhibitory activity against 3CLpro [49]. Further experimental validation and in-silico analysis revealed distinct mechanisms of action: one compound acted as a covalent inhibitor targeting the catalytic pocket, while two others functioned as allosteric inhibitors affecting the monomer/dimer equilibrium of 3CLpro, a key requirement for its enzymatic activity [49]. The identified compounds demonstrated significant antiviral activity in vitro, effectively reducing SARS-CoV-2 replication in VeroE6 and Calu-3 cell lines [49]. This study highlights the potential of combining HTS with computational approaches to rapidly identify effective antiviral agents during medical emergencies.
Experimental Protocol: HTS for 3CLpro Inhibitors
- Target: SARS-CoV-2 3CLpro (Mpro), essential for viral polyprotein processing.
- Library: 325,000 structurally diverse compounds.
- Assay Type: Biochemical assay monitoring protease activity.
- Hit Identification: Compounds showing significant inhibition of 3CLpro enzymatic activity.
- Secondary Validation:
- Antiviral efficacy in VeroE6 and Calu-3 cell lines infected with SARS-CoV-2.
- Cytotoxicity assessment to determine selective index.
- In-silico analysis (docking) to elucidate binding modes and mechanisms.
- Mechanism Elucidation: Distinguished between covalent catalytic inhibitors and allosteric dimerization disruptors [49].
Case Study 2: A Strategy for Broad-Spectrum Coronavirus Inhibitors
Given the recurring emergence of coronaviruses, researchers have developed an innovative HTS strategy to identify broad-spectrum drugs. This approach utilizes two milder coronaviruses, HCoV-OC43 and mouse hepatitis virus (MHV), which can be handled outside of high-level biocontainment (BSL-3) facilities required for SARS-CoV-2 [51]. These viruses share extensive homology in essential functional domains with SARS-CoV-2, including the highly conserved RNA-dependent RNA polymerase (RdRp), RNA helicase, and 3CLpro [51].
Experimental Protocol: Broad-Spectrum Antiviral Screening
- Engineered Viruses: HCoV-OC43 and MHV incorporating a luciferase reporter gene to quantitatively indicate viral activity.
- Screening Process:
- Large-scale compound libraries screened against both reporter viruses.
- Antiviral efficiency quantified by measuring luciferase activity.
- Lead selection prioritized compounds effective against both viruses to reduce false positives.
- Hit-to-Lead Optimization: Selected leads undergo structural modification and optimization.
- Validation: Optimized compounds evaluated for efficacy against authentic SARS-CoV-2 in BSL-3 laboratories [51].
This surrogate virus system allows for true high-throughput screening of large compound collections, providing a rapid and cost-effective pathway to identify promising broad-spectrum antiviral candidates for further development [51].
Diagram 1: Workflow for broad-spectrum antiviral HTS. This strategy uses safer surrogate viruses for primary screening before BSL-3 validation [51].
HTS in Anticancer Drug Discovery
Case Study 1: Genome-Wide Association of Anticancer Drug Response
To systematically investigate the role of human genetic variation in anticancer drug response, researchers conducted one of the largest LCL screens to date, profiling 44 FDA-approved anticancer drugs across 680 lymphoblastoid cell lines (LCLs) from the 1000 Genomes Project [52]. This innovative approach combined HTS with genome-wide association studies (GWAS) to identify germline genetic variants influencing drug susceptibility. The drug panel represented nine major chemotherapeutic classes, plus a paclitaxel + epirubicin combination therapy commonly used for breast cancer [52].
The GWAS analysis identified several significant associations, most notably implicating the NAD(P)H quinone dehydrogenase 1 (NQO1) gene in the dose-response to multiple drugs, including arsenic trioxide, erlotinib, trametinib, and the paclitaxel + epirubicin combination [52]. While NQO1 was previously known as a biomarker for epirubicin response, this study revealed novel associations with these additional treatments. Functional follow-up demonstrated that baseline gene expression of NQO1 was positively correlated with drug resistance for 43 of the 44 treatments surveyed, suggesting NQO1 expression may be a general marker of increased resilience to chemotherapeutic agents [52].
Table 2: Key Findings from GWAS of 44 Anticancer Drugs in 680 LCLs [52]
| Analysis Category | Findings | Implications |
|---|---|---|
| Screening Scale | 44 FDA-approved drugs; 680 LCLs; 6 doses per drug | Largest LCL screen for anticancer drug response to date |
| Primary Hit | NQO1 gene associated with response to multiple drugs | Suggests a common mechanism influencing resistance to diverse agents |
| Functional Correlation | Baseline NQO1 expression correlated with resistance to 43/44 drugs | NQO1 may serve as a general biomarker for chemoresistance |
| Prioritized Drug Associations | Arsenic trioxide, erlotinib, trametinib, paclitaxel + epirubicin | Reveals novel therapeutic areas for NQO1 targeting |
| Proposed Clinical Application | Suppressing NQO1 expression to increase drug sensitivity | Potential combination therapy strategy to overcome resistance |
Experimental Protocol: HTS-GWAS Integration for Cancer Pharmacogenomics
- Cell Model: 680 LCLs from the 1000 Genomes Project (representing human germline genetic diversity).
- Drug Treatment: 44 anticancer drugs at six concentrations each to establish dose-response curves.
- Phenotyping: High-throughput cell viability assessment to quantify cytotoxic response for each drug-cell line pair.
- Genotyping: Genome-wide SNP data from the 1000 Genomes Project.
- Association Analysis: GWAS to identify genetic variants correlated with drug response phenotypes.
- Functional Validation:
- Gene expression analysis (NQO1 baseline and drug-induced).
- Interrogation of functional mechanisms linking genetic variants to drug response [52].
Case Study 2: The ATAD5-Luciferase Assay for Genotoxin Discovery
The ATAD5-luciferase HTS assay represents a sophisticated cell-based screening platform that exploits the stabilization of the ATAD5 protein following DNA damage [50]. This assay is particularly robust and reproducible in a 1536-well plate format, demonstrating high specificity for genotoxic compounds. In a pilot screen of approximately 4,000 small molecules, the ATAD5-luciferase assay successfully identified three potential chemotherapeutic agents—resveratrol, genistein, and baicalein—that offered potential improvements over conventional cancer drugs [50]. These compounds, all antioxidants, demonstrated the ability to kill rapidly dividing cells without inducing mutagenesis or chromosomal alterations, side effects that often make cells more resilient to apoptosis [50]. Based on this success, the assay was subsequently used to screen a collection of 300,000 chemical probes, generating hundreds of additional hits for further development [50].
Diagram 2: ATAD5-luciferase assay principle. This cell-based HTS identifies genotoxic compounds through a DNA damage-responsive reporter system [50].
Experimental Protocol: ATAD5-Luciferase HTS for Genotoxins
- Assay Principle: Engineered cell line where luciferase expression is controlled by the ATAD5 promoter, which is induced by DNA damage.
- Screening Format: 1536-well microplates for ultra-high-throughput capacity.
- Readout: Luminescence signal quantification proportional to DNA damage response.
- Hit Selection: Compounds inducing significant luminescence increase over controls.
- Counter-Screening:
- Assessment in DNA-repair-deficient chicken DT40 cell lines (Polymerase β, Rev3, XPA, FANCC, Ku70/Rad54, ATM mutants).
- Evaluation in human tumor cell lines impaired in MSH2 expression (mismatch repair deficiency) [50].
- Advantage: Identifies compounds that kill cancer cells without causing mutations that could lead to resistance.
Essential Research Reagent Solutions for HTS
The successful implementation of HTS campaigns relies on a standardized toolkit of research reagents and platforms. The table below details key solutions referenced in the featured case studies.
Table 3: Essential Research Reagent Solutions for HTS in Drug Discovery
| Reagent/Solution | Function in HTS | Application Examples |
|---|---|---|
| Reporter Cell Lines | Engineered cells that produce a detectable signal upon target engagement or pathway activation | Luciferase-expressing HCoV-OC43/MHV for antiviral screening [51]; ATAD5-luciferase for genotoxin identification [50] |
| Diverse Compound Libraries | Collections of chemically diverse molecules for screening against biological targets | Library of 325,000 compounds for 3CLpro inhibitor discovery [49]; 300,000 chemical probes for ATAD5 screening [50] |
| Fluorogenic Peptide Substrates | Protease substrates that release fluorescence upon cleavage, enabling enzymatic activity monitoring | FRET-based substrate (Dabcyl-KTSAVLQ/SGFRKME-Edans) for SARS-CoV-2 Mpro activity inhibition assays [53] |
| Specialized Microplates | Miniaturized assay containers with well densities from 96 to 1536 for high-throughput testing | 1536-well plates for ATAD5-luciferase assay [50]; standard format for uHTS [1] |
| Automated Liquid Handling Systems | Robotics for precise nanoliter-scale dispensing of reagents and compounds | Essential for uHTS achieving >300,000 assays per day [1]; automated pipetting stations [39] |
The featured case studies demonstrate the powerful application of HTS across both antiviral and anticancer drug discovery domains. The successful identification of novel 3CLpro inhibitors for SARS-CoV-2 and the establishment of broad-spectrum coronavirus screening platforms highlight how HTS methodologies can be rapidly deployed against emerging viral threats [49] [51]. In oncology, the integration of HTS with genome-wide association studies in diverse LCL populations has uncovered important genetic determinants of drug response, such as NQO1, while specialized assays like the ATAD5-luciferase system enable the discovery of novel genotoxic agents with improved safety profiles [50] [52]. As HTS technologies continue to evolve—with advances in automation, miniaturization, and data analysis—their role in accelerating the discovery of effective therapeutic agents will remain indispensable to both basic and translational research. The continued refinement of these platforms, particularly through incorporation of artificial intelligence and machine learning for data analysis, promises to further enhance their efficiency and predictive power in future drug discovery campaigns [54] [1].
Ensuring Success: Robust Assay Design, Quality Control, and Hit Triage
In the domain of high-throughput screening (HTS) for reaction discovery and drug development, the reliability of the assay is the foundation upon which successful campaigns are built. A robust and reproducible assay ensures that the identification of "hits" – compounds with desired activity – is both accurate and efficient. High-throughput screening has become an essential element in modern discovery pipelines, where screening volume is a critical factor given typical hit rates of only approximately 1% [55]. Within this framework, three interconnected concepts are paramount for characterizing assay performance: the signal window, which reflects the assay's dynamic range; robustness, which indicates its consistency; and the Z'-factor, a key metric that quantifies its overall quality and suitability for HTS. This guide provides an in-depth technical examination of these core principles, equipping researchers with the knowledge to develop, optimize, and validate assays that generate trustworthy, high-quality data.
Core Concepts and Quantitative Measures
The Signal Window
The Signal Window (SW), also referred to as the signal-to-background ratio, is a fundamental measure of an assay's dynamic range. It quantifies the separation between the signal produced in a positive control (e.g., a reaction with full enzyme activity) and the signal from a negative control (e.g., a reaction with no enzyme or a fully inhibited enzyme).
- Definition and Calculation: The signal window is typically calculated using the formula: [ \text{Signal Window (SW)} = \frac{|\mup - \mun|}{\sqrt{\sigmap^2 + \sigman^2}} ] where (\mup) and (\mun) are the mean signals of the positive and negative controls, and (\sigmap) and (\sigman) are their respective standard deviations. This formulation accounts for both the separation of means and the variability of the data.
- Interpretation: A larger signal window indicates a greater distinction between the positive and negative states, making it easier to reliably distinguish active compounds from inactive ones. An assay with a small or narrow signal window is more susceptible to noise, leading to potential false positives and false negatives.
The Z'-factor
The Z'-factor is a standardized metric that has become the gold standard for evaluating the quality and robustness of high-throughput screening assays. It integrates both the assay's dynamic range (signal window) and the data variability associated with the positive and negative controls [56].
- Definition and Calculation: The Z'-factor is defined by the following equation: [ Z'\text{-factor} = 1 - \frac{3(\sigmap + \sigman)}{|\mup - \mun|} ] where (\mup) and (\mun) are the mean signals of the positive and negative controls, and (\sigmap) and (\sigman) are their standard deviations.
- Interpretation and Benchmarking: The value of the Z'-factor provides a clear assessment of assay quality:
- (Z' \geq 0.5): An excellent assay suitable for HTS.
- (0 < Z' < 0.5): A marginal assay that may require optimization.
- (Z' \leq 0): An unacceptable assay where the positive and negative control signals overlap significantly.
The Z'-factor is recommended as the preferred measure of assay performance for screening assays because it provides a single, interpretable value that captures both the assay signal and the associated noise [56].
Assay Variability Ratio (AVR)
While the Z'-factor is the most widely adopted metric, the Assay Variability Ratio (AVR) is another measure used for similar purposes. A direct comparison of their mathematical properties and sampling behavior led to the recommendation of the Z'-factor as the more robust and informative statistic for screening applications [56].
Comparative Analysis of Performance Measures
The table below summarizes the key characteristics, advantages, and limitations of the primary assay performance measures.
Table 1: Comparison of Primary Assay Performance Measures
| Measure | Formula | Key Advantage | Primary Limitation | ||
|---|---|---|---|---|---|
| Signal Window (SW) | ( SW = \frac{ | \mup - \mun | }{\sqrt{\sigmap^2 + \sigman^2}} ) | Provides a signal-to-noise ratio that is intuitive. | Does not define a standardized quality threshold for HTS suitability. |
| Z'-factor | ( Z' = 1 - \frac{3(\sigmap + \sigman)}{ | \mup - \mun | } ) | Integrates dynamic range and variability into a single, standardized metric; excellent for HTS qualification [56]. | Less informative for concentration-response assays. |
| Assay Variability Ratio (AVR) | Details of formula compared in source material | Serves a similar purpose to the Z'-factor. | Based on comparative studies, is not the recommended preferred measure [56]. |
Experimental Protocols for Assay Validation
A rigorous assay validation protocol is essential to generate reliable data for calculating the Z'-factor and other performance metrics.
Protocol for Determining Z'-factor
This procedure outlines the steps to experimentally determine the Z'-factor of a developed assay.
- Plate Selection: Use a standard assay microplate (e.g., 96-well or 384-well).
- Control Dispensing:
- Dispense the positive control (e.g., a reaction with a known active enzyme) into a minimum of 16 wells, distributed across the plate to capture positional effects.
- Dispense the negative control (e.g., a reaction with a blank buffer or a fully inhibited enzyme) into a minimum of 16 wells, similarly distributed.
- Assay Execution: Run the entire assay according to the established protocol, including all incubation and reading steps.
- Data Collection: Measure the raw signal from every well using the appropriate detector (e.g., plate reader for absorbance, fluorescence, or luminescence).
- Statistical Analysis: For the positive and negative control data sets, calculate:
- The mean signal ((\mup) and (\mun))
- The standard deviation ((\sigmap) and (\sigman))
- Calculation: Input these values into the Z'-factor formula to obtain the final score.
Workflow for Assay Development and Validation
The following diagram illustrates the logical workflow from initial assay development through to final validation and deployment in a high-throughput setting.
Diagram 1: Assay Development and Validation Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
The reliability of an assay is dependent on the quality and appropriateness of its components. The following table details key reagents and materials essential for robust assay development.
Table 2: Key Research Reagent Solutions for Assay Development
| Item | Function in Assay Development | Application Notes |
|---|---|---|
| Purified Enzyme/Target | The core biological component whose activity is being measured. | Source from commercial vendors, recombinant expression, or native purification; purity and activity are critical [57]. |
| Substrates & Cofactors | Reactants and molecules required for the enzymatic reaction to proceed. | Selection of native vs. analog substrates depends on the readout; concentration must be optimized (e.g., around Km) [57]. |
| Detection Reagents | Dyes, probes, or reporters that generate a measurable signal (absorbance, fluorescence, luminescence). | Choice depends on required sensitivity and susceptibility to interference from compound libraries [57]. |
| Positive Control | A known activator or a system component that gives a maximum signal response. | Enables normalization between plates and defines the upper assay boundary for Z'-factor calculation [57]. |
| Negative Control | An inactive sample (e.g., no enzyme, inactivated enzyme) that defines the baseline signal. | Essential for defining the lower assay boundary and for calculating the signal window and Z'-factor. |
| Buffer Components | Maintain the pH, ionic strength, and chemical environment for optimal and consistent target activity. | Must be optimized for the specific target; can include stabilizers like BSA to prevent non-specific binding. |
| HS014 | HS014, MF:C71H94N20O17S2, MW:1563.8 g/mol | Chemical Reagent |
Advanced Applications in Reaction Discovery Research
The principles of robust assay development are directly applicable to cutting-edge research in reaction discovery. Modern approaches are increasingly reliant on High-Throughput Experimentation (HTE), which involves performing hundreds to thousands of miniature, parallel chemical reactions to empirically determine optimal conditions or to explore reaction scope [58]. For instance, recent work has generated comprehensive data sets encompassing thousands of novel chemical reactions, serving as the foundation for training deep learning models to predict reaction outcomes [58]. In such workflows, the "assay" may be a analytical method (e.g., UPLC-MS) used to quantify reaction yield or success. The reproducibility and low variability of this readout across a large plate are crucial for generating high-quality training data. A high Z'-factor in this context would indicate that the analytical method can reliably distinguish between successful and unsuccessful reactions, thereby enabling accurate model prediction and the identification of optimal, generalizable reaction conditions for drug discovery. This synergy between robust experimental design and data science is accelerating the critical hit-to-lead optimization phase in medicinal chemistry [58].
In the realm of high-throughput screening (HTS) for reaction discovery and drug development, the integrity of data is paramount. Systematic errors, particularly those related to spatial positioning within microplates, represent a significant challenge to data quality and the validity of screening outcomes. Unlike random errors that produce measurement noise, systematic errors introduce consistent biases that can lead to both false-positive and false-negative results, thereby critically impacting the hit selection process [59]. Among these, edge effects and plate position artifacts are prevalent issues, where the physical location of a well on a microplate—most commonly the peripheral wells—significantly influences the measured signal, independent of the actual biological or chemical reaction [60] [61]. This technical guide examines the origins of these artifacts, provides methodologies for their detection and quantification, and outlines robust strategies for their mitigation, all within the broader framework of ensuring robust and reproducible HTS principles.
Mechanisms and Causes of Edge Effects
Edge effects refer to the systematic discrepancy in assay measurements between the outer wells and the inner wells of a microplate. This phenomenon is not attributable to a single cause but is the result of several interconnected physical and environmental factors.
- *Evaporation:* The primary driver of edge effects is the differential evaporation of solvent from the wells. The outer wells of a microplate have a higher surface-to-volume ratio exposed to the ambient environment of the incubator or workstation. This leads to faster evaporation in these wells compared to the more sheltered inner wells [60]. Consequently, the concentration of solutes increases in the outer wells over time, which can amplify or suppress signals and lead to inaccurate readings.
- *Temperature Gradients:* Microplates incubated in COâ‚‚ incubators can experience uneven heating. Wells on the edge of the plate may cool or heat more rapidly than those in the center, leading to temperature gradients across the plate. These gradients can affect enzymatic reaction rates, cell growth, and other temperature-sensitive assay components [60] [59].
- *Cell Distribution Inconsistencies (for Cell-Based Assays):* In cell-based assays, a key factor contributing to edge effects is the uneven distribution of cells in peripheral wells. Research has demonstrated that when newly seeded plates are placed directly into a 37°C CO₂ incubator, evaporation at the plate's edge creates convective currents. These currents cause cells to settle unevenly, often in a crescent or donut pattern at the well periphery, which directly impacts the uniformity of the measured signal [61].
Other contributing factors include variations in gas exchange (e.g., COâ‚‚ levels affecting pH in cell culture media) and meniscus effects during liquid handling, which can be more pronounced at the edges of the plate. The cumulative impact of these factors is a systematic over- or under-estimation of activity in specific well locations, which can obscure true biological activity and compromise the screening campaign [60] [59].
Detecting and Quantifying Spatial Artifacts
The first step in combating spatial artifacts is their rigorous detection and quantification. This involves both visual analytical tools and statistical methods.
Hit Distribution Surface Analysis
A powerful visual method for identifying location-dependent biases is the analysis of a hit distribution surface. After an initial hit selection process using a predefined threshold (e.g., μ - 3σ for an inhibition assay), the number of hits for each well location (e.g., A1, A2, ... P24) across all screened plates is computed and visualized. In an ideal, error-free screen, hits are expected to be randomly and evenly distributed across all well locations. The presence of striking patterns—such as an overabundance of hits in specific rows, columns, or particularly around the edges—provites strong evidence of a systematic artifact affecting the assay [59].
Statistical Methods for Error Detection
Quantitative statistical tests are essential to confirm the presence of systematic errors objectively. The following methods have been validated for this purpose:
- *Two-Way Median Polish (B-Score Normalization):* This robust method, introduced by researchers at Merck Frosst, is used to account for row and column effects within a plate. The process involves fitting a model that estimates the overall plate median, a row effect offset, and a column effect offset. The residuals from this model represent the data with the systematic row and column biases removed. These residuals are then normalized by their median absolute deviation (MAD) to generate B-scores. The presence of significant row or column effects in the initial model is a direct indicator of systematic spatial artifacts [59] [62].
- *Plate Drift Analysis:* This involves running control plates over an extended period, mimicking the duration of a full screening campaign. The signal window and key assay metrics (like Z'-factor) are monitored over time. A significant temporal drift in these metrics indicates systematic errors related to instrument warm-up, reagent degradation, or environmental shifts that can correlate with plate position in a run [60].
- *Hypothesis Testing (e.g., Student's t-test):* Formal statistical tests can be applied to compare data from different plate zones. For instance, a t-test can be used to compare the mean signal of all edge wells against the mean signal of all inner wells. A statistically significant difference (e.g., p-value < 0.05) confirms the presence of a measurable edge effect [59].
Table 1: Key Statistical Metrics for Assessing Spatial Artifacts
| Metric/Method | Calculation/Description | Interpretation | ||
|---|---|---|---|---|
| Hit Distribution Map | Visual plot of hit frequency per well location. | Patterns (rows, columns, edges) indicate systematic error. | ||
| Two-Way Median Polish | residual = raw_value - (plate_median + row_effect + column_effect) |
Significant row or column effects confirm spatial bias. | ||
| B-Score | residual / MAD(residuals) |
Normalized data with spatial effects removed; values > | 3 | may be hits. |
| Edge vs. Inner t-test | Compares mean signals of edge and inner wells. | A significant p-value (p < 0.05) confirms an edge effect. | ||
| Z'-Factor | `1 - [3*(σpositive + σnegative) / | μpositive - μnegative | ]` | Measures assay quality; affected by increased variance from edge effects. |
Experimental Mitigation Strategies
Once detected, spatial artifacts can be mitigated through a combination of practical laboratory techniques and clever experimental design.
Environmental and Procedural Controls
- *Pre-Incubation at Room Temperature:* A simple and highly effective technique for reducing edge effects in cell-based assays is to pre-incubate newly seeded plates at room temperature in ambient air for a period (e.g., 1 hour) before transferring them to the 37°C CO₂ incubator. This allows the cells to settle evenly to the bottom of the well before the temperature- and evaporation-driven convective currents begin, resulting in a more uniform cell distribution [61].
- *Humidity and Temperature Control:* Using incubators with precise humidity control (often >80-90% relative humidity) is critical to minimize solvent evaporation. Furthermore, ensuring the incubator is properly calibrated and maintains a uniform temperature throughout its chamber is essential to prevent thermal gradients [60].
- *Use of Low-Profile Plates and Seals:* Employing microplates with fitted lids and using adhesive seals, particularly during long-term incubation or storage, creates a physical barrier that drastically reduces evaporation from all wells, with the most pronounced benefit for the outer wells [60].
Plate Layout and Assay Design
- *Strategic Placement of Controls:* Instead of clustering controls in a single row or column, distribute positive and negative controls across the entire plate, including the edge wells. This allows for location-specific normalization and makes the assay more robust to spatial biases [60].
- *Edge Well Exclusion or Filling:* In screens with a very high number of compounds where the loss of data points is acceptable, one can simply not use the outermost wells for test compounds, filling them instead with buffer, saline, or control solutions. This physically isolates the test compounds from the most severely affected region.
- *Randomization and Blocking:* For smaller screening sets, randomizing the placement of compounds and replicates across the entire plate can help ensure that spatial biases do not consistently affect the same compounds. Blocking, where an entire plate is dedicated to a single class of compounds or a specific control condition, can also be used to confound the effect.
Diagram: A workflow for the systematic management of spatial artifacts in HTS, integrating procedural, analytical, and corrective steps.
Data Correction and Normalization Techniques
When procedural controls are insufficient, computational post-processing methods can be applied to correct for the identified spatial biases.
- *B-Score Normalization:* As described in Section 3.2, this is a widely adopted method for removing row and column effects. The process involves a two-way median polish on a per-plate basis, followed by normalization of the residuals by the median absolute deviation (MAD). The resulting B-scores are effectively the data with the spatial biases removed, allowing for a more accurate hit identification based on the residual biological activity [59] [62].
- *Well Correction:* This is a more aggressive correction technique designed to remove systematic biases affecting specific well locations across all plates in an entire assay. It involves two main steps: a least-squares approximation is performed separately for each unique well location (e.g., well A1 across all plates), followed by a Z-score normalization of the data within each of these well locations. This method is particularly powerful for correcting persistent, location-specific errors but should be used with caution as it can introduce bias in error-free data [59].
- *Control-Based Normalization (Percent Inhibition/Activation):* This method uses the control wells distributed across the plate to normalize the data. The formula
(x_ij - μ_neg) / (μ_pos - μ_neg)is often used, where xij is the raw measurement in well (i,j), μneg is the mean of negative controls, and μ_pos is the mean of positive controls. When controls are strategically placed, this can correct for localized drifts [59].
Table 2: Research Reagent Solutions for Managing Spatial Artifacts
| Reagent / Material | Primary Function | Utility in Mitigating Edge Effects |
|---|---|---|
| Humidified COâ‚‚ Incubators | Provides stable temperature, COâ‚‚, and humidity for cell culture. | High humidity (>80%) is critical to minimize solvent evaporation from all wells, especially edge wells. |
| Adhesive Plate Seals / Fitted Lids | Creates a physical seal over the microplate. | Directly reduces evaporation by limiting air exchange over the well, protecting edge wells most. |
| Low-Evaporation Microplates | Microplates designed with specialized well geometry or materials. | Minimizes the surface-to-volume ratio or uses materials that reduce evaporative loss. |
| Pre-Dispensed Control Compounds | Stable control compounds plated across the microplate. | Enables location-specific normalization (e.g., percent inhibition) to correct for spatial biases. |
| Echo-Qualified Plates / Acoustic Dispensing Fluid | Enables non-contact, nanoliter-volume liquid transfer. | Reduces volumetric errors in miniaturized assays where edge effects are more pronounced. |
Validating Assay Robustness
Before initiating a full-scale screening campaign, it is imperative to validate that the implemented mitigation and correction strategies have successfully rendered the assay robust to spatial artifacts.
The Z'-factor is a critical statistical parameter used for this purpose. It is calculated as follows:
Z' = 1 - [3*(σ_positive + σ_negative) / |μ_positive - μ_negative| ]
where σ and μ represent the standard deviation and mean of the positive and negative controls, respectively. An assay is generally considered excellent and robust for screening if the Z'-factor is >0.5, indicating a wide separation between controls and low variability [60].
This validation should be performed under conditions that explicitly test for edge effects. This involves running multiple control plates where all wells contain the same type of control (e.g., all negative controls) and analyzing the data for any residual spatial patterns after correction. The Z'-factor should be calculated separately for the edge wells and the inner wells to ensure it meets the quality threshold in both regions. A successful validation demonstrates that the signal window is stable and that the assay performance is consistent across the entire microplate, from center to edge [60].
In the field of reaction discovery and drug development, high-throughput screening (HTS) serves as a critical method for rapidly evaluating large compound libraries to identify promising starting points for therapeutic development. A major goal of HTS is to select compounds—known as "hits"—that exhibit a desired size of inhibition or activation effects from among thousands or even millions of inactive compounds [63]. The process of identifying these active compounds, termed hit selection, presents significant statistical challenges due to the massive scale of data involved and the need to distinguish true biological signals from assay noise and variability [63]. The reliability of hit selection is fundamentally dependent on two key factors: the difference in behavior between active and inactive compounds (the 'signal window'), and the variation within the data [64]. Intuitively, it becomes easier to identify a hit when there is a large signal window coupled with low variability [64].
Statistical methods for hit selection have evolved considerably to address these challenges, with Z-score and Strictly Standardized Mean Difference (SSMD) emerging as cornerstone techniques. These methods, along with their robust counterparts, provide researchers with powerful tools to quantify effect sizes while accounting for data variability, enabling more reliable identification of true hits amidst the background of experimental noise and artifacts [63] [65]. The application of these methods differs depending on the screening context—whether conducted without replicates (typical in primary screens) or with replicates (typical in confirmatory screens)—requiring researchers to select appropriate statistical approaches for their specific experimental designs [63].
Foundational Statistical Methods for Hit Selection
The Z-score and Z-factor Framework
The Z-score method represents one of the most established statistical approaches for hit selection in primary screens without replicates. This method operates on the principle that measured values of all investigated compounds in a plate typically follow a normal distribution, with true hits appearing as statistical outliers [63]. The Z-score for a compound is calculated as the number of standard deviations its measurement deviates from the plate mean, allowing researchers to identify compounds with unusually high or low activity compared to the population distribution.
A closely related metric, the Z-factor (or Z-value), and its variant Z-prime factor (Z'-value), serve as essential quality control parameters for assessing assay performance [64] [66]. These metrics are defined by the following equations:
Z-prime value (Z') = 1 - [3(σ₊ + σ₋) / |μ₊ - μ₋|]
Z-value (Z) = 1 - [3(σs + σc) / |μs - μc|]
Where μ represents the mean and σ represents the standard deviation of the signals for positive (+) and negative (-) controls, or samples (s) and controls (c) [66].
The key distinction between these parameters lies in their application: Z-prime value evaluates assay quality during validation using only positive and negative controls, while Z-value assesses actual assay performance during or after screening when test samples are included [66]. The following table summarizes the interpretation and application of these Z statistics:
Table 1: Z-Factor Metrics for Assay Quality Assessment
| Parameter | Data Used | Application Context | Interpretation Guidelines |
|---|---|---|---|
| Z-prime value (Z') | Positive and negative controls only | Assay development and validation | Z' > 0.5: Excellent assay [66] |
| Z-value (Z) | Test samples and controls | During or after screening | 0.5-1.0: Excellent performance; 0-0.5: May be acceptable; <0: Assay not usable [66] |
In practice, researchers first optimize assays using Z-prime value to ensure sufficient dynamic range and acceptable signal variability before proceeding to full-scale screening. The Z-value then provides a running assessment of assay performance during the actual screening process [66]. While the Z-prime value > 0.5 has become a widely accepted cutoff for assay quality, it's important to note that this threshold may not be appropriate for all assay types, particularly more variable cell-based assays, requiring a nuanced, case-by-case application [66].
Strictly Standardized Mean Difference (SSMD)
The Strictly Standardized Mean Difference (SSMD) has emerged as a powerful alternative to traditional Z-scores for hit selection, particularly in RNAi HTS experiments [65]. SSMD addresses a key limitation of simpler metrics like fold change or percent inhibition by explicitly incorporating data variability into its calculation [63]. SSMD is defined as the ratio of the mean difference to the variability of the difference, offering a more comprehensive measurement of effect size that accounts for both the magnitude of effect and the noise present in the data.
The calculation of SSMD differs depending on whether replicates are available. For screens without replicates, SSMD is calculated using the same strong assumption as the Z-score method—that every compound has the same variability as a negative reference in a plate [63]. However, for screens with replicates, SSMD can be directly calculated for each compound using the formula:
SSMD = (μs - μc) / √(σs² + σc²)
Where μs and μc represent the sample and control means, and σs and σc represent their standard deviations [63].
SSMD offers several advantages over traditional metrics. The links between SSMD and d+-probability provide a clear probabilistic interpretation of effect sizes, allowing researchers to understand hit quality from a probability perspective [65]. As a ranking metric, SSMD has been shown to be more stable and reliable than percentage inhibition, leading to more robust hit selection results [65]. Importantly, the use of SSMD-based methods can reduce both false-negative and false-positive rates compared to conventional approaches [65].
A particularly powerful application of SSMD involves the dual-flashlight plot, where researchers plot SSMD versus average log fold-change (or average percent inhibition/activation) for all compounds investigated in an experiment [63]. This visualization technique enables simultaneous assessment of both effect size (via SSMD) and magnitude of response (via fold change), helping identify compounds with large differential effects that also demonstrate biologically meaningful response magnitudes [63].
Robust Statistical Counterparts
Traditional statistical methods for hit selection often face challenges when dealing with real-world HTS data, which frequently contains outliers and assay artifacts. Robust statistical counterparts have been developed to address these limitations, providing more reliable hit selection in the presence of data anomalies [63].
The z-score method represents a robust variant of the traditional Z-score approach. While the regular Z-score is sensitive to outliers, the z-score incorporates statistical techniques that are less influenced by extreme values, making it more suitable for HTS data where outliers are not uncommon [63]. Similarly, SSMD* offers a robust version of SSMD that maintains performance even when the data contains artifacts or violates normality assumptions [63].
Additional robust methods include:
- B-score method: A normalization approach that removes systematic row and column effects within assay plates, correcting for spatial patterns that may occur during screening [63].
- Quantile-based method: Utilizes percentiles rather than means and standard deviations, making it less sensitive to extreme values [63].
These robust methods are particularly valuable in primary screens without replicates, where the strong assumption of equal variability across all compounds may not hold true due to the presence of true hits with large effects or strong assay artifacts that behave as outliers [63]. The application of robust methods helps prevent both false positives (from artifacts) and false negatives (from over-conservative statistical approaches), ultimately improving the quality of hit selection decisions.
Table 2: Comparison of Hit Selection Methods for Different Screening Scenarios
| Method | Screen Type | Key Assumptions | Advantages | Limitations |
|---|---|---|---|---|
| Z-score | Without replicates | Normal distribution; Equal variability across compounds [63] | Simple calculation; Easily interpretable | Sensitive to outliers; Depends on strong assumptions [63] |
| SSMD | With or without replicates (different calculations) | Works best under normality [63] | Captures effect size and variability; Better false discovery rate control [65] | May highlight small mean differences with very low variability [63] |
| Robust Methods (z, SSMD, B-score) | Primarily without replicates | Fewer distributional assumptions | Resistant to outliers and artifacts [63] | May require more computational resources |
Experimental Protocols for Hit Selection
Protocol 1: Hit Selection Using Z-score and Z-factor
Purpose: To establish and validate a robust HTS assay using Z-factor analysis, then perform hit selection using Z-scores.
Materials and Reagents:
- Compound library: Typically 0.5-5 million compounds for industrial HTS [3]
- Positive and negative controls: Well-characterized compounds producing maximal and minimal responses
- Assay reagents: Specific to target (e.g., enzymes, cell lines, substrates)
- Microplates: 384-well or 1536-well formats for HTS
- Detection system: Appropriate for assay readout (luminescence, fluorescence, absorbance)
Procedure:
- Assay development phase:
- Test multiple assay conditions to optimize reagents, procedures, kinetics, and instrumentation [66]
- Calculate Z-prime value using only positive and negative controls: Z' = 1 - [3(σ₊ + σ₋) / |μ₊ - μ₋|] [66]
- Iterate optimization until Z' > 0.5 (or establish appropriate threshold for specific assay type) [66]
Primary screening phase:
- Screen compound library without replicates under optimized conditions
- For each compound, calculate Z-score = (xi - μplate) / σplate, where xi is the compound measurement, and μplate and σplate are the mean and standard deviation of all compounds on the plate [63]
- Apply threshold for hit selection (typically Z-score ≥ 2.5 or as determined by desired false discovery rate) [67]
Validation:
- Select hits based on Z-score threshold
- Proceed to confirmatory screening with replicates
Troubleshooting Notes: If Z-prime values are consistently low (<0), reevaluate assay conditions, control compounds, or detection method. For cell-based assays, consider accepting lower Z-prime thresholds due to higher inherent variability [66].
Protocol 2: Hit Selection Using SSMD with Replicates
Purpose: To identify hits with large effects while controlling for variability using SSMD in screens with replicates.
Materials and Reagents:
- Compound library: Typically smaller focused libraries for confirmatory screens
- Controls: Positive, negative, and vehicle controls
- Replication capability: Sufficient materials for multiple tests
Procedure:
- Experimental design:
- Plan for minimum of 3 replicates per compound
- Include controls on each plate to monitor assay performance
Screening execution:
- Test all compounds and controls in replicates across multiple plates
- Randomize compound placement to avoid positional biases
SSMD calculation:
- For each compound, calculate SSMD = (μs - μc) / √(σs² + σc²)
- Where μs and σs are the mean and standard deviation of the sample replicates
- μc and σc are the mean and standard deviation of the negative control replicates [63]
Hit selection:
- Rank compounds by SSMD value
- Apply SSMD threshold for hit selection (context-dependent)
- For additional insight, create dual-flashlight plot: SSMD vs. average log fold-change [63]
False discovery rate control:
- Use SSMD-based testing methods to control false-positive and false-negative rates [65]
Validation: Confirm hits in secondary assays with fresh compounds and concentration-response testing.
Protocol 3: Normalization Across Multiple Screens
Purpose: To enable hit selection across multiple screening batches or libraries when using cell-based phenotypic assays with higher variability.
Materials and Reagents:
- Multiple compound libraries: Screened separately over time
- Standard compound: Producing known concentration-response in the assay
- Control reagents: Consistent across screens
Procedure:
- Screen design:
- Include a standard concentration-response curve on each plate (e.g., IFN-β dose response for interferon signaling assays) [67]
- For each library or batch, maintain consistent plate layout and controls
Data conversion:
- Fit raw data to concentration-response curve on per-plate, per-quadrant basis
- Convert assay readout to effective biological response units (e.g., effective IFN-β concentration) using 4-parameter curve fit: Y = Bottom + (Top - Bottom) / (1 + 10^((LogEC50 - X) * HillSlope)) [67]
Data integration:
- Combine normalized effective response values across all screens
- Apply Z-score transformation to centered, scaled combined data
- Select hits based on maximum combined Z-score across all screens (typically ≥ 2.5) [67]
Hit confirmation:
- Retest selected hits in concentration-response format with fresh compounds
- Validate using orthogonal assay methods when possible
This approach is particularly valuable for cell-based phenotypic screens which often show greater batch-to-batch variability compared to biochemical assays [67].
Visualization of Hit Selection Workflows
Hit Selection Method Decision Framework
The following diagram illustrates the logical decision process for selecting appropriate statistical methods based on screening characteristics:
High-Throughput Screening Triage Workflow
The following workflow diagrams the comprehensive triage process for hit identification and validation in HTS:
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for HTS Hit Selection
| Reagent/Material | Function in HTS | Application Examples | Quality Considerations |
|---|---|---|---|
| Compound Libraries | Source of chemical matter for screening | Diversity libraries, targeted collections, DNA-encoded libraries (DEL) [68] | Filter for PAINS, REOS; assess drug-likeness; ensure structural diversity [3] |
| Positive/Negative Controls | Assay quality assessment and normalization | Known inhibitors/activators, vehicle controls [66] | Well-characterized; produce consistent maximal/minimal responses |
| Detection Reagents | Signal generation for activity measurement | Luciferase reagents, fluorescent probes, colorimetric substrates | High sensitivity; low background; suitable for automation |
| Cell Lines | Biological context for phenotypic screens | Engineered reporter lines, primary cells, disease models | Consistent phenotype/passage number; appropriate controls |
| Microplates | Miniaturized reaction vessels | 384-well, 1536-well formats [66] | Low well-to-well variability; compatible with automation |
| Automation Systems | High-throughput processing | Liquid handlers, plate readers, robotic arms [67] | Precision; reproducibility; minimal cross-contamination |
Advanced Applications and Future Directions
The field of hit selection continues to evolve with emerging technologies and methodologies. DNA-encoded libraries (DELs) represent a promising approach that expands the accessible chemical space for screening [68]. These libraries allow researchers to screen vastly larger compound collections (millions to billions) than traditional HTS, creating new demands for statistical methods that can handle the increased scale and complexity of resulting data.
The integration of medicinal chemistry expertise throughout the HTS triage process has proven essential for successful hit identification [3]. This partnership between biology and chemistry enables more effective discrimination between true hits and problematic chemotypes such as pan-assay interference compounds (PAINS), assay artifacts, and promiscuous bioactive compounds [3]. The triage process involves classifying hits into categories: compounds likely to succeed as probes or tool compounds, those with little chance of success, and those where expert intervention could make a significant difference in outcome [3].
Quantitative HTS (qHTS) approaches, which test compounds at multiple concentrations, present additional opportunities for improved hit selection through curve-fitting and classification algorithms [69]. These methods typically use nonlinear regression models, such as the Hill model, to characterize concentration-response relationships, enabling more sophisticated classification of compounds as active, inactive, or inconclusive [69]. Advanced statistical approaches, including preliminary test estimation and M-estimation procedures, have been developed to handle heteroscedastic data and outliers common in qHTS assays, providing better control of false discovery rates while maintaining good power [69].
As HTS technologies continue to advance, the development of robust statistical methods for hit selection will remain crucial for maximizing the value of screening campaigns and identifying high-quality starting points for reaction discovery and drug development programs.
High-Throughput Screening (HTS) serves as a cornerstone technology in modern drug discovery and reaction research, enabling the rapid assessment of thousands to millions of compounds against biological targets [1]. However, this approach faces a significant challenge: the generation of false positive results that can misdirect research efforts and consume valuable resources. Among these deceptive compounds, Pan-Assay Interference Compounds (PAINS) represent a particularly problematic category. These compounds exhibit activity across multiple disparate assay platforms through interference mechanisms rather than genuine target-specific interactions [3]. The presence of PAINS in screening libraries poses a substantial threat to research validity, as they can generate promising but ultimately irreproducible results, leading research programs down unproductive paths. Recognizing and effectively filtering these compounds is therefore essential for maintaining the integrity and efficiency of HTS campaigns in both drug discovery and reaction research contexts.
The impact of PAINS extends beyond mere inconvenience. In academic settings, where HTS implementation has grown significantly, the lack of dedicated triage expertise can result in the publication and pursuit of artifacts that would typically be flagged in industrial settings [3]. This problem is compounded by the fact that even carefully curated screening libraries contain approximately 5% PAINS, a percentage comparable to the broader universe of commercially available compounds [3]. The dissemination of these false positives through scientific literature perpetuates cycles of wasted research effort, making comprehensive PAINS recognition and filtering strategies an essential component of robust screening methodologies.
Understanding PAINS and Their Mechanisms
Defining Characteristics of PAINS
PAINS are not merely promiscuous inhibitors but represent specific structural classes that consistently produce false positive results across diverse assay formats. These compounds typically function through mechanism-independent interference rather than genuine biological activity [3]. Their behavior stems from intrinsic chemical properties that allow them to disrupt assay systems through non-target-specific interactions. Key characteristics include frequent hitter behavior, where the same structural motif appears as a "hit" in multiple unrelated screens, and assay-specific interference, where the apparent activity disappears when alternative assay formats are employed to validate results.
The problematic nature of PAINS is further compounded by their ability to mimic legitimate structure-activity relationships (SAR), creating the illusion of meaningful biological interaction. Some PAINS may show apparent concentration-dependent responses or even appear to follow expected SAR patterns within congeneric series, making them particularly deceptive to researchers unfamiliar with their behavior. This mimicry capacity underscores the importance of structural recognition and mechanistic understanding in PAINS identification.
Common PAINS Scaffolds and Structural Motifs
Research has identified numerous structural classes that frequently exhibit PAINS behavior. These chemotypes consistently appear as hits across various screening campaigns regardless of the biological target. Table 1 summarizes some of the most prevalent PAINS scaffolds and their characteristic interference mechanisms:
Table 1: Common PAINS Scaffolds and Their Interference Mechanisms
| Scaffold Class | Characteristic Structure | Primary Interference Mechanisms | Additional Notes |
|---|---|---|---|
| Eosin-like compounds | Xanthene derivative | Photoinduced reactivity, membrane disruption | Particularly problematic in fluorescence-based assays |
| Curcuminoids | 1,3-dicarbonyl structure | Redox activity, metal chelation, aggregation | Can appear to have potent activity (low µM) |
| Ene-rhodanines | Thiazolidinedione core | Thiol reactivity, redox cycling | Often exhibit steep SAR, mimicking real hits |
| Quinones | Para- or ortho-quinone | Redox cycling, reactive oxygen species generation | Interference highly dependent on assay conditions |
| Catechols | ortho-dihydroxybenzene | Metal chelation, oxidation to quinones | Can chelate metal cofactors in enzymes |
| Acyl hydrazones | R1-C=N-N-R2 | Schiff base formation, metal chelation | Prone to hydrolysis, reactivity with nucleophiles |
These structural classes represent only a subset of known PAINS, with ongoing research continuing to identify additional problematic chemotypes. The presence of these motifs in screening hits should trigger immediate suspicion and prompt thorough investigation of potential interference mechanisms before proceeding with hit optimization.
Biochemical Mechanisms of Interference
PAINS employ diverse biochemical strategies to generate false positive signals, with specific mechanisms often dependent on both the compound structure and assay methodology. Aggregation-based interference represents one of the most common mechanisms, where compounds form colloidal aggregates that non-specifically sequester proteins, leading to apparent inhibition [1]. These aggregates typically range from 50-1000 nm in size and can be detected through add-on experiments such as detergent addition or dynamic light scattering.
Reactive compound behavior provides another major interference pathway, where PAINS covalently modify protein targets through electrophilic functional groups or generate reactive oxygen species that indirectly impact protein function. This category includes compounds capable of redox cycling, which can deplete essential reducing agents in assay systems or generate oxidative stress conditions that non-specifically impact target activity.
Spectroscopic interference represents a third major category, particularly relevant to optical assay formats. Some PAINS exhibit strong fluorescence at wavelengths used for detection, while others may quench fluorescent signals or absorb light in critical spectral regions. Still other PAINS function as metal chelators, stripping essential metal cofactors from metalloenzymes or creating apparent activity through sequestration of metal impurities in assay buffers.
Experimental Protocols for PAINS Identification
Primary Triage Workflow
The initial identification of potential PAINS should begin immediately after primary screening results are available. Figure 1 illustrates the comprehensive triage workflow that integrates both computational and experimental approaches:
Figure 1: Comprehensive PAINS Triage Workflow Integrating Computational and Experimental Approaches
This workflow emphasizes the sequential application of filters, beginning with computational screening and proceeding through increasingly resource-intensive experimental validation. The decision point represents a critical juncture where triage evidence is comprehensively evaluated before committing to lead optimization efforts.
Orthogonal Assay Validation
The cornerstone of PAINS identification remains experimental validation through orthogonal assay formats. Assay orthogonality refers to the use of fundamentally different detection methodologies to measure compound activity against the same target. A compound exhibiting consistent activity across multiple orthogonal platforms is less likely to represent a PAINS offender than one showing activity in only a single assay format.
Primary orthogonal strategies include transitioning between binding assays (e.g., surface plasmon resonance, thermal shift assays) and functional assays (e.g., enzyme activity, cell-based reporter systems). For example, a hit identified in a fluorescence-based assay should be confirmed using a luminescence-based or absorbance-based format with the same biological target. Similarly, compounds identified in biochemical assays should be evaluated in relevant cell-based systems to confirm target engagement in a more complex biological environment.
Counter-screening approaches provide another valuable orthogonal strategy. These include testing compounds against unrelated targets to assess promiscuity and evaluating activity in reporter systems designed specifically to detect common interference mechanisms. For example, a redox-sensitive reporter system can identify compounds acting through reactive oxygen species generation, while a detergent addition assay can detect aggregation-based inhibitors [1].
Analytical Characterization Methods
Advanced analytical techniques provide powerful tools for identifying specific PAINS mechanisms. Dynamic Light Scattering (DLS) represents the gold standard for detecting compound aggregation, capable of identifying colloidal particles in the 1-1000 nm size range. The protocol involves incubating compounds at screening concentrations in assay buffer and measuring particle size distribution. A significant population of particles in the 50-500 nm range suggests aggregation as a potential interference mechanism.
Mass Spectrometry (MS) methods can detect covalent modification of protein targets by reactive PAINS. Intact protein MS reveals mass shifts corresponding to compound adducts, while tandem MS with proteolytic digestion can identify specific modification sites. The experimental protocol typically involves incubating the protein target with compound under screening conditions, followed by buffer exchange and MS analysis.
Nuclear Magnetic Resonance (NMR) techniques offer additional insights into PAINS behavior, particularly through protein-observed NMR methods that detect compound binding through chemical shift perturbations. The advantage of NMR lies in its ability to detect weak, non-specific binding characteristic of PAINS interactions. NMR can also identify compound reactivity through time-dependent spectral changes and detect aggregation through line-broadening effects.
Computational Filtering Strategies
Cheminformatic Filters and Tools
Computational approaches provide the first line of defense against PAINS, enabling rapid assessment of compound libraries before significant experimental resources are invested. These methods leverage known structural motifs associated with assay interference to flag potentially problematic compounds. Table 2 summarizes key computational tools and their applications in PAINS filtering:
Table 2: Computational Tools for PAINS Identification and Filtering
| Tool/Filter Name | Methodology | Application Context | Access |
|---|---|---|---|
| PAINS Filters | Structural pattern matching | Initial library design, post-HTS triage | Publicly available |
| REOS (Rapid Elimination of Swill) | Multiple parameter filtering | Compound acquisition, library design | Proprietary (Vertex) |
| ZINC Database | Curated commercial compounds | Virtual screening, library design | Publicly available |
| eMolecules | Commercially available compounds | Compound sourcing, library enhancement | Subscription-based |
| GDB-13 | Enumerated virtual compounds | Virtual screening, library design | Publicly available |
| CAS Registry | Comprehensive substance database | Historical compound assessment | Subscription-based |
The implementation of these filters typically begins during library design, where compounds containing PAINS motifs are excluded from screening collections. Post-screening, these tools help prioritize hits for follow-up by flagging those with structural features associated with interference. It is important to note, however, that computational filters should guide rather than replace experimental validation, as they may generate both false positives and false negatives.
Library Design Considerations
Preventing PAINS contamination begins with thoughtful library design and curation. Screening libraries should be constructed with chemical quality as a primary consideration, prioritizing compounds with favorable physicochemical properties and excluding known problematic motifs [3]. The concept of "lead-likeness" informs library design, emphasizing properties associated with successful optimization rather than merely potent activity.
Diversity considerations must be balanced against PAINS risk. While structural diversity increases the probability of identifying novel chemotypes, it also elevates the risk of including unvetted compounds with potential interference properties. This balance can be achieved through scaffold-based representation, where multiple analogues of each scaffold are included to facilitate hit validation through SAR assessment even during initial screening.
Library sourcing decisions significantly impact PAINS content. Commercial compound collections vary considerably in quality, with some suppliers providing pre-filtered libraries while others offer largely unfiltered chemical space. Academic screening centers in particular should prioritize quality over quantity, recognizing that a smaller, well-curated library of 100,000 compounds will typically yield more reliable hits than a larger, poorly filtered collection [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful PAINS identification and filtering requires specific research tools and methodologies. Table 3 catalogues essential reagents and materials utilized in PAINS triage workflows:
Table 3: Essential Research Reagents and Materials for PAINS Investigation
| Reagent/Material | Function in PAINS Triage | Application Examples | Considerations |
|---|---|---|---|
| Non-ionic detergents | Disrupt compound aggregates | Add to assay buffer (0.01% Triton X-100) | Can interfere with some protein targets |
| Redox-sensitive dyes | Detect redox cycling compounds | Counter-screens with DTT, glutathione | Monitor time-dependent signal changes |
| Chelating resins | Remove metal impurities | Pre-incubate compounds with Chelex resin | May strip essential metals from metalloenzymes |
| Thiol-reactive probes | Detect covalent modification | Monitor free thiol depletion | Controls needed for spontaneous oxidation |
| Reference PAINS compounds | Positive controls for interference | Include in assay validation | Commercial sources available |
| Cytotoxicity assays | Distinguish specific from non-specific effects | Cell viability measurements in cell-based assays | Multiple mechanisms can cause toxicity |
| Dynamic Light Scattering (DLS) instruments | Detect compound aggregation | Measure particle size in assay buffer | Requires appropriate concentration ranges |
| Surface Plasmon Resonance (SPR) systems | Detect direct binding | Confirm target engagement | Nonspecific binding can generate false positives |
This toolkit enables researchers to implement the critical counter-screens and validation experiments necessary to distinguish legitimate hits from PAINS. The selection of specific reagents should be guided by the assay technologies employed and the structural characteristics of compounds under investigation.
Addressing the PAINS challenge requires more than technical solutions—it demands a cultural shift in how the scientific community approaches HTS and hit validation. The integration of medicinal chemistry expertise throughout the screening process, from library design to hit triage, represents the most effective strategy for minimizing PAINS-related artifacts [3]. This collaborative approach ensures that biological screening and chemical assessment evolve in parallel rather than sequentially.
The development of standardized reporting practices for HTS results would significantly advance PAINS awareness. Complete disclosure of triage methodologies, including both computational filtering parameters and experimental counter-screens, would enhance result interpretation and facilitate meta-analyses across screening campaigns. Journal policies increasingly mandate this level of methodological transparency, helping prevent the dissemination of PAINS-masked as legitimate discoveries.
Ultimately, recognizing that PAINS identification is an ongoing process rather than a one-time filter is crucial. As new assay technologies emerge, novel interference mechanisms will inevitably be discovered, requiring continuous refinement of PAINS detection strategies. Maintaining curated, community-accessible databases of confirmed PAINS, along with their documented interference behaviors, would accelerate this learning process across the scientific community. Through these integrated technical and cultural approaches, the field can mitigate the false-positive problem posed by PAINS and enhance the efficiency of both drug discovery and reaction research.
In high-throughput screening (HTS) for reaction discovery research, dose-response analysis serves as a critical bridge between initial hit identification and the selection of viable candidates for further development. The shape of the concentration-response (CR) curve provides fundamental insights into the biological activity and potential artifacts associated with small-molecule modulators [70] [71]. Interpreting these curve profiles allows researchers to distinguish between high-quality hits worthy of pursuit and compounds likely to generate false-positive results. Within the framework of HTS principles, rigorous evaluation of curve characteristics represents an essential step in transitioning from primary screening data to confirmed leads with legitimate bioactivity.
The transition from single-concentration screening to multi-point dose-response analysis introduces significant analytical complexity. While primary HTS is typically conducted at a single compound concentration, subsequent dose-response characterization across a broad concentration range enables researchers to generate curves from which crucial parameters like IC₅₀ values can be calculated [70]. The resulting curve shapes—whether steep, shallow, bell-shaped, or classical sigmoidal—provide critical information about compound behavior under physiological conditions. This guide establishes a systematic framework for interpreting these curve profiles within the context of HTS campaign triaging, emphasizing practical troubleshooting methodologies to enhance the efficiency of reaction discovery research.
Interpreting Problematic Curve Profiles
Characteristics and Implications of Different Curve Shapes
Table 1: Characteristic Profiles of Problematic Dose-Response Curves
| Curve Shape | Key Characteristics | Potential Mechanisms | Recommended Actions |
|---|---|---|---|
| Steep Curves | Abrupt transition from minimal to maximal effect; Hill coefficient >>1 [70] | - Compound aggregation [70]- Cytotoxicity [70]- Cooperative binding mechanisms | - Implement aggregation counter-screens- Assess cellular viability- Analyze structure-activity relationships |
| Shallow Curves | Gradual response transition over multiple log units; Hill coefficient <1 [70] | - Poor membrane permeability- Multi-site binding- Metabolic instability- Competing mechanisms | - Evaluate compound stability- Assess pharmacokinetic properties- Consider off-target effects |
| Bell-Shaped Curves | Activity loss at higher concentrations; inverted U-shape profile [70] | - Compound precipitation- Secondary target inhibition- Cytotoxicity at high concentrations- Assay interference | - Check solubility limits- Test for target promiscuity- Examine cellular health endpoints |
Experimental Validation of Curve Anomalies
The process of validating anomalous dose-response curves requires a multifaceted experimental approach. For steep curves, the investigation should prioritize the detection of colloidal aggregates, which represent a common source of false positives in HTS campaigns. Experimental countermeasures include the addition of non-ionic detergents such as Triton X-100 or Tween-20 to the assay buffer, which can disrupt aggregate formation without significantly impacting specific target-compound interactions [70]. Cellular health assessments using viability assays (e.g., CellTiter-Glo, MTT) or cytotoxicity markers (e.g., LDH release) provide essential context for distinguishing true bioactivity from generalized toxicity [70].
For shallow curves, the experimental focus shifts toward understanding compound stability and binding kinetics. Metabolic stability assays using liver microsomes or hepatocyte preparations can identify rapid compound degradation, while surface plasmon resonance (SPR) or isothermal titration calorimetry (ITC) provide direct measurements of binding kinetics and stoichiometry [70]. Bell-shaped curves demand particular scrutiny of solubility limits through light-scattering techniques or direct visualization, coupled with counter-screens against related targets to identify promiscuous inhibition patterns. In all cases, orthogonal assay approaches that employ different readout technologies (e.g., fluorescence replaced by luminescence or absorbance) provide critical validation of observed activities [70].
Experimental Workflows for Curve Interpretation
Integrated Screening Cascade for Hit Triage
Figure 1: Hit Triage Workflow for Problematic Curve Profiles
Orthogonal Assay Selection Matrix
Table 2: Experimental Protocols for Curve Anomaly Resolution
| Curve Anomaly | Primary Assay Technology | Orthogonal Validation Methods | Key Reagent Solutions |
|---|---|---|---|
| Steep Curves | Luminescence viability (CellTiter-Glo) | - Aggregation testing (light scattering)- Cytotoxicity multiplexing (LDH, caspase)- High-content imaging (membrane integrity) | - Non-ionic detergents (Tween-20)- Serum albumin (BSA)- Cell health dyes (propidium iodide) |
| Shallow Curves | Fluorescence intensity binding | - Surface plasmon resonance (SPR)- Isothermal titration calorimetry (ITC)- Metabolic stability (microsomal incubations) | - Cofactor supplements (NADPH)- Protease/phosphatase inhibitors- Permeability enhancers |
| Bell-Shaped Curves | Absorbance enzyme activity | - Solubility assessment (nephelometry)- Secondary target panels- Cytotoxicity counterscreens (CellTox Green) | - Solubilizing agents (DMSO)- Chelating agents (EDTA)- Antioxidants (DTT) |
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Research Reagent Solutions for Dose-Response Troubleshooting
| Reagent Category | Specific Examples | Function in Troubleshooting | Application Context |
|---|---|---|---|
| Cellular Viability Indicators | CellTiter-Glo, MTT, Resazurin | Quantifies metabolic activity to distinguish specific activity from general toxicity [70] | Counterscreens for steep curves; cellular fitness assessment |
| Membrane Integrity Reporters | LDH assay, CellTox Green, propidium iodide | Identifies cytotoxic compounds through plasma membrane damage detection [70] | Exclusion of promiscuous toxic compounds in bell-shaped curves |
| Apoptosis Markers | Caspase-Glo 3/7, annexin V, TUNEL | Detects programmed cell death mechanisms that may confound target-specific effects [72] [70] | Secondary assessment of steep curve compounds |
| Oxidative Stress Indicators | 8OHG staining, DCFDA, MitoSOX | Measures reactive oxygen species generation contributing to nonspecific effects [72] | Interpretation of shallow curves with multiple mechanisms |
| DNA Damage Reporters | γH2AX staining, Comet assay | Identifies genotoxic compounds that may produce aberrant curve shapes [72] | Counterscreen for steep and bell-shaped curves |
| Biophysical Binding Tools | SPR chips, ITC cells, MST capillaries | Provides direct binding confirmation independent of functional readouts [70] | Orthogonal validation for shallow curves |
| Compound Solubility Enhancers | Detergents (Tween-20), BSA, cyclodextrins | Reduces aggregation-mediated artifactual inhibition [70] | Resolution of steep and bell-shaped curves |
Advanced Data Integration and Visualization Approaches
Multi-Parameter Toxicity Profiling
The Tox5-score methodology represents an advanced framework for integrating dose-response parameters from multiple endpoints and experimental conditions into a unified toxicity assessment metric [72]. This approach moves beyond single-endpoint GI₅₀ determinations to incorporate complementary readouts that control for potential assay interference from tested agents. The scoring system integrates data from five core toxicity assays measuring cell viability (CellTiter-Glo), cell number (DAPI), DNA damage (γH2AX), oxidative stress (8OHG), and apoptosis (Caspase-Glo 3/7) across multiple time points and concentration ranges [72]. This multidimensional data integration enables researchers to distinguish between specific bioactivity and general toxicity contributing to problematic curve shapes, particularly steep and bell-shaped profiles that may indicate deleterious cellular effects.
Figure 2: Multi-Endpoint Toxicity Scoring Workflow
FAIR Data Principles in HTS Analysis
Implementing Findability, Accessibility, Interoperability, and Reuse (FAIR) principles in HTS data management represents a critical advancement in dose-response analysis [72]. Automated data FAIRification workflows, such as those implemented in the ToxFAIRy Python module, facilitate the conversion of HTS data into standardized formats like NeXus, which integrates all data and metadata into a single file and multidimensional matrix structure [72]. This approach directly addresses challenges in curve interpretation by ensuring comprehensive metadata capture—including concentration, treatment time, material properties, cell line specifications, and replicate information—all of which are essential for contextualizing aberrant curve shapes. The application of these computational frameworks enables more robust curve shape analysis through consistent data processing pipelines that minimize manual handling errors and enhance reproducibility in reaction discovery research.
Systematic interpretation of dose-response curve profiles represents a critical competency in high-throughput screening for reaction discovery research. The framework presented in this guide enables researchers to distinguish between artifacts and genuine bioactivity through integrated experimental strategies combining counter assays, orthogonal approaches, and cellular fitness assessments. By implementing these structured troubleshooting methodologies and leveraging advanced data integration approaches like the Tox5-score, research teams can significantly enhance the efficiency of hit triage campaigns and prioritize compounds with the greatest potential for successful development. The continued adoption of FAIR data principles and standardized processing workflows will further strengthen the analytical rigor applied to dose-response curve interpretation across the drug discovery continuum.
From Hits to Leads: Validation Strategies and Comparative Analysis
In the field of high-throughput screening (HTS) for reaction discovery research, identifying active compounds (hits) from a primary screen is merely the first step. The most challenging and critical phase that follows is the hit confirmation cascade, a rigorous triaging process designed to separate true, specific bioactive compounds from false positives and assay artifacts. Within this cascade, the use of experimental replicates and the integrity of biological samples stand as non-negotiable principles to ensure data reproducibility and the identification of high-quality leads for further optimization [70] [73]. This guide outlines the essential experimental strategies and methodologies for establishing a robust hit confirmation workflow.
Core Principles of the Hit Confirmation Cascade
The hit confirmation cascade is a multi-stage experimental process designed to prioritize specific bioactive compounds by systematically eliminating artifacts and false positives. A primary HTS campaign typically tests compounds at a single concentration, generating an initial list of active compounds, or "primary hits." [70] [74] The core challenge is that this initial list is often populated with compounds that interfere with the assay technology itself rather than specifically modulating the biological target. [70]
The foundational principle of the subsequent cascade is to progressively apply more stringent and diverse experimental tests to confirm the bioactivity, specificity, and cellular relevance of these primary hits. This process is universally recognized as essential for scoring the most active and specific compounds. [70] Key pillars of this strategy include:
- Confirmation and Dose-Response: The first step involves re-testing the primary hits, typically in replicates, to confirm the activity observed in the initial screen. This is followed by generating dose-response curves to quantify potency (e.g., IC50/EC50) and efficacy. The shape of these curves can provide early warnings of issues such as toxicity, poor solubility, or compound aggregation. [70] [75] [74]
- Counter-Screening: These assays are designed specifically to identify and eliminate compounds that generate assay interference or technology-specific artifacts. This is critical for filtering out compounds that exhibit autofluorescence, signal quenching, singlet oxygen quenching, or non-specific protein reactivity. [70] [74]
- Orthogonal Screening: This involves confirming the biological activity using an assay with a fundamentally different readout technology. The purpose is to ensure the observed effect is genuine to the biology and not an artifact of the primary detection method. [70]
- Cellular Fitness Screening: This tier of testing is vital for cell-based assays to exclude compounds that exert their effects through general cytotoxicity or by compromising fundamental cellular health, thereby identifying compounds that maintain global non-toxicity. [70]
Essential Experimental Protocols and Strategies
Hit Confirmation and Potency Assessment
Objective: To verify the reproducibility of primary hits and quantify their biological activity.
Detailed Methodology:
- Confirmatory Screening: Re-test the primary hit compounds in the same assay conditions used in the primary HTS campaign, but now performing the experiment in independent replicates (e.g., duplicates or triplicates). This confirms that the initial activity is reproducible and not a statistical outlier or a result of a transient artifact. [74]
- Dose-Response Screening: Prepare a dilution series of each confirmed hit compound across a broad concentration range (typically 8-12 points in a 3- or 4-fold serial dilution). Test these concentrations in the primary assay to generate a concentration-response profile. [75] [74]
- Data Analysis: Fit the dose-response data to a four- or five-parameter logistic (4PL/5PL) model to derive key parameters of potency and efficacy [75]. The standard 4PL equation is:
Y = Bottom + (Top - Bottom) / (1 + 10^((LogIC50 - X) * HillSlope))whereYis the response,Xis the log10(concentration),TopandBottomare the upper and lower asymptotes,HillSlopedescribes the steepness of the curve, andLogIC50is the log10 of the concentration that produces a response halfway betweenTopandBottom. [22]
The Non-Negotiable: Replicates The use of replicates in confirmatory screening is fundamental to assessing the reproducibility of the primary result. In quantitative HTS (qHTS), where concentration-response curves are generated simultaneously for thousands of compounds, parameter estimates like AC50 can be highly variable if the data are from a single run. Incorporating experimental replicates significantly improves the precision of these parameter estimates, directly impacting the reliability of potency rankings. [22] [73] A lack of dose-response curve reproducibility is a common reason for discarding a compound. [70]
Counter-Screens for Artifact Elimination
Objective: To identify and eliminate compounds that act through technology interference or non-specific mechanisms.
Detailed Methodology: Counter screens are designed to bypass the actual biological reaction or interaction and instead measure the compound's effect on the detection technology. [70] Key strategies include:
- Assay Technology Interference: For a primary screen using a fluorescent readout, a counter-screen would involve testing the hit compounds in a system that contains all the detection reagents but lacks the key biological component (e.g., the enzyme or receptor). A compound that still generates a signal is likely autofluorescent or is quenching the signal. Similarly, for reporter gene assays (e.g., luciferase), counterscreens can identify compounds that directly inhibit the reporter enzyme. [70] [74]
- Aggregation-Based Inhibition: To identify compounds that act by forming colloidal aggregates, the dose-response assay is repeated in the presence of a non-ionic detergent like 0.01% Triton X-100. A significant reduction in potency in the presence of detergent is a strong indicator of aggregate-based inhibition. [75]
- Redox Cycling and Chelation: Specific assays can be deployed to detect compounds that interfere through chemical reactivity, such as redox cycling or metal chelation, which can lead to non-specific oxidation or inactivation of the target. [70]
The Non-Negotiable: Specificity Profiling Relying solely on the primary assay readout is insufficient. Counter-screens are a non-negotiable step to classify and eliminate compounds with undesirable mechanisms, ensuring that only compounds with a high likelihood of specific target interaction progress. [70]
Orthogonal Assays for Biological Validation
Objective: To confirm the bioactivity of hits using an independent assay that measures the same biological outcome but with a different readout technology.
Detailed Methodology: Orthogonal assays analyze the same biological pathway or phenotype but use a complementary detection method. The choice of orthogonal assay depends on the nature of the primary screen [70]:
- If the primary screening used a fluorescence-based readout, the orthogonal assay could employ luminescence or absorbance-based readouts.
- For biochemical, target-based approaches, biophysical assays are powerful orthogonal methods to confirm direct binding. These include:
- Surface Plasmon Resonance (SPR)
- Isothermal Titration Calorimetry (ITC)
- Microscale Thermophoresis (MST)
- If the primary screen was a bulk-readout cell-based assay (e.g., a plate reader measuring a population average), an excellent orthogonal method is high-content imaging and analysis. This allows inspection of the compound's effects on a single-cell level, providing a more comprehensive picture of the cellular phenotype (e.g., morphology, texture, protein translocation). [70]
Cellular Fitness Assays
Objective: To exclude compounds that exhibit general cytotoxicity or harm to cells, ensuring the identification of modulators that maintain global cellular non-toxicity.
Detailed Methodology: Cellular fitness can be assessed using a variety of assays that report on the health of the treated cell population [70]:
- Cell Viability Assays: Measure metabolic activity (e.g., CellTiter-Glo, MTT assay) or ATP content.
- Cytotoxicity Assays: Measure membrane integrity by detecting the release of enzymes like lactate dehydrogenase (LDH) (e.g., CytoTox-Glo, CellTox Green).
- Apoptosis Assays: Measure the activation of caspases, key enzymes in the programmed cell death pathway.
- High-Content Analysis of Cellular Health: Utilize microscopy-based techniques with fluorescent dyes to evaluate:
- Nuclear Integrity: Staining with DAPI or Hoechst for condensation or fragmentation.
- Mitochondrial Health: Staining with MitoTracker or TMRM/TMRE for membrane potential.
- Membrane Integrity: Staining with dyes like TO-PRO-3 or YOYO-1.
The following table summarizes the key experimental tiers of the hit confirmation cascade and their roles in ensuring data quality:
Table 1: Core Components of the Hit Confirmation Cascade
| Confirmation Tier | Primary Objective | Key Methodologies | Outcome |
|---|---|---|---|
| Dose-Response & Replicates | Confirm reproducibility & quantify potency | Re-testing in replicates; 8-12 point concentration curves; 4PL/5PL curve fitting [75] [74] | Reliable IC50/EC50 and Hill slope values |
| Counter-Screens | Eliminate technology artifacts & non-specific mechanisms | Assay interference profiling; detergent-based assays for aggregators; redox/chelation tests [70] [75] | Filtered list of specific bioactive compounds |
| Orthogonal Assays | Validate biology with independent readouts | SPR, ITC, MST; luminescence/absorbance alternatives; high-content imaging [70] | Confidence in the biological relevance of the hit |
| Cellular Fitness | Exclude general cytotoxicity | Viability (CellTiter-Glo), cytotoxicity (LDH), apoptosis (caspase) assays; high-content health profiling [70] | Identification of non-toxic, bioactive molecules |
The Critical Role of Sample Freshness and Handling
The Non-Negotiable: Sample Integrity The reliability of all experimental data in the confirmation cascade is contingent upon the integrity of the biological samples and reagents used. The use of fresh, properly handled samples is not merely a best practice but a fundamental requirement. This is critically highlighted by failures in other screening domains, such as prenatal testing for Down syndrome using the urinary biomarker beta-core fragment.
A three-year prospective study investigating this biomarker found that sample storage and handling directly impacted assay performance and data reproducibility. When urine samples were frozen, stored, and then re-assayed, the Down syndrome samples showed a significant and predictable loss of immunoreactivity, with higher initial values suffering greater losses. Researchers hypothesized that the beta-core fragment molecules aggregated upon storage in the freezer, which interfered with the assay's detection antibodies. This aggregation was partially reversible with high-salt buffer treatment, recovering lost immunoreactivity. [76] This case underscores a universal principle: poor sample handling can introduce systematic biases and artifacts, leading to both false negatives and an irreproducible or misleading assessment of a compound's or biomarker's true activity. For any screening campaign, establishing and rigorously adhering to standardized protocols for sample preparation, storage, and usage is essential to prevent such avoidable errors.
Visualizing the Hit Confirmation Workflow
The following diagram illustrates the sequential, multi-tiered process of the hit confirmation cascade, showing how a large set of primary hits is progressively refined into a small number of high-quality leads.
Hit Confirmation Cascade Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
A successful hit confirmation campaign relies on a suite of reliable reagents and assay kits. The following table details essential tools for implementing the cascade.
Table 2: Essential Research Reagent Solutions for Hit Confirmation
| Reagent / Assay Kit | Function in Hit Confirmation |
|---|---|
| Cell Viability Assays(e.g., CellTiter-Glo, MTT) | Measures metabolic activity or ATP content as a primary readout for cellular health and to exclude cytotoxic compounds. [70] |
| Cytotoxicity Assays(e.g., LDH assay, CytoTox-Glo, CellTox Green) | Measures membrane integrity and cell death, providing a complementary view to viability assays. [70] |
| Apoptosis Assays(e.g., Caspase Glo) | Detects activation of caspase enzymes to identify compounds that induce programmed cell death. [70] |
| High-Content Fluorescent Dyes(e.g., DAPI/Hoechst, MitoTracker, TMRM/TMRE) | Used in high-content imaging to assess nuclear integrity, mitochondrial mass, and membrane potential, respectively, for detailed cellular fitness profiling. [70] |
| Membrane Integrity Dyes(e.g., TO-PRO-3, YOYO-1) | Fluorescent dyes that only stain cells with compromised plasma membranes, indicating dead or dying cells. [70] |
| Non-Ionic Detergents(e.g., Triton X-100) | Used in counter-screens to identify colloidal aggregate-forming compounds; a loss of potency in the presence of detergent indicates aggregation. [75] |
| Biophysical Analysis Kits(For SPR, ITC, MST) | Reagents and consumables for configuring orthogonal, label-free assays to confirm direct binding of hits to the purified target. [70] |
The hit confirmation cascade is a disciplined and multi-faceted process that is fundamental to the success of any high-throughput screening campaign in reaction discovery research. It is a strategic funnel that systematically trades a large volume of initial data for a smaller set of high-confidence, high-quality leads. The consistent use of experimental replicates is crucial for establishing reproducibility and reliable parameter estimation, while the integrity of biological samples is a foundational prerequisite for generating trustworthy data. By rigorously implementing a workflow that integrates dose-response confirmation, targeted counter-screens, orthogonal biological validation, and cellular fitness testing, researchers can effectively mitigate the risks of artifact-driven dead ends. This ensures that resources are invested in optimizing truly promising chemical starting points, thereby accelerating the journey toward a viable lead candidate.
Employing Counter-Screens to Eliminate Assay Technology Interference
In the pursuit of novel chemical matter through high-throughput screening (HTS) for reaction discovery and drug development, a significant impediment to progress is the prevalence of false-positive signals. These artifacts can stem from various sources, but a pernicious and common category is assay technology interference, where compounds directly interfere with the detection method rather than engaging the intended target [77]. Within a broader thesis on HTS principles, the rigorous identification and elimination of such interference is not merely a cleanup step but a foundational practice for ensuring the fidelity of screening data and the efficient allocation of resources [78]. This guide details the strategic employment of counter-screens (or artefact assays) as an essential experimental methodology to purge these technological artifacts from hit lists.
The Principle and Design of Counter-Screens
A counter-screen is a parallel assay designed to be identical to the primary HTS assay in all components except for the biologically active target (e.g., the enzyme, receptor, or pathway being studied) [77] [78]. Its sole purpose is to identify compounds that generate a signal due to the assay technology itself. For instance, in a bead-based AlphaScreen assay, a compound acting as a biotin mimetic could produce a signal by bridging the donor and acceptor beads, independent of the target protein [77]. If a compound is active in the primary screen but also shows activity in the matched target-less counter-screen, it is classified as a Compound Interfering with an Assay Technology (CIAT) and is typically deprioritized [77].
This experimental strategy is a cornerstone of high-quality hit triaging [78]. It moves beyond purely computational filters by providing direct empirical evidence of interference, thereby protecting valuable resources from being wasted on following up false leads [77].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and reagents critical for establishing and running effective counter-screen campaigns.
| Research Reagent / Material | Function in Counter-Screening |
|---|---|
| Counter-Screening Plate (Assay-Ready) | A microplate identical to the primary screen plate, but pre-dispensed with all assay components (buffers, substrates, co-factors, detection reagents) excluding the target protein. This ensures perfect technological parity [77]. |
| Detection Kit (e.g., AlphaScreen, FRET) | The same signal-generation kit (beads, fluorescently labeled antibodies, etc.) used in the primary assay. Consistency is vital for isolating technology-specific interference [77]. |
| Vehicle Control (e.g., DMSO) | The compound solvent used in the primary screen. Serves as the negative control for the counter-screen to establish baseline signal. |
| Known Technology Interferer (Control Compound) | A compound historically validated to cause interference in the specific assay technology (e.g., a known fluorescent quencher for FRET). Acts as a positive control to validate the counter-screen's ability to detect interference. |
| Automated Liquid Handling System | Ensures precise and reproducible dispensing of compounds from the primary screening library into the counter-screen plates, minimizing operational variability. |
| High-Sensitivity Plate Reader | Instrumentation capable of detecting the assay's readout (luminescence, fluorescence, TR-FRET) with the same parameters as the primary screen. |
Methodology: Establishing and Implementing a Counter-Screen Protocol
A robust counter-screening protocol is integral to the HTS triage process [77] [78]. The following steps outline a detailed methodology:
- Data Collection & Compound Selection: Following a primary HTS campaign, collect results for all compounds. The population for counter-screening typically includes all primary hits exceeding a predefined activity threshold (e.g., >50% inhibition or activation) [77].
- Counter-Screen Assay Configuration: For each unique primary assay technology (e.g., AlphaScreen, TR-FRET), prepare an artefact assay plate. This involves using the exact same master mix protocol as the primary assay but omitting the target protein. The vacant target binding site or catalytic center is replaced with an equivalent volume of assay buffer.
- Experimental Execution: Using an acoustic or pintool dispenser, transfer the selected compounds from the primary assay plate to the corresponding counter-screen plate at the same tested concentration. Include control wells (vehicle and known interferer) on each plate.
- Incubation & Readout: Follow the identical incubation times, temperatures, and detection steps as the primary assay. Read the plates on the same reader using the same settings.
- Data Analysis & Hit Triage: Calculate percentage activity or signal modulation for each compound in the counter-screen. Compounds showing significant activity in the counter-screen (e.g., >30% signal modulation) are flagged as CIATs. The remaining active compounds from the primary screen that are inactive in the counter-screen are considered higher-quality, technology-interference-free hits for confirmation and dose-response studies [78].
Quantitative Performance of Machine Learning Models vs. Traditional Methods
The data derived from historical counter-screen campaigns can be used to build predictive computational models. The table below summarizes the performance of a Random Forest Classification (RFC) model trained on counter-screen data, compared to other common methods, as reported in a key study [77].
Table 1: Performance Comparison of CIAT Identification Methods Across HTS Technologies
| Assay Technology | Method | ROC AUC | Key Finding / Comparison |
|---|---|---|---|
| AlphaScreen | RFC (on counter-screen data) | 0.70 | The model provides a complementary and wider set of predicted CIATs compared to other methods [77]. |
| FRET | RFC (on counter-screen data) | 0.62 | Outperforms a structure-independent statistical method (BSF) when applied to novel compounds [77]. |
| TR-FRET | RFC (on counter-screen data) | 0.57 | Demonstrates the feasibility of learning interference patterns from artefact assay data [77]. |
| AlphaScreen | PAINS Substructure Filters | Very Low Accuracy (~9%) | Filters had low accuracy; performance was slightly better for AlphaScreen than other technologies, consistent with their origin [77]. |
| FRET/TR-FRET | PAINS Substructure Filters | Very Low Accuracy (~1.5%) | Highlights the limited applicability domain of PAINS filters when applied outside their original assay context [77]. |
| General | Binomial Survivor Function (BSF) | Not Applicable (Statistical Score) | A structure-independent method that cannot predict interference for novel, untested compounds [77]. |
ROC AUC: Area Under the Receiver Operating Characteristic Curve. A value of 0.5 indicates random performance, while 1.0 indicates perfect prediction.
Experimental Protocol for Building a Predictive CIAT Model from Counter-Screen Data
The following protocol is adapted from the machine-learning approach used to generate the data in Table 1 [77]:
- Dataset Curation: From an HTS database, compile results for compounds tested in primary assays for a specific technology (e.g., AlphaScreen). Extract matching results from the associated downstream artefact (counter-screen) assays for those same compounds.
- Compound Labeling: Label each compound as a CIAT (active in the artefact assay) or an NCIAT (non-interfering, inactive in the artefact assay). This forms the ground-truth dataset.
- Descriptor Calculation: Encode the chemical structure of each compound using 2D molecular descriptors (e.g., molecular weight, logP, topological indices, fingerprint bits).
- Model Training: Partition the data into training and test sets. Train a Random Forest classifier (or another suitable algorithm) using the structural descriptors as features and the CIAT/NCIAT label as the target variable.
- Validation & Application: Validate the model's performance on the held-out test set using metrics like ROC AUC. The trained model can then predict the interference potential of new compounds before they are even screened, acting as a pre-filter.
Visualizing the Workflow and Interference Mechanisms
The logical workflow for integrating counter-screens into an HTS triage process and the common mechanisms of assay interference are summarized in the following diagrams.
Diagram 1: Integrated hit triage workflow using a counter-screen.
Diagram 2: Categories of assay technology interference mechanisms.
In high-throughput screening (HTS) for reaction discovery research, orthogonal assays serve as a critical strategy for confirming that observed compound activity stems from genuine biological effects rather than assay-specific interference. Orthogonal assays are defined as methods that use fundamentally different physical or detection principles to measure the same biological attribute or activity [79]. This approach provides independent verification of initial screening results, dramatically increasing confidence in hit identification and characterization.
The essential value of orthogonal assays lies in their ability to eliminate false positives that frequently plague HTS campaigns. In conventional screening, compound interference can arise from various sources including compound aggregation, chemical reactivity, fluorescence interference, and enzyme inhibition unrelated to the targeted biology [80]. These interference mechanisms can produce reproducible, concentration-dependent activity that mimics genuine target engagement, making them particularly challenging to identify without secondary confirmation using different detection methodologies. By employing assays with distinct detection mechanisms, researchers can effectively discriminate between true biological activity and assay-specific artifacts, ensuring that only compounds with authentic mechanisms of action progress through the discovery pipeline.
The Critical Need for Orthogonal Assays in HTS
Modern HTS technologies rely heavily on sensitive light-based detection methods, such as fluorescence or luminescence, which are susceptible to various types of interference that can generate false positives [80]. The most problematic interference types share a key characteristic with genuine activity: they are reproducible and concentration-dependent. Common interference mechanisms include:
- Compound Aggregation: Compounds forming colloidal aggregates can non-specifically inhibit enzymes, with characteristics including steep Hill slopes, sensitivity to enzyme concentration, and reversibility by detergent [80].
- Compound Fluorescence: Fluorescent compounds can interfere with fluorescence-based detection, particularly in assays using blue-shifted spectral ranges where up to 50% of apparent actives may result from fluorescence interference [80].
- Reporter Enzyme Inhibition: Direct inhibition of reporter enzymes like firefly luciferase can account for as high as 60% of actives in some cell-based assays [80].
- Redox Reactivity: Compounds that undergo redox cycling can generate hydrogen peroxide, leading to time-dependent enzyme inactivation [80].
Regulatory and Scientific Rationale
From a regulatory perspective, agencies including the FDA, MHRA, and EMA have indicated in guidance documents that orthogonal methods should be used to strengthen underlying analytical data [81]. This regulatory emphasis reflects the scientific consensus that orthogonal approaches substantially enhance decision-making confidence throughout the drug discovery process. For complex therapeutics like cell and gene therapies, orthogonal methods are particularly recommended to fully characterize potency through multiple mechanisms of action [82].
Scientifically, orthogonal confirmation is essential for building robust structure-activity relationships (SAR) because it ensures that measured activity reflects true biological engagement rather than assay-specific artifacts. This is especially critical when advancing chemical matter through hit-to-lead optimization, where resource allocation decisions depend heavily on accurate activity assessments [83].
Implementing Orthogonal Assay Strategies: Methodologies and Protocols
Fundamental Principles of Orthogonality
Two analytical methods are considered orthogonal when they employ different physical principles to measure the same property of the same sample [79]. True orthogonality aims to minimize method-specific biases and potential interferences by approaching the measurement from fundamentally different directions. This differs from complementary measurements, which may target different attributes but reinforce each other to support the same decision [79].
In practical terms, orthogonality in biological assays can be achieved through various approaches:
- Different detection principles (e.g., mass spectrometry vs. fluorescence)
- Different experimental systems (e.g., biochemical vs. cell-based assays)
- Different measurement parameters (e.g., binding vs. functional activity)
- Different sample processing methods (e.g., labeled vs. label-free detection)
Case Study: Orthogonal Assays for WIP1 Phosphatase Inhibitor Discovery
A comprehensive example of orthogonal assay implementation comes from research on WIP1 phosphatase, an attractive cancer therapeutic target. Researchers developed two orthogonal biochemical activity assays utilizing phosphopeptides from native WIP1 substrates [84].
Mass Spectrometry-Based Assay Protocol
The first assay employed RapidFire mass spectrometry to directly quantify the enzymatically dephosphorylated peptide reaction product:
- Format: 384-well plate
- Substrate: Native phosphopeptide substrates (VEPPLpSQETFS)
- Reaction Conditions: 10-30 ng WIP1, 20 mM HEPES pH 7.5, 100 mM NaCl, 0.5 mM MnCl2, 0.01% Tween-20, 1 mM DTT
- Incubation: 30-60 minutes at room temperature
- Quenching: Formic acid (final concentration 0.5-1%)
- Internal Standard: 1 μM 13C-labeled product peptide for quantification
- Detection: RapidFire MS with MS/MS detection monitoring specific product ions
- Key Parameters: Limit of quantification (LOQ) = 28.3 nM, Z'-factor = 0.74, signal-to-background = 80 [84]
Fluorescence-Based Assay Protocol
The orthogonal assay utilized a red-shifted fluorescence detection method:
- Format: 1,536-well plate
- Detection Principle: Rhodamine-labeled phosphate binding protein (Rh-PBP) fluorescence change upon inorganic phosphate (Pi) binding
- Reaction Conditions: Similar to MS assay but optimized for real-time measurement
- Measurement: Real-time monitoring of Pi release using red-shifted fluorescence (excitation/emission ~575-620 nm)
- Advantages: Reduced interference from compound fluorescence, suitable for HTS [84]
The orthogonality between these assays stems from their fundamentally different detection principles—MS directly measures the dephosphorylated peptide product, while fluorescence detects the released inorganic phosphate. This approach validated the application of miniaturized physiologically relevant WIP1 activity assays to discover small-molecule modulators from HTS [84].
Experimental Workflow for Orthogonal Assay Development
The following diagram illustrates a generalized workflow for implementing orthogonal assays in hit confirmation:
Generalized Orthogonal Assay Workflow
Orthogonal Assay Applications Across Discovery Research
Cell-Based and Binding Assays
Cell-based assays provide particularly valuable orthogonal approaches because they enable assessment of compound activity in physiologically relevant environments that maintain critical aspects of protein behavior, including membrane localization, proper folding, post-translational modifications, and interactions with cofactors or endogenous ligands [85]. Unlike biochemical assays using purified proteins, cell-based systems can detect binding events conditional on physiological context, providing insight into target activity under near-physiological conditions.
Innovative platforms like oocyte-based binding assays (e.g., Vipergen's cellular Binder Trap Enrichment/cBTE) enable DNA-encoded library screening directly in live cells, preserving membrane context and protein folding for structurally complex targets that are difficult to purify or assay using classical methods [85]. These approaches are particularly valuable for targets like GPCRs, ion channels, and intracellular protein-protein interactions where native cellular environment is crucial for proper function.
Potency Assay Development for Cell Therapies
For advanced therapeutics like CAR-T and TCR-T cell therapies, orthogonal methods are recommended to fully characterize potency through multiple mechanisms of action [82]. A comprehensive potency strategy for these complex therapies typically includes:
- Genetic level assessment: Measuring delivery and integration of gene of interest using ddPCR or qPCR
- Protein expression: Quantifying transgene expression using flow cytometry
- Functional activity: Measuring cytokine release (e.g., IFNγ) using ELISA, ELLA, or MSD
- Cytotoxic activity: Assessing target cell killing using luminescence or flow cytometry-based assays [82]
This multi-faceted approach ensures that critical quality attributes are measured through independent methods, providing a comprehensive understanding of product quality and consistency.
Research Reagent Solutions for Orthogonal Assays
Table 1: Essential Research Reagents for Orthogonal Assay Development
| Reagent Category | Specific Examples | Function in Orthogonal Assays |
|---|---|---|
| Detection Systems | Rhodamine-labeled phosphate binding protein (Rh-PBP) [84] | Enables real-time fluorescence detection of inorganic phosphate release in phosphatase assays |
| Mass Spec Standards | 13C-labeled peptide internal standards [84] | Provides accurate quantification in MS-based assays through internal calibration |
| Cell-Based Systems | Xenopus laevis oocytes [85] | Preserves native membrane environment for studying membrane protein targets |
| Assay Technologies | AlphaScreen, Surface Plasmon Resonance (SPR) [84] [81] | Provides alternative detection principles for binding and functional assays |
| Cytokine Detection | ELISA, ELLA, MSD platforms [82] | Measures functional cytokine release in cell-based potency assays |
| Genetic Tools | ddPCR, qPCR reagents [82] | Quantifies transgene delivery and integration in gene-modified therapies |
Comparison of Orthogonal Assay Modalities
Table 2: Orthogonal Assay Platforms and Their Characteristics
| Assay Platform | Detection Principle | Typical Applications | Advantages | Limitations |
|---|---|---|---|---|
| RapidFire Mass Spectrometry [84] | Mass-to-charge ratio measurement | Enzyme activity, metabolite quantification | Direct product measurement, minimal interference | Lower throughput, specialized equipment |
| Fluorescence (Red-Shifted) [84] | Fluorescence emission change | Enzyme activity, binding assays | Reduces compound autofluorescence, HTS compatible | Potential quenching, interference |
| Surface Plasmon Resonance (SPR) [84] [83] | Refractive index changes | Binding kinetics, affinity measurements | Label-free, provides kinetic parameters | Surface immobilization effects |
| Cell-Based Binding Assays [85] | Ligand binding in live cells | Membrane protein targets, complex interfaces | Physiological relevance, native environment | Throughput limitations, viability concerns |
| Thermal Shift Assays [83] | Protein thermal stability | Target engagement, binding confirmation | Label-free, works with impure proteins | Indirect binding measurement |
| Cellular Cytotoxicity [82] | Luminescence or fluorescence | Cell-killing capacity, functional potency | Functional relevance, mechanistic insight | Variable biological response |
Implementation Framework and Best Practices
Designing an Orthogonal Assay Strategy
Successful implementation of orthogonal assays requires careful planning and consideration of the specific research context:
- Pre-planning: Identify potential interference mechanisms in primary assays and select orthogonal methods that circumvent these limitations [80].
- Physiological Relevance: Prioritize assays that utilize native substrates and physiologically relevant conditions when possible [84].
- Throughput Matching: Ensure orthogonal assays have appropriate throughput for the confirmation stage, which may involve smaller compound sets than primary HTS.
- Data Integration: Implement systems that enable efficient comparison and analysis of results across different assay platforms [81].
Data Management and Analysis Considerations
The combination of multiple assay technologies presents data management challenges that require specialized solutions:
- Platform Integration: Utilize data management systems that can handle diverse data types from different instrumentation [81].
- Cross-Assay Analytics: Implement analytical tools that enable combined analysis of results from primary and orthogonal assays for structure-activity relationship (SAR) analysis [81].
- Visualization Tools: Employ interactive visualization platforms that facilitate comparison of results across different assay modalities and enable informed decision-making about compound progression [81].
Orthogonal assays represent an indispensable component of modern high-throughput screening for reaction discovery research. By employing fundamentally different detection principles to measure the same biological activity, orthogonal approaches provide critical validation of initial screening results, effectively discriminating between genuine biological activity and assay-specific artifacts. The implementation of well-designed orthogonal assay strategies enhances decision-making confidence, reduces costly late-stage attrition, and ultimately accelerates the discovery of novel therapeutic agents. As drug discovery increasingly focuses on complex biological targets and sophisticated therapeutic modalities, the role of orthogonal assays in providing robust, physiologically relevant validation will only continue to grow in importance.
In high-throughput screening (HTS), a primary challenge is distinguishing true bioactive compounds from false positives that arise from assay interference or non-specific mechanisms. Counterscreens are indispensable experimental strategies designed to identify and eliminate these artifacts by assessing compound specificity and cellular fitness. This technical guide details the implementation of counter, orthogonal, and cellular fitness screens within HTS cascades, providing a structured framework to prioritize high-quality hits for reaction discovery and drug development research. By employing these methodologies, researchers can effectively triage primary hit sets toward specific and bioactive molecules, thereby enhancing the efficiency and success of early drug discovery campaigns [70] [86].
The initial phase of a high-throughput screening (HTS) or high-content screening (HCS) campaign generates a list of primary active compounds (hits). The most critical subsequent task is to differentiate true, specific modulators from false-positive hits. False positives frequently result from compound interference with the assay technology, readout, or format, such as compound fluorescence, aggregation, luciferase inhibition, redox reactivity, or general cytotoxicity [86]. A carefully designed counterscreening strategy is essential to mitigate these risks, ensuring that a hit discovery program advances only the most promising, on-target compounds [70].
Counterscreens are follow-up experiments that do not necessarily need to be high-throughput themselves, as they are applied to a markedly reduced number of selected primary hits. Their primary purpose is to assess hit specificity and eliminate artifacts, thereby classifying and removing compounds that interfere with the readout technology or exhibit non-specific activity [70]. This process is fundamental to the broader thesis that robust HTS principles require a cascade of computational and experimental approaches to select for activity, specificity, and cellular compatibility.
Classifying Counterscreening Strategies
Experimental efforts to triage HTS/HCS hits should integrate three complementary types of screens: counter, orthogonal, and cellular fitness screens. These can be conducted in parallel or consecutively to develop a detailed picture of a compound's effects [70]. The following table summarizes the objectives and examples for each strategy.
Table 1: Classification of Key Counterscreening Strategies
| Screen Type | Primary Objective | Common Examples |
|---|---|---|
| Counter Screen | Identify and eliminate compounds causing assay technology interference or non-specific activity. | Luciferase inhibition assay, HTRF signal interference assay, cytotoxicity assay, redox assay, aggregation test [70] [86]. |
| Orthogonal Screen | Confirm the bioactivity of primary hits using a different readout technology or assay condition. | Replacing fluorescence with luminescence or absorbance; using SPR, ITC, or MST in target-based approaches; high-content imaging vs. bulk-readout [70]. |
| Cellular Fitness Screen | Exclude compounds exhibiting general toxicity or harm to cells to classify bioactive yet non-toxic molecules. | Cell viability (CellTiter-Glo, MTT), cytotoxicity (LDH assay, CytoTox-Glo), apoptosis (caspase assay), high-content analysis of organelles [70]. |
Counter Screens
Counter screens are designed to identify compounds that interfere with the detection technology used in the primary HTS. For example, in a luminescent assay, a technology counter screen (e.g., a luciferase false-positive screen) detects compounds that directly inhibit the luciferase enzyme itself. Similarly, in an HTRF (Homogeneous Time-Resolved Fluorescence) assay, analyzing raw data can help flag compounds that interfere with the FRET signal [86].
A specificity counter screen is used to filter out compounds that produce a signal through undesirable, off-target properties. In cellular assays, a common cause of false-positive hits is general cytotoxicity. Designing a cytotoxicity assay specifically for detecting and eliminating compounds that modulate the readout through cellular death is therefore essential. This confirms whether the observed activity is specific to the target pathway or a consequence of cell death [86].
Orthogonal and Cellular Fitness Assays
Orthogonal assays analyze the same biological outcome as the primary screen but use an independent readout technology or assay format. This provides greater confidence that the observed activity is genuine. For instance, a fluorescence-based primary screen can be validated with a luminescence- or absorbance-based assay. In target-based approaches, biophysical methods like Surface Plasmon Resonance (SPR) or Isothermal Titration Calorimetry (ITC) can characterize compound binding and affinity directly [70].
Cellular fitness screens ensure that hit compounds do not exhibit general toxicity. These assays can use bulk-readout methods like CellTiter-Glo for viability or high-content, image-based techniques. High-content analysis can evaluate cellular health using nuclear staining and counting, mitochondrial stains (e.g., MitoTracker), or membrane integrity dyes (e.g., TO-PRO-3). The "cell painting" assay provides a particularly comprehensive morphological profile that can predict compound-mediated cellular toxicity [70].
Experimental Design and Workflow
Integrating counterscreens effectively requires strategic planning regarding their placement within the overall HTS cascade. The optimal stage for deploying a counterscreen depends on the specific project needs and the nature of the primary screen.
Screening Cascade Models
The placement of the counterscreen within the workflow can be adapted for efficiency and early filtering.
Table 2: HTS Screening Cascades Illustrating Counterscreen Placement
| Cascade Type | Workflow Sequence | Typical Use Case |
|---|---|---|
| Basic Cascade | Primary Screen → Hit Potency (Dose-Response) → Counterscreen (at hit confirmation/triplicate stage) → Hit Validation [86]. | Protein-protein interaction HTS where a technology counterscreen is sufficient. |
| Adapted Cascade | Primary Screen → Counterscreen → Hit Confirmation/Triplicate → Hit Potency → Hit Validation [86]. | Cell-based HTS prone to cytotoxicity, or assays where a co-factor accounts for many hits, requiring early artifact identification. |
Key Experimental Protocols
This section outlines general methodologies for key experiments in the counterscreening workflow.
3.2.1 Primary Hit Potency Assessment Following the primary screen, hit compounds are tested in a broad concentration range to generate dose-response curves, from which half-maximal inhibitory concentration (ICâ‚…â‚€) values are calculated.
- Methodology: Serially dilute hit compounds in the assay buffer or cell culture medium. Test each dilution in the primary assay format. Plot the response (e.g., % inhibition) against the logarithm of the compound concentration. Fit a curve to the data points to determine the ICâ‚…â‚€.
- Data Triaging: Compounds that do not generate reproducible dose-response curves are discarded. Curves with steep, shallow, or bell-shaped profiles may indicate toxicity, poor solubility, or aggregation, and these hits are typically removed [70].
3.2.2 Technology Counter Screen: Luciferase Inhibition Assay This is critical for primary screens using luciferase-based readouts.
- Methodology: In a cell-free system, incubate test compounds with the luciferase enzyme and its substrate (e.g., D-luciferin). Measure the resulting luminescence signal over time. A significant decrease in luminescence compared to a vehicle control indicates direct inhibition of the luciferase enzyme [86].
- Data Triaging: Compounds showing potent luciferase inhibition are flagged as assay-specific artifacts and are excluded from further progression.
3.2.3 Specificity Counter Screen: Cytotoxicity Assay This identifies compounds whose activity in a cellular primary screen is due to general cell death.
- Methodology: Use the same cell line as the primary screen but measure a viability endpoint. Common assays include:
- CellTiter-Glo Assay: Measures cellular ATP levels, indicating metabolically active cells.
- LDH (Lactate Dehydrogenase) Assay: Measures the release of LDH from cells with compromised membranes, indicating cytotoxicity.
- High-Content Analysis: Use dyes like CellTox Green (cytoplasmic staining) or YOYO-1 (nucleic acid staining) in combination with live-cell markers to quantify the proportion of dead versus healthy cells on a single-cell level [70].
- Data Triaging: Compounds that significantly reduce viability or increase cytotoxicity at or near their active concentration in the primary assay are considered non-specific and are typically removed. A 10-fold potency window between the primary activity and cytotoxicity is often considered a promising starting point [86].
Visualization of Workflows and Relationships
The following diagrams, generated with Graphviz using the specified color palette, illustrate the logical relationships and experimental workflows described in this guide.
HTS Hit Triage Strategy
This diagram outlines the overarching strategy for triaging HTS hits using computational and experimental approaches.
Counterscreen Deployment Cascade
This diagram compares the two main strategies for integrating counterscreens into the HTS workflow.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of the described counterscreening strategies relies on a set of key reagents and tools. The following table details essential materials and their functions.
Table 3: Key Research Reagent Solutions for Counterscreens
| Reagent / Assay | Function in Counterscreening |
|---|---|
| Luciferase Enzyme & Substrate | Core components for technology counterscreens in luminescence-based assays; identifies compounds that inhibit the reporter enzyme [86]. |
| CellTiter-Glo / MTT Reagents | Measure cellular ATP (CellTiter-Glo) or metabolic activity (MTT) as indicators of cell viability and health in cellular fitness screens [70]. |
| LDH Assay Kit | Quantifies lactate dehydrogenase release from cells, serving as a biomarker for cytotoxicity and plasma membrane damage [70]. |
| MitoTracker / TMRM/TMRE Dyes | Fluorescent dyes that stain active mitochondria; used in high-content cellular fitness screens to assess mitochondrial health and function [70]. |
| CellTox Green / YOYO-1 Dyes | DNA-binding dyes that are impermeant to live cells; used to label dead cells specifically in high-content cytotoxicity assays [70]. |
| Surface Plasmon Resonance (SPR) Chip | A biosensor surface used in biophysical orthogonal assays to directly measure binding kinetics and affinity between a target and a hit compound [70]. |
| BSA (Bovine Serum Albumin) / Detergents | Buffer additives used to reduce unspecific compound binding (BSA) or counteract compound aggregation (detergents) during counter assays [70]. |
High-Throughput Screening (HTS) is an automated, robust process that enables the rapid testing of large chemical, genetic, or biological libraries to identify effectors of specific biological mechanisms [50]. The ultimate success of HTS in drug discovery depends on assays that are reproducible in miniaturized formats, have low false-positive rates, and can identify compounds with genuine therapeutic potential [50]. Within this framework, advanced validation techniques—encompassing biophysical methods and cellular fitness assays—serve a critical role. They move beyond simple activity readouts to provide deep characterization of binding events and cellular health, ensuring that only the highest quality hits progress through the discovery pipeline. Biophysical methods quantify the precise physical interactions between biomolecules, offering data on binding affinity, kinetics, and thermodynamics. Concurrently, cellular fitness assays assess the broader physiological impact of compounds on cells, identifying and eliminating those that cause stress or toxicity unrelated to the intended target [78]. This integrated approach is fundamental for triaging false positives and prioritizing credible lead compounds.
Core Biophysical Methods for Binding Characterization
Biophysical techniques are cornerstone technologies for confirming direct target engagement and characterizing the nature of biomolecular interactions. They provide robust, label-free data that is indispensable for hit confirmation and lead optimization.
Surface Plasmon Resonance (SPR)
2.1.1 Principle and Workflow Surface Plasmon Resonance (SPR) is a label-free technique that quantitatively analyzes binding interactions in real-time by measuring changes in the refractive index on a sensor surface [87] [88]. In a typical SPR setup, one binding partner (the ligand) is immobilized onto a thin gold film sensor chip. The other partner (the analyte) is flowed over this surface in solution. When binding occurs, it increases the mass on the sensor surface, altering the refractive index and causing a shift in the resonance angle or wavelength of reflected light [87] [89]. This shift is measured as a response signal (Response Units, RU) over time, generating a sensorgram that details the entire binding event: association as the analyte binds, equilibrium, and dissociation as it is washed away [89]. Localized SPR (LSPR) is a variation that uses metal nanoparticles instead of a continuous gold film, offering benefits such as reduced instrument cost, portability, and robustness against buffer mismatch and temperature drift [87].
2.1.2 Data Output and Applications
SPR directly provides the association rate constant (kon), the dissociation rate constant (koff), and the equilibrium dissociation constant (KD), which is calculated as koff/kon [87] [89]. This kinetic profile is highly valuable for drug discovery, as it reveals not just the strength of an interaction (KD), but also the speed of binding and unbinding. This information can predict the functional and pharmacokinetic properties of a drug candidate. SPR is widely used for hit confirmation, detailed kinetic characterization of lead compounds, and epitope mapping [90]. Its high sensitivity and ability to measure a wide range of on-rates, off-rates, and affinities have established it as a gold standard in the field [87].
Diagram 1: SPR experimental workflow.
Isothermal Titration Calorimetry (ITC)
2.2.1 Principle and Workflow Isothermal Titration Calorimetry (ITC) is a powerful, label-free technique that directly measures the heat released or absorbed during a biomolecular binding event [87] [89]. The instrument consists of a reference cell (filled with solvent or buffer) and a sample cell (containing one binding partner, e.g., a protein). The second binding partner (the ligand) is loaded into a syringe and titrated into the sample cell in a series of small injections. The instrument measures the power (microjoules per second) required to maintain a constant temperature difference (typically zero) between the two cells [87]. Each injection produces a heat burst (exothermic or endothermic) that is plotted against time. Integrating these peaks produces a binding isotherm, which is fit to a model to extract thermodynamic parameters [89].
2.2.2 Data Output and Applications
ITC is unique in its ability to provide a complete thermodynamic profile of an interaction in a single experiment [89]. The primary data outputs are the equilibrium binding constant (KA, from which KD is derived), the stoichiometry of binding (n), the change in enthalpy (ΔH), and the change in entropy (ΔS). The change in Gibbs free energy (ΔG) is calculated from these values [89]. This thermodynamic signature helps researchers understand the driving forces behind binding—whether it is enthalpically driven (e.g., through hydrogen bonds) or entropically driven (e.g., through hydrophobic interactions). This information is crucial for guiding medicinal chemistry efforts to optimize lead compounds [90].
Microscale Thermophoresis (MST)
2.3.1 Principle and Workflow Microscale Thermophoresis (MST) measures the directed motion of fluorescent molecules in response to a microscopic temperature gradient [87]. A key property is that a molecule's movement (thermophoresis) depends on its size, charge, and hydration shell. When this molecule binds to a partner, one or more of these properties change, resulting in a measurable change in its thermophoretic movement [87]. In a typical experiment, a target molecule is fluorescently labeled (either intrinsically or via a dye) and mixed with a series of concentrations of the unlabeled binding partner. Each mixture is loaded into a capillary, and a focused infrared laser creates a microscopic temperature gradient. The instrument monitors the fluorescence as the molecules move through this gradient.
2.3.2 Data Output and Applications
The change in fluorescence is used to calculate the fraction of bound target, allowing for the determination of the equilibrium dissociation constant (KD) [87]. A significant advantage of MST is its ability to work in complex biological fluids like cell lysates, serum, or even in the presence of detergents, making it suitable for studying interactions under near-native conditions [87]. It requires very small sample volumes and can handle a wide size range of interactants, from ions to mega-Dalton complexes [87].
Table 1: Comparative Overview of Key Biophysical Techniques
| Parameter | SPR | ITC | MST |
|---|---|---|---|
| What it Measures | Binding kinetics & affinity | Thermodynamics & affinity | Affinity |
| Key Outputs | kon, koff, KD |
KD, n, ΔH, ΔS, ΔG |
KD |
| Immobilization | Required | Not required | Not required |
| Label-Free | Yes | Yes | No (requires fluorescence) |
| Sample Consumption | Low [87] | High [87] [88] | Very Low [87] |
| Throughput | High [87] | Low (0.25-2 h/assay) [87] | Medium to High |
| Affinity Range | pM - mM [89] | nM - μM [89] | nM - mM [87] |
Table 2: Summary of Technique Advantages and Limitations
| Technique | Primary Advantages | Key Limitations |
|---|---|---|
| SPR | Label-free, real-time kinetics, high sensitivity and throughput, wide affinity range [87] [89] | Requires immobilization, high cost, steep learning curve, fluidic maintenance [87] |
| ITC | Label-free, provides full thermodynamic profile, no immobilization [87] [89] | Large sample quantity, low throughput, insensitive to very weak/strong binding [87] [88] |
| MST | Very small sample volume, works in complex mixtures, wide analyte size range [87] | Requires fluorescence (labeling or intrinsic), no kinetic data, potential for confounding parameters [87] |
The Role of Cellular Fitness Assays in HTS
While biophysical methods confirm direct binding, cellular fitness assays evaluate the overall physiological state of cells following treatment with test compounds. This is a critical counter-screen to eliminate false positives caused by general cellular toxicity or stress.
Principles and Significance
Cellular fitness assays are designed to assess the health and viability of cells in response to perturbations, such as exposure to small-molecule libraries during HTS [78]. A common challenge in HTS is the presence of hit compounds that generate assay interference or non-specific cytotoxicity, leading to false-positive results [78]. For example, a compound might inhibit a readout (e.g., luminescence) not by modulating the intended target, but by generally killing cells or inhibiting transcription/translation. Fitness assays help identify these artifacts. An integrated platform for cellular fitness might assess parameters such as cell proliferation, membrane integrity, and the induction of stress response proteins like Hsp10 and Hsp70 in the same experimental well [91]. Monitoring these markers provides a multiplexed readout of overall cellular fitness, allowing researchers to determine optimal experimental conditions and filter out promiscuous or toxic compounds early in the screening cascade [91] [78].
Implementation in Screening Cascades
These assays are strategically positioned as secondary or orthogonal screens. A practical example is the three-step HTS phenotypic cascade developed to identify necroptosis inhibitors [92]. After a primary screen identified compounds that inhibited TNF-α-induced cell death, a critical secondary step tested whether these same compounds interfered with apoptosis. This successfully filtered out compounds that were generally cytotoxic rather than specifically inhibiting the necroptosis pathway, ensuring the selection of high-quality, mechanism-specific hits [92]. This process of "hit triaging" using cellular fitness endpoints is essential for prioritizing compounds with a higher likelihood of success in later-stage development [78].
Diagram 2: HTS hit triaging workflow.
Integrated Experimental Design and Protocols
Success in HTS relies on strategically combining biophysical and cell-based validation into a coherent workflow. The following section outlines key protocols and practical considerations for implementation.
Reagent Quality Control for Biophysical Assays
The integrity of the protein reagent is arguably the most critical factor in any biophysical or biochemical assay, as issues can compromise an entire screening campaign [90]. A comprehensive quality control (QC) profile should be established before initiating large-scale screening.
Table 3: Essential Protein Quality Control Checks [90]
| QC Group | Methods | Information Gained |
|---|---|---|
| Identity | LC-MS, Amino Acid Analysis | Confirms correct sequence and molecular mass. |
| Purity | SDS-PAGE, Analytical SEC, DLS | Assesses homogeneity and monodispersity; detects aggregates. |
| Concentration | UV Spectrometry, Bradford Assay | Provides accurate concentration for experiment stoichiometry. |
| Functionality | ITC, SPR, Functional Assay | Verifies binding competence and catalytic activity with a known tool compound. |
| Stability | DSF, DSC | Determines melting temperature (Tm) and evaluates thermal stability. |
Detailed Protocol: Isothermal Titration Calorimetry (ITC)
1. Sample Preparation:
- Protein/Buffer Matching: The protein and ligand must be in identical buffer conditions to avoid heat effects from buffer mismatch. This is often achieved by dialysis.
- Degassing: Both protein and ligand solutions must be degassed prior to the experiment to prevent bubble formation in the cell during titration.
- Concentration: The cell typically contains the larger binding partner at a concentration that will yield a measurable
c-value (c = n*[Mcell]/KD), ideally between 10 and 100. The syringe contains the ligand at a concentration 10-20 times higher than that in the cell [89].
2. Experimental Setup:
- Load the degassed protein solution into the sample cell and the ligand solution into the syringe.
- Set the experimental parameters: temperature, reference power, stirring speed, number of injections, injection volume, and duration between injections.
3. Data Collection and Analysis:
- The instrument automatically performs the series of injections, measuring the heat change with each one.
- The raw data (μcal/sec vs. time) is integrated to produce a plot of kcal/mol of injectant vs. molar ratio.
- This binding isotherm is fit to an appropriate model (e.g., a "one set of sites" model) to obtain the
KA (1/KD),n, ΔH, and ΔS[89].
Detailed Protocol: A Cellular Fitness Assay (High-Content)
1. Cell Seeding and Treatment:
- Seed cells (e.g., HeLa cells) in a 96- or 384-well microplate optimized for imaging and allow them to adhere.
- Transfert cells with a reporter (e.g., EGFP plasmid) using the transfection reagent of choice (e.g., FuGENE HD was identified as optimal in one study for minimal side effects [91]).
- Treat cells with test compounds from the HTS hit list over a range of concentrations and for a defined exposure time.
2. Staining and Multiplexed Readout:
- Fix and stain cells with fluorescent dyes or antibodies to mark key fitness parameters:
- Nuclei (e.g., DAPI or Hoechst) for cell count and proliferation.
- Cytoskeleton (e.g., Phalloidin) for morphological assessment.
- Stress Markers (e.g., antibodies against Hsp70 or Hsp10) [91].
- Alternatively, use live-cell dyes to assess membrane integrity or mitochondrial health.
3. Image Acquisition and Analysis:
- Use an automated microscope to acquire high-resolution images from multiple sites per well.
- Employ high-content analysis software to extract quantitative data from the images, for example:
- Total cell count per well (proliferation).
- Percentage of EGFP-positive cells (transfection efficiency).
- Mean intensity of Hsp70 staining per cell (stress response) [91].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagent Solutions for Advanced Validation Assays
| Reagent / Solution | Function / Application | Example Notes |
|---|---|---|
| SPR Sensor Chips | Provides a surface for ligand immobilization. | Available with different chemistries (e.g., CM5 for covalent coupling, NTA for His-tagged capture) [88]. |
| ITC-grade Buffers | Ensures no heat of dilution artifacts. | Requires meticulous buffer matching; often prepared from a common dialysate stock [89]. |
| Fluorescent Dyes (MST) | Enables detection via thermophoresis. | Can be covalently linked to the target protein; labeling efficiency and specificity are critical [87]. |
| Cell Viability/Cytotoxicity Kits | Measures cellular fitness. | Kits based on ATP content (e.g., CellTiter-Glo) or membrane integrity (e.g., LDH release) are common [92]. |
| Antibodies for Stress Markers | Detects unfolded protein response. | Antibodies against heat shock proteins (Hsp70, Hsp10) are used in high-content fitness assays [91]. |
| Transfection Reagents | Introduces DNA/RNA for cell-based assays. | FuGENE HD was identified in one screen as optimal with minimal impact on cellular health [91]. |
The integration of biophysical methods and cellular fitness assays creates a powerful validation framework for high-throughput screening campaigns. SPR, ITC, and MST provide complementary, high-fidelity data on the biophysical nature of binding events, from kinetics to thermodynamics. Meanwhile, cellular fitness assays act as an essential filter, ensuring that the observed activity is driven by specific target modulation rather than general cellular toxicity. Employing these techniques in a strategic, sequential manner—from primary HTS to hit confirmation and characterization—dramatically improves the quality of the resulting hit list. This rigorous, multi-faceted approach de-risks the early drug discovery pipeline, ensuring that only the most promising and reliable chemical starting points are selected for the costly and time-intensive process of lead optimization.
Conclusion
High-Throughput Screening stands as a powerful, integrated discipline that merges biology, chemistry, and data science to accelerate discovery. The journey from a conceptual screen to a validated lead compound requires meticulous attention to foundational principles, robust assay design, sophisticated statistical analysis, and a multi-faceted validation strategy. As the field evolves, future directions are poised to tackle increasingly 'difficult-to-drug' targets through advanced modalities like targeted protein degradation. Furthermore, the ongoing trends toward further miniaturization, the integration of AI and machine learning for data analysis, and the adoption of more physiologically relevant 3D cell models promise to enhance the sensitivity, predictive power, and success rate of HTS campaigns, solidifying its critical role in biomedical research and therapeutic development.
References
- 1. High-Throughput Screening - Drug Discovery [https://www.technologynetworks.com/drug-discovery/articles/high-throughput-screening-principles-applications-and-advancements-405121]
- 2. High Throughput Screening (HTS) [https://www.sygnaturediscovery.com/drug-discovery/bioscience/screening/medium-high-throughput-screening-mts-hts-2/]
- 3. The essential roles of chemistry in high-throughput screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4465542/]
- 4. A Robotic Platform for Quantitative High-Throughput Screening [https://pmc.ncbi.nlm.nih.gov/articles/PMC2651822/]
- 5. Miniaturization technologies in HTS: how fast, how small, ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644698012033]
- 6. High-Throughput Screening Assay Miniaturization [https://focus.gbo.com/blog/hts/the-power-of-small-high-throughput-screening-assay-miniaturization]
- 7. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOopftv_-5DXSYCnbHi7dK25qDNWjyhrWsf1OQQPKnuV5rGIC1VkS]
- 8. Why Does Sensitivity Matter for High-Throughput Screening? [https://bellbrooklabs.com/why-does-sensitivity-matter-for-high-throughput-screening/?srsltid=AfmBOooPyxENIfT-Xp4dujrBjRQpSePAuUnGrOJ9nZ--3b99CQOYp0-w]
- 9. High-Throughput Screening Meets AI and 3D Models [https://www.technologynetworks.com/drug-discovery/articles/how-high-throughput-screening-is-transforming-modern-drug-discovery-405922]
- 10. Highly sensitive fluorescence detection technology ... [https://pubmed.ncbi.nlm.nih.gov/12867149/]
- 11. Sensitivity and breadth of detection of high-throughput ... [https://www.nature.com/articles/s41541-020-0207-4]
- 12. A Quantitative High-Throughput Screening Data Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9540341/]
- 13. Novel trends in high-throughput screening [https://www.sciencedirect.com/science/article/abs/pii/S1471489209001283]
- 14. High-throughput screening [https://en.wikipedia.org/wiki/High-throughput_screening]
- 15. The History of Microplates [https://www.news-medical.net/life-sciences/The-History-of-Microplates.aspx]
- 16. Origin and evolution of high throughput screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1978279/]
- 17. Evolution of Ultra-High-Throughput Screening [https://www.labmanager.com/evolution-of-ultra-high-throughput-screening-17974]
- 18. Application and prospects of high-throughput screening for in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9244953/]
- 19. Ultra High Throughput Screening of Natural Product ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4521994/]
- 20. High-Throughput Screening Platforms in the Discovery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7926814/]
- 21. to Lead (H2L) Hit in Drug Discovery Process [https://www.azolifesciences.com/article/Hit-to-Lead-(H2L)-Process-in-Drug-Discovery.aspx]
- 22. Quantitative high-throughput screening data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4375054/]
- 23. High Throughput Screening - an overview [https://www.sciencedirect.com/topics/chemistry/high-throughput-screening]
- 24. High Throughput Screening - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/high-throughput-screening]
- 25. A protocol for high-throughput screening ... [https://www.sciencedirect.com/science/article/pii/S2666166723003726]
- 26. Compound Management for Quantitative High-Throughput ... [https://www.sciencedirect.com/science/article/pii/S1535553507003541]
- 27. Protocol for high-throughput compound screening using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7985391/]
- 28. Phenotypic and target-based HTS in drug discovery [https://lifechemicals.com/blog/computational-chemistry/476-phenotypic-and-target-based-hts-in-drug-discovery]
- 29. Mechanism of Action and Target Identification - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7479624/]
- 30. Phenotypic Drug Discovery: Recent successes, lessons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9708951/]
- 31. Phenotypic Screening - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/phenotypic-screening]
- 32. Target Identification vs. Phenotypic Screening in Drug ... [https://pharmafeatures.com/strategic-dichotomy-target-identification-vs-phenotypic-screening-in-drug-discovery/]
- 33. The Application of Phenotypic High-Throughput Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2836266/]
- 34. Phenotypic Versus Target-Based Screening for Drug ... [https://www.technologynetworks.com/drug-discovery/articles/phenotypic-versus-target-based-screening-for-drug-discovery-300037]
- 35. Phenotype and target-based chemical biology investigations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8291603/]
- 36. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOooxOhqOzqDUSzUaPfk6_-ftyBz_JaTX-oNSDgcDFg-St4u_mvUR]
- 37. High throughput fluorescence imaging approaches for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4863443/]
- 38. High content screening strategies for large-scale ... [https://www.sciencedirect.com/science/article/abs/pii/S0166354223002425]
- 39. An Overview of High | The Scientist Throughput Screening [https://www.the-scientist.com/an-overview-of-high-throughput-screening-71561]
- 40. - Liquid in Handling - High Throughput Screening [https://www.microlit.us/the-crucial-role-of-liquid-handling-instruments-in-high-throughput-screening/]
- 41. How Microplate Readers Are Transforming Modern ... [https://flowster.app/microplate-readers-transforming-modern-laboratory-research/]
- 42. The microplate: utility in practice [https://www.bmglabtech.com/en/the-microplate-utility-in-practice/]
- 43. The Microplate Market Past, Present and Future [https://www.ddw-online.com/the-microplate-market-past-present-and-future-1127-200904/]
- 44. Overview of liquid instrumentation for handling - high ... throughput [https://pubmed.ncbi.nlm.nih.gov/23839961/]
- 45. Microplates for Drug Discovery [https://www.corning.com/worldwide/en/products/life-sciences/products/microplates.html]
- 46. High Throughput Screening Assays for Drug Discovery [https://bellbrooklabs.com/high-throughput-screening-assays-drug-discovery/?srsltid=AfmBOorjPl8qRIIdIH9ZOq89lgWfl2YSqGBmlfATZPDq1kECwE0HbQy3]
- 47. The evolution of chemical collections and drug-like diversity [https://www.ddw-online.com/the-evolution-of-chemical-collections-and-drug-like-diversity-36277-202509/]
- 48. Discovery of aldolase A inhibitors via high-throughput ... [https://pubmed.ncbi.nlm.nih.gov/40651537/]
- 49. Identification of effective antiviral 3CLpro inhibitors [https://www.sciencedirect.com/science/article/pii/S0166354225000452]
- 50. Cell-based high-throughput screens for the discovery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3388188/]
- 51. A high-throughput drug screening strategy against ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7832824/]
- 52. High-throughput screening and genome-wide analyses of 44 ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1009732]
- 53. High-throughput screening and evaluation of repurposed ... [https://www.nature.com/articles/s41392-021-00763-5]
- 54. Advances in high-throughput drug screening based on ... [https://www.sciencedirect.com/science/article/pii/S2090123225006897]
- 55. Recent advances in high-throughput screening methods ... [https://www.sciencedirect.com/science/article/abs/pii/S1367593125000031]
- 56. A comparison of assay performance measures in screening assays ... [https://pubmed.ncbi.nlm.nih.gov/16490779/]
- 57. Cradle – The Art of Assays , Part 1: Insights From Our Lab Into... [https://www.cradle.bio/blog/the-art-of-assays-part-1]
- 58. Expediting hit-to-lead progression in drug discovery ... [https://www.nature.com/articles/s41467-025-66324-4]
- 59. Systematic error detection in experimental high-throughput ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3034671/]
- 60. Designing High-Throughput Experiments Using Microplate ... [https://www.labx.com/resources/designing-high-throughput-experiments-using-microplate-technology/5576]
- 61. A Simple Technique for Reducing Edge Effect in Cell ... [https://www.sciencedirect.com/science/article/pii/S2472630322002242]
- 62. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 63. Hit selection [https://en.wikipedia.org/wiki/Hit_selection]
- 64. Assay performance and the Z'-factor in HTS [https://www.drugtargetreview.com/article/108865/assay-performance-and-the-z-factor-in-hts/]
- 65. The use of strictly standardized mean difference for hit ... [https://pubmed.ncbi.nlm.nih.gov/17435171/]
- 66. The Z prime value (Z´) [https://www.bmglabtech.com/en/blog/the-z-prime-value/]
- 67. High-Throughput Screening Normalized To Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3867592/]
- 68. Selecting Approaches for Hit Identification and Increasing ... [https://www.sciencedirect.com/science/article/pii/S2472555222066734]
- 69. Robust Analysis of High Throughput Screening (HTS) Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3727440/]
- 70. Brief Guide: Experimental Strategies for High-Quality Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8293735/]
- 71. Grouping concentration response curves by features of ... [https://www.sciencedirect.com/science/article/pii/S2472555221000198]
- 72. High-throughput screening data generation, scoring and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020062/]
- 73. Assessing Reproducibility of High-throughput Experiments ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9039958/]
- 74. High Throughput Screening (HTS) Services [https://www.evotec.com/solutions/drug-discovery-preclinical-development/discovery/hit-identification-services/high-throughput-screening-hts-services]
- 75. High Throughput Screening [https://www.chemdiv.com/high-throughput-screening-hts/]
- 76. Urinary screening tests for fetal Down syndrome: I. Fresh beta ... [https://pubmed.ncbi.nlm.nih.gov/10327140/]
- 77. Identification of Compounds That Interfere with High†... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6856845/]
- 78. Experimental Strategies for High-Quality Hit Selection from ... [https://www.sciencedirect.com/science/article/pii/S2472555222067296]
- 79. Orthogonal and complementary measurements of ... [https://www.sciencedirect.com/science/article/pii/S016836592200863X]
- 80. Apparent Activity in High-Throughput Screening: Origins ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2878863/]
- 81. Therapeutics Discovery with Orthogonal Assay Data [https://revvitysignals.com/article/blog/improving-therapeutics-discovery-orthogonal-assay-data]
- 82. Accelerating Innovative Cell Therapy Development ... [https://elevate.bio/elevated-insights/accelerating-innovative-cell-therapy-development-through-phase-appropriate-potency-control/]
- 83. Target Engagement Assays in Early Drug Discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207595/]
- 84. Physiologically relevant orthogonal assays for the discovery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6873202/]
- 85. Unlocking the Potential of Cell-Based Assays in Modern ... [https://www.vipergen.com/unlocking-the-potential-of-cell-based-assays-in-modern-scientific-research/]
- 86. The Importance of Counter Screens in HTS [https://www.sygnaturediscovery.com/news-and-events/blog/the-importance-of-counter-screens-in-hts/]
- 87. SPR, ITC, MST & BLI: What's the optimal interaction ... [https://nicoyalife.com/blog/spr-vs-itc-vs-mst-vs-bli/]
- 88. High-throughput investigation of macromolecular ... [https://link.springer.com/article/10.1007/s12551-025-01359-x]
- 89. Isothermal titration calorimetry and surface plasmon ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202324000707]
- 90. Biophysical methods in early drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8963580/]
- 91. A high content assay to assess cellular fitness - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/23957721/]
- 92. Phenotypic high-throughput screening platform identifies ... [https://www.nature.com/articles/s41420-020-0240-0]