Partial Validation for Modified Analytical Methods: A Lifecycle Guide for Pharma Professionals
This article provides a comprehensive guide to partial validation for modified analytical methods in pharmaceutical development.
Partial Validation for Modified Analytical Methods: A Lifecycle Guide for Pharma Professionals
Abstract
This article provides a comprehensive guide to partial validation for modified analytical methods in pharmaceutical development. Tailored for researchers and scientists, it clarifies when partial validation is required, outlines a risk-based methodology for its execution, and presents strategies for troubleshooting and optimization. By synthesizing regulatory expectations and practical applications, this resource empowers professionals to ensure data integrity and maintain regulatory compliance throughout a method's lifecycle, from foundational concepts to comparative analysis with other validation types.
Understanding Partial Validation: Definitions, Scope, and Regulatory Context
In the lifecycle of an analytical method, modifications are inevitable. Partial validation is the documented process of establishing that a previously fully validated bioanalytical method remains reliable after a modification, without necessitating a complete re-validation [1] [2]. It is a targeted, risk-based assessment that confirms the method's continued suitability for its intended use following specific, often minor, changes.
This guide provides a structured comparison of partial, full, and cross-validation to help researchers and scientists select the appropriate validation pathway.
What is Partial Validation?
Partial validation is defined as the demonstration of assay reliability following a modification of an existing bioanalytical method that has previously been fully validated [1]. It is not a less rigorous process, but a more focused one. The extent of testing is determined by the nature and potential impact of the change, and can range from a single intra-assay precision and accuracy experiment to a nearly full validation [1] [2].
The core principle is a risk-based approach, where the parameters evaluated are selected based on the potential impacts of the modifications on method performance [1].
When is Partial Validation Required?
Common scenarios requiring partial validation include [3] [1] [2]:
- Method transfer between laboratories or analysts.
- Changes in instrumentation or software platforms.
- Changes to sample processing procedures (e.g., a change in extraction volume).
- Modification of the analytical methodology within the same technology (e.g., a minor change in mobile phase pH or composition).
- Extension of the analytical range.
- Changes in the species within the same matrix (e.g., rat plasma to mouse plasma).
- Changes in the matrix within the same species (e.g., human plasma to human urine), though a change in matrix type may sometimes be considered a new method requiring full validation [1].
The table below summarizes the core objectives, typical triggers, and scope of the three main types of method validation.
| Feature | Full Validation | Partial Validation | Cross-Validation |
|---|---|---|---|
| Objective | Establish performance characteristics for a new method, proving it is suitable for its intended use [3] [2]. | Confirm reliability after a modification to a fully validated method [1] [2]. | Compare two bioanalytical methods to ensure data comparability [3] [2]. |
| Typical Triggers | - Newly developed method [2]- Adding a metabolite to an assay [2]- New drug entity [3] | - Method transfer [3]- Minor changes in equipment, SOPs, or analysts [3] [1]- Change in sample processing [1] | - Data from >1 lab or method within the same study [2]- Comparing original and revised methods [2]- Different analytical techniques used across studies [2] |
| Scope | Comprehensive assessment of all validation parameters (e.g., specificity, accuracy, precision, LLOQ, linearity, stability, robustness) [3]. | Targeted assessment based on risk. Evaluates only parameters potentially affected by the change (e.g., only precision and accuracy for an analyst change) [1]. | Direct comparison of methods using spiked matrix and/or subject samples to establish equivalence or concordance [3] [2]. |
Experimental Protocols and Data Requirements
The experimental design for each validation type varies significantly in breadth. The following table outlines the key parameters and data requirements based on regulatory guidance and industry best practices.
| Validation Parameter | Full Validation | Partial Validation | Cross-Validation |
|---|---|---|---|
| Accuracy & Precision | Required. Minimum of 5 determinations per 3 concentrations (LLOQ, Low, Mid, High) [2]. | Required for affected parameters. Scope depends on change (e.g., 2 sets over 2 days for chromatographic method transfer) [1]. | Required. Comparison of accuracy and precision profiles between the two methods. |
| Linearity & Range | Required. Minimum of 5 concentrations to establish calibration model [2]. | May be required if the quantitative range is modified. | Required to ensure overlapping ranges of quantitation. |
| Specificity/Selectivity | Required. Must demonstrate no interference from blank matrix, metabolites, etc. [2]. | Required if modification could impact interference (e.g., new matrix). | Required to show both methods can differentiate the analyte. |
| Stability | Comprehensive (freeze-thaw, short-term, long-term, post-preparative) [2]. | May be required if storage conditions or sample processing changes. | Not typically a focus, unless stability differences are suspected. |
| Robustness | Evaluated to show method resilience to deliberate variations [3]. | Often a key focus if equipment or reagents are changed. | Not typically assessed. |
| Key Experiment | Complete characterization of the method. | Targeted experiments based on risk assessment of the change. | Co-analysis of a set of samples by both methods. |
Detailed Protocol: Method Transfer as a Partial Validation
A common application of partial validation is the transfer of a chromatographic assay. The Global Bioanalytical Consortium provides specific recommendations for this scenario [1]:
- Objective: To demonstrate that a method performs similarly in a receiving laboratory compared to the originating laboratory.
- Experimental Design:
- A minimum of two sets of accuracy and precision data are generated over a 2-day period.
- Quality Control (QC) samples at the Lower Limit of Quantification (LLOQ) must be included.
- QC samples at the upper limit (ULOQ) are not required.
- Experiments like dilution or stability are generally not required unless the environmental conditions (e.g., temperature, humidity) are expected to be an issue.
- Acceptance Criteria: The results must meet pre-defined acceptance criteria for precision and accuracy, demonstrating the method is performing similarly in the new environment [1].
The Validation Lifecycle: A Decision Workflow
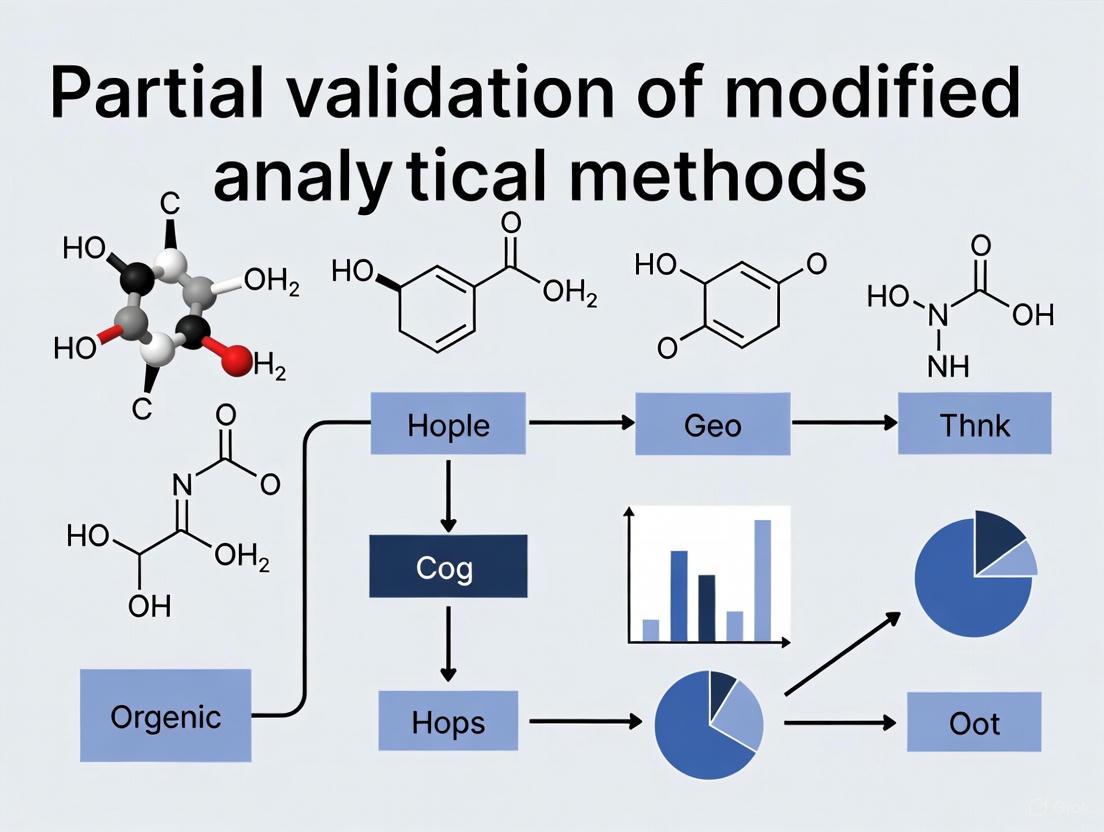
The following diagram illustrates the logical relationships between different validation activities and the triggers for selecting partial validation over other types.
Research Reagent Solutions for Method Validation
The following table details key materials and reagents essential for conducting robust method validation studies, particularly in chromatographic assays.
| Reagent/Material | Function in Validation | Critical Consideration |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for identifying the analyte and constructing calibration curves [2]. | Purity and stability are paramount; must be well-characterized and obtained from a certified source. |
| Control Blank Matrix | The biological fluid (e.g., plasma, urine) without the analyte, used to demonstrate specificity [2]. | Must be from the same species and type as the study samples. The absence of interfering components is critical. |
| Quality Control (QC) Samples | Spiked samples at low, mid, and high concentrations within the calibration curve, used to assess accuracy and precision [2]. | Should be prepared independently from calibration standards and used to monitor the performance of each analytical run. |
| Stable Isotope-Labeled Internal Standard | Added to all samples to correct for variability in sample preparation and instrument response, improving precision [1]. | Ideally used in chromatographic assays (e.g., LC-MS); must demonstrate no interference with the analyte. |
| Mobile Phase Components | The solvent system used to elute the analyte from the chromatographic column [4]. | Composition, pH, and buffer concentration are Critical Method Variables (CMVs) that can affect retention time, peak shape, and resolution [4]. |
| Chromatographic Column | The stationary phase where separation of the analyte from matrix components occurs. | Specifications (e.g., C18, dimensions, particle size) are key method parameters. Reproducibility between columns lots should be assessed for robustness. |
Selecting the correct validation pathway is critical for both regulatory compliance and scientific integrity. Full validation is the foundation for any new method. Partial validation is a flexible, risk-based tool for managing the inevitable evolution of a method post-validation, ensuring continued reliability while conserving resources. Cross-validation is the specific process for bridging data when multiple methods or laboratories are involved. Understanding these distinctions allows drug development professionals to build a efficient and compliant analytical lifecycle, ensuring that data quality is maintained from development through to routine application.
In the rigorous landscape of pharmaceutical development, the traditional approach to analytical method validation has been a comprehensive, one-time event conducted before a method's implementation. However, this static model is increasingly misaligned with the dynamic needs of modern drug development, where methods must evolve in response to new formulations, patient populations, and manufacturing processes. Partial validation represents a paradigm shift toward a more flexible, risk-based approach where specific method parameters are re-evaluated when method conditions change, rather than performing full revalidation. This strategy is embedded within a broader continuous improvement framework, enabling organizations to maintain methodological rigor while accelerating development timelines and reducing costs.
The concept of partial validation is particularly crucial within Model-Informed Drug Development (MIDD) approaches, where quantitative models are iteratively refined as new data emerges. These models, which include population pharmacokinetics (popPK), physiologically based pharmacokinetic (PBPK) modeling, and exposure-response modeling, rely on a foundation of analytically valid measurements that remain fit-for-purpose throughout the drug development lifecycle. As noted by regulatory scientists, MIDD approaches "allow an integration of information obtained from non-clinical studies and clinical trials in a drug development program" and enable more informed decision-making while reducing uncertainty [5]. Partial validation provides the mechanism through which the analytical methods supporting these models can adapt efficiently to expanding data sources and evolving clinical contexts.
Theoretical Framework: Partial Validation in Continuous Improvement Cycles
The Method Lifecycle and Validation Triggers
The method lifecycle extends far beyond initial validation, encompassing development, implementation, monitoring, and iterative improvement. Within this continuum, partial validation serves as a targeted mechanism for ensuring ongoing method reliability when specific, predefined changes occur. Unlike full validation, which verifies all performance parameters, partial validation focuses only on those parameters likely to be affected by a given modification, making it both resource-efficient and scientifically appropriate.
Key triggers for partial validation include:
- Transfer of methods between laboratories or sites
- Changes in methodology or instrumentation
- Updates to drug formulation or composition
- Expansion to new patient populations or matrices
- Evolution of regulatory requirements or standards
- Implementation of new software or algorithms for data analysis
The foundation for partial validation lies in risk-based decision making, where the scope of revalidation is determined by assessing the potential impact of changes on method performance. This approach aligns with the principles of Lean Sigma methodology, which has been successfully deployed across drug discovery value chains to deliver "incremental and transformational improvement in product quality, delivery time and cost" [6]. By applying these principles to analytical method management, organizations can eliminate wasteful comprehensive revalidation when targeted assessment would suffice.
Integration with Continuous Improvement Philosophies
Partial validation operates as a critical enabler of continuous improvement in analytical science, providing the mechanism through which methods can evolve without compromising quality. In the context of pharmaceutical R&D, continuous improvement programs focus on "increasing clinical proof-of-concept (PoC) success and the speed of candidate drug (CD) delivery" [6]. Analytical methods must keep pace with this accelerated timeline while maintaining reliability.
The integration occurs through:
- Iterative Method Enhancement: Systematic gathering of method performance data during routine use identifies opportunities for refinement, with partial validation confirming improvements maintain reliability.
- Knowledge Management: Documenting partial validation outcomes builds institutional understanding of method robustness and critical parameters.
- Reduced Method Lifecycle Costs: Targeted validation activities conserve resources compared to full revalidation, freeing capacity for innovation.
- Adaptive Compliance Strategies: Partial validation provides a structured approach to maintaining regulatory compliance while implementing method improvements.
This integrated approach is particularly valuable when deploying artificial intelligence and machine learning in drug discovery, where models require continuous refinement based on new data. As noted in industry assessments of AI in drug discovery, establishing "clear and measurable KPIs to track progress and evaluate the effectiveness of research efforts" is essential for continuous improvement [7]. Partial validation of the analytical methods that generate training data for these AI models ensures their ongoing reliability as the models evolve.
Comparative Analysis: Partial Validation vs. Traditional Approaches
Performance Metrics Comparison
The strategic implementation of partial validation offers significant advantages across multiple performance dimensions compared to traditional full validation approaches. These benefits extend beyond mere cost reduction to impact timelines, resource allocation, and methodological agility.
Table 1: Comparative Analysis of Validation Approaches in the Method Lifecycle
| Performance Metric | Traditional Full Validation | Partial Validation Approach | Comparative Advantage |
|---|---|---|---|
| Validation Timeline | 4-8 weeks (all parameters) | 1-3 weeks (targeted parameters) | 50-75% reduction in validation time |
| Resource Requirements | High (cross-functional team, extensive testing) | Moderate (focused team, selective testing) | 40-60% reduction in resource utilization |
| Method Agility | Low (resistant to change due to revalidation burden) | High (structured approach to method evolution) | Enables rapid method adaptation |
| Regulatory Flexibility | Limited (fixed validation package) | Adaptable (risk-based documentation) | Better alignment with QbD principles |
| Cost Implications | $50,000-100,000 per full validation | $15,000-30,000 per partial validation | 60-70% cost reduction per change |
| Knowledge Management | Static validation package | Growing understanding of critical parameters | Enhanced method robustness understanding |
Impact on Drug Development Timelines
The cumulative effect of partial validation implementation across the drug development lifecycle can substantially accelerate overall development programs. With the average drug development process taking 10-15 years [8], efficiency gains in analytical method management contribute to reducing this timeline.
In practice, a typical drug development program may require 15-25 significant method modifications throughout its lifecycle. Under a traditional validation approach, these changes would trigger full revalidation, consuming approximately 18-48 months of cumulative validation time. Through partial validation, this timeline can be reduced to 6-18 months, representing a potential saving of 1-2.5 years in overall development time. These efficiencies are particularly valuable in the clinical research phase, where approximately 25-30% of phase III studies ultimately receive regulatory approval [8], making speed and adaptability critical competitive advantages.
The application of partial validation principles extends beyond conventional small molecules to complex modalities like biologics and cell and gene therapies, where "the potential for future application of MIDD include understanding and quantitative evaluation of information related to biological activity/pharmacodynamics, cell expansion/persistence, transgene expression, immune response, safety, and efficacy" [5]. As these innovative therapies require increasingly sophisticated analytical methods, partial validation provides a pathway for method evolution without excessive regulatory burden.
Experimental Protocols for Partial Validation Studies
Protocol Design Principles
Designing scientifically sound partial validation studies requires careful consideration of the specific method changes being implemented and their potential impact on method performance. The foundational principle is risk-based scope determination, where the extent of validation is proportional to the significance of the method modification. This approach aligns with the experimental medicine approach discussed in neuroscience drug development, which employs an "iterative process of testing specific mechanistic hypotheses" [9].
Key design considerations include:
- Change Impact Assessment: Systematic evaluation of how method modifications might affect different validation parameters.
- Parameter Selection: Identification of specific validation parameters (accuracy, precision, specificity, etc.) that require re-evaluation based on the change.
- Acceptance Criteria Definition: Establishment of predefined criteria for each parameter based on method requirements and regulatory expectations.
- Statistical Power: Appropriate sample size determination to ensure sufficient power to detect clinically or analytically significant changes.
- Comparative Testing: Inclusion of original method conditions alongside modified conditions to facilitate direct comparison.
These design principles support the continuous improvement philosophy by creating a structured framework for method evolution. As described in evaluations of Lean Sigma in drug discovery, successful implementation requires "distinguishing 'desirable' and 'undesirable' variability because variability in research can be a source of innovation" [6]. Partial validation protocols must similarly distinguish between meaningful changes in method performance and acceptable variation.
Specific Experimental Protocols
Protocol for Instrumentation Platform Transfer
Objective: Validate method performance after transfer to a new instrument platform while maintaining original method parameters.
Experimental Design:
- Sample Preparation: Prepare three concentration levels (QC low, medium, high) covering the calibration range (n=6 each).
- Analysis Sequence: Analyze in random order across original and new instrumentation.
- Comparison Approach: Use statistical equivalence testing with pre-defined equivalence margins (±15% for accuracy, ≤15% RSD for precision).
- Data Analysis: Calculate between-instrument difference in accuracy and precision using appropriate statistical methods.
Acceptance Criteria: No statistically significant difference (p<0.05) in accuracy or precision between platforms; all QC samples within ±15% of nominal concentration.
Protocol for Sample Matrix Expansion
Objective: Validate method performance when extending an established method to a new patient population with potentially different matrix composition.
Experimental Design:
- Sample Preparation: Prepare QC samples in original and new matrices (n=6 each at three concentrations).
- Selectivity Assessment: Analyze individual matrix lots from at least 6 different sources.
- Matrix Effect Evaluation: Use post-column infusion to assess ionization suppression/enhancement.
- Stability Assessment: Evaluate stability in new matrix under relevant storage conditions.
Acceptance Criteria: Accuracy and precision within ±15% (±20% at LLOQ) of nominal values; no significant matrix effect; selectivity demonstrated across all individual matrix lots.
Case Studies: Partial Validation in Drug Development Applications
Case Study 1: Model-Informed Drug Development
The application of partial validation is particularly evident in Model-Informed Drug Development (MIDD), where models are continuously refined as new clinical data becomes available. In one documented case, MIDD approaches were used to support the approval of a new dosing regimen for paliperidone palmitate without additional clinical trials. The approach utilized "popPK modeling and simulation to support approval of a loading dose, dosing window, re-initiation strategy and dosage adjustment in patient subgroups" [5].
The analytical methods supporting the popPK model underwent partial validation when:
- The model was expanded to new patient subpopulations
- Additional metabolic pathways were incorporated
- The model was adapted to support a new dosing regimen
In each case, partial validation focused specifically on parameters affected by these changes, such as model precision at new concentration ranges or selectivity in the presence of new metabolites. This approach enabled continuous model refinement while maintaining regulatory confidence, ultimately supporting "regulatory decision-making and policy development" [5]. The success of this case highlights how partial validation of supporting analytical methods enables the application of MIDD approaches across the drug development lifecycle.
Case Study 2: Continuous Improvement in Oncology Drug Discovery
AstraZeneca's deployment of a continuous improvement program across its oncology drug discovery value chain provides another compelling case study. The program utilized Lean Sigma methodology to increase "clinical proof-of-concept (PoC) success and the speed of candidate drug (CD) delivery" [6]. Analytical method management was identified as a critical component of this initiative.
Key outcomes included:
- Reduced Method Qualification Time: Implementation of partial validation strategies reduced average method qualification time by 45% when methods were transferred between research sites.
- Enhanced Method Portability: Standardized partial validation protocols enabled more efficient method transfer between discovery and development teams.
- Accelerated Candidate Selection: Robust yet flexible analytical methods allowed for more rapid comparison of candidate compounds against critical quality attributes.
The program succeeded by focusing on "process, project and strategic" levels of the drug discovery value chain [6], with partial validation serving as a key enabler at the process level. This case demonstrates how partial validation integrates with broader continuous improvement initiatives to enhance R&D productivity.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing effective partial validation strategies requires carefully selected reagents, reference standards, and analytical materials. These tools ensure validation studies accurately assess method performance while maintaining efficiency and regulatory compliance.
Table 2: Essential Research Reagents and Solutions for Partial Validation Studies
| Reagent/Solution | Function in Partial Validation | Critical Quality Attributes | Application Examples |
|---|---|---|---|
| Authentic Reference Standards | Quantification and method calibration | Purity, stability, structural confirmation | Potency determination, method calibration |
| Stable Isotope-Labeled Internal Standards | Normalization of analytical variability | Isotopic purity, chemical stability | Mass spectrometry-based assays |
| Matrix Blank Solutions | Assessment of selectivity and specificity | Matrix composition, absence of interferents | Selectivity verification in new populations |
| Quality Control Materials | Monitoring method performance | Stability, homogeneity, commutability | Accuracy and precision assessment |
| System Suitability Solutions | Verification of instrument performance | Retention characteristics, peak shape | System performance monitoring |
| Extraction Solvents & Reagents | Sample preparation procedural consistency | Purity, composition, lot-to-lot consistency | Extraction efficiency studies |
The selection and qualification of these materials should be proportionate to their intended use in partial validation studies. For example, when expanding a method to a new matrix, particular attention should be paid to sourcing representative matrix materials from appropriate populations. This approach aligns with the growing emphasis on diversity in clinical research [8], ensuring analytical methods remain valid across diverse patient populations.
Visualization of Method Lifecycle and Partial Validation Workflow
The following diagram illustrates the continuous improvement cycle for analytical methods, highlighting decision points for partial validation within the method lifecycle.
Method Lifecycle and Validation Decision Workflow
This workflow emphasizes the risk-based decision making central to partial validation strategies. Changes trigger assessment of potential impact on method performance, with the validation response proportionate to the risk. This approach ensures efficient resource utilization while maintaining methodological integrity.
Statistical Approaches for Partial Validation Data Analysis
Method Comparison Techniques
Statistical analysis of partial validation data focuses on demonstrating equivalence between the original and modified method conditions. Appropriate statistical methods vary based on the validation parameter being assessed and the nature of the method change.
Table 3: Statistical Methods for Partial Validation Data Analysis
| Validation Parameter | Recommended Statistical Methods | Equivalence Criteria | Data Requirements |
|---|---|---|---|
| Accuracy | Equivalence testing (TOST), Bland-Altman analysis | ±15% of nominal value (±20% at LLOQ) | 3 concentrations, n≥5 replicates |
| Precision | F-test for variance comparison, ANOVA | RSD ≤15% (≤20% at LLOQ) | 3 concentrations, n≥6 replicates |
| Selectivity | Hypothesis testing for interference | No significant interference (p<0.05) | 6 individual matrix sources |
| Linearity | Weighted regression, lack-of-fit test | R² ≥0.99, residuals ≤15% | 5-8 concentration levels |
| Robustness | Experimental design (DoE), ANOVA | No significant effect (p<0.05) | Deliberate variations |
These statistical approaches enable objective assessment of whether method modifications have significantly impacted performance. The use of equivalence testing is particularly important, as it directly tests the hypothesis that method performance remains equivalent within predefined acceptance limits, rather than merely failing to find a difference as with traditional hypothesis testing.
Integration with Analytical Validation Frameworks
The statistical approaches for partial validation align with broader analytical validation frameworks being developed for novel measurement technologies. For example, in the validation of sensor-based digital health technologies (sDHTs), researchers have evaluated multiple statistical methods including "the Pearson correlation coefficient (PCC) between DM and RM, simple linear regression (SLR) between DM and RM, multiple linear regression (MLR) between DMs and combinations of RMs, and 2-factor, correlated-factor confirmatory factor analysis (CFA) models" [10].
These approaches can be adapted to partial validation of traditional analytical methods, particularly when dealing with:
- Complex method modifications affecting multiple parameters simultaneously
- Multivariate data requiring advanced modeling techniques
- Method harmonization across multiple sites or platforms
The findings from digital health validation research suggest that "CFA to assess the relationship between a novel DM and a COA RM" [10] may be applicable to analytical method validation when establishing equivalence between original and modified method conditions.
Partial validation represents a sophisticated, risk-based approach to analytical method management that aligns with continuous improvement philosophies in pharmaceutical development. By enabling targeted, efficient method evolution while maintaining regulatory compliance, partial validation strategies directly address the industry's need for greater efficiency and adaptability. When implemented within a structured framework with appropriate statistical support, partial validation reduces development costs and timelines while enhancing method understanding and robustness.
The integration of partial validation with emerging approaches like Model-Informed Drug Development and digital health technologies creates opportunities for further optimization of the method lifecycle. As drug development continues to evolve toward more personalized medicines and complex therapeutic modalities, the flexible, science-driven principles of partial validation will become increasingly essential for maintaining analytical excellence while supporting innovation.
In the pharmaceutical industry, analytical methods are developed and validated to ensure the identity, potency, purity, and performance of drug substances and products. The lifecycle of an analytical procedure naturally requires modifications over time due to factors such as changes in the synthesis of the drug substance, composition of the finished product, or the analytical procedure itself [11]. When such changes occur, revalidation is necessary to ensure the method remains suitable for its intended purpose. The extent of this revalidation—often termed partial validation—depends on the nature of the changes [11]. Global regulatory bodies, including the International Council for Harmonisation (ICH), the US Food and Drug Administration (FDA), and the United States Pharmacopeia (USP), provide the foundational guidelines that govern these modification processes. A thorough understanding of these drivers is essential for researchers, scientists, and drug development professionals to maintain regulatory compliance and ensure the continued reliability of analytical data throughout a product's lifecycle.
Comparative Analysis of ICH, FDA, and USP Guidelines
The regulatory frameworks provided by ICH, FDA, and USP, while aligned in their overall goal of ensuring data quality, exhibit differences in terminology, structure, and specific requirements. The following table provides a high-level comparison of these key regulatory bodies.
Table 1: Comparison of Key Regulatory Bodies for Analytical Methods
| Regulatory Body | Primary Role & Scope | Key Guidance Documents | Regulatory Standing |
|---|---|---|---|
| International Council for Harmonisation (ICH) | Develops international technical guidelines for the pharmaceutical industry to ensure safety, efficacy, and quality [12] [13]. | ICH Q2(R2) Validation of Analytical Procedures [12]; ICH Q14 Analytical Procedure Development [13]. | Provides harmonized standards; adopted by regulatory agencies (e.g., FDA, EMA). |
| US Food and Drug Administration (FDA) | US regulatory agency that enforces laws and issues binding regulations and non-binding guidance for drug approval and marketing [14]. | Adopts and enforces ICH guidelines (e.g., Q2(R2)) [12]; Issues FDA-specific guidance documents. | Has legal authority; requirements are mandatory for market approval in the US. |
| United States Pharmacopeia (USP) | Independent, scientific organization that sets public compendial standards for medicines and their ingredients [15] [16]. | General Chapters: <1220> Analytical Procedure Lifecycle [16], <1225> Validation of Compendial Procedures [11]. | Recognized in legislation (Food, Drug, and Cosmetic Act); standards are legally enforceable. |
Detailed Comparison of Validation Parameters and Terminology
A critical aspect for scientists is navigating the specific validation characteristics required by different guidelines. The following table compares the parameters as outlined by ICH, FDA, and USP, which is crucial for planning any method modification and subsequent partial validation.
Table 2: Comparison of Analytical Validation Parameters Across Guidelines
| Validation Characteristic | ICH Q2(R2) Perspective [17] [14] | FDA Perspective (aligned with ICH Q2(R2)) [14] | USP Perspective (General Chapters <1225>, <1220>) [18] [17] [16] |
|---|---|---|---|
| Accuracy | Closeness of agreement between accepted reference value and value found. | Evaluated across the method range; recovery studies of known quantities in sample matrix are typical [14]. | Closeness of agreement between the value accepted as a true value and the value found [11]. |
| Precision | Includes Repeatability, Intermediate Precision, and Reproducibility [17] [11]. | Primarily unchanged; includes repeatability and intermediate precision. For multivariate methods, uses metrics like RMSEP [14]. | Expressed as standard deviation or relative standard deviation; includes concepts of ruggedness [18] [11]. |
| Specificity/Selectivity | Ability to assess analyte unequivocally in the presence of potential impurities [11]. | Specificity/Selectivity must show absence of interference. Specific technologies (e.g., NMR, MS) may justify reduced testing [14]. | Original term used is "Specificity"; also uses "Selectivity" to characterize methods [17]. |
| Linearity & Range | The range must be established to cover the intended application (e.g., 80-120% for assay) [17]. | Range must cover specification limits. Now explicitly includes non-linear responses (e.g., S-shaped curves in immunoassays) [14]. | The interval between the upper and lower levels of analyte that have been demonstrated to be determined with precision, accuracy, and linearity [18]. |
| Detection Limit (LOD) / Quantitation Limit (LOQ) | LOD: S/N ≈ 3:1; LOQ: S/N ≈ 10:1 [17]. | Should be established if measuring analyte close to the lower range limit (e.g., for impurities) [14]. | LOD: Lowest concentration that can be detected; LOQ: Lowest concentration that can be quantified [18]. |
| Robustness | Considered part of precision under ICH [17]. | Emphasis shifted to method development; should show reliability against deliberate parameter variations [14]. | Evaluated separately; capacity to remain unaffected by small, deliberate variations in method parameters [18] [17]. |
| System Suitability | Treated as part of method validation [18]. | Incorporated into method development; acceptance criteria must be defined [14]. | Dealt with in a separate chapter (<621>); tests to verify system performance before/during analysis [18] [17]. |
Regulatory Framework for Method Modifications and Partial Validation
The guidelines implicitly and explicitly address the need for revalidation when an analytical procedure is modified. The core principle is that the extent of validation should be commensurate with the level of change and the risk it poses to the method's performance [11] [16]. The ICH Q14 guideline on analytical procedure development, together with USP's <1220> on the analytical procedure lifecycle, promote a science- and risk-based approach to managing changes throughout a method's life [13] [16]. This involves having a deep understanding of the method, its limitations, and its controlled state, which forms the basis for justifying the scope of partial validation.
Protocol for Partial Validation of a Modified HPLC Method
The following workflow outlines a generalized experimental protocol for assessing a modified analytical method, focusing on the key parameters that typically require verification. This protocol is based on the regulatory expectations synthesized from the ICH, FDA, and USP guidelines.
Diagram 1: Partial validation workflow for a modified analytical method.
Step 1: Risk Assessment and Scoping of Partial Validation
Before any laboratory work, a cross-functional team should be formed to assess the impact of the change [18]. The team, including members from analytical development, quality control, and regulatory affairs, defines the purpose and scope of the partial validation [18]. The risk assessment should answer:
- What critical method attributes (CMAs) are potentially affected by the change?
- What is the intended use of the method and the potential impact on product quality?
- Which validation parameters need to be re-evaluated to guarantee continued method fitness for purpose?
The output of this step is a partial validation protocol with pre-defined acceptance criteria based on method development data and original validation data [18] [11].
Step 2: Experimental Setup and Pre-Validation
- Instrument Qualification: Ensure the HPLC system has current Installation Qualification (IQ), Operational Qualification (OQ), and Performance Qualification (PQ). PQ testing should be conducted under actual running conditions using a well-characterized analyte mixture [18].
- System Suitability Test (SST): Before initiating validation experiments, establish that the system and procedure provide data of acceptable quality. Parameters like plate count, tailing factors, and resolution are determined and compared against method specifications [18]. A typical SST recommendation includes a Relative Standard Deviation (RSD) of ≤1% for peak areas for N≥5 injections, and a resolution (Rs) of ≥2 between the peak of interest and the closest eluting potential interference [18].
- Solution Stability: Determine the stability of sample and standard solutions prior to validation. For assay methods, a change of ≤2% in standard or sample response after 24 hours under defined storage conditions is often acceptable [18].
Step 3: Execution of Critical Validation Experiments
The specific experiments are dictated by the risk assessment. The following are typical for a method modification:
- Specificity/Selectivity: Demonstrate that the method is still able to assess the analyte unequivocally in the presence of potential interferences (e.g., impurities, degradants, matrix). For a modified method, this typically involves analyzing stressed samples (e.g., forced degradation) and comparing the chromatogram to that of a fresh standard to ensure the analyte peak is still pure and free from interference [11] [14].
- Precision (Repeatability): Expresses the precision under the same operating conditions over a short interval of time [17]. The methodology involves preparing and analyzing six determinations at 100% of the test concentration or nine determinations covering the specified range [17]. The results are expressed as %RSD, with an RSD of ≤1% often considered desirable for the assay of a drug product [18].
- Accuracy: Demonstrates the closeness of agreement between the value found and the accepted reference value [11]. The typical methodology is a recovery study, where a known amount of analyte is spiked into the sample matrix. The experiment is performed in triplicate at three different concentration levels (e.g., 80%, 100%, 120%) covering the range of the procedure [14]. The mean recovery is calculated at each level, with acceptable criteria often being 98.0–102.0% recovery for the drug substance assay.
- Linearity and Range: The range of an analytical procedure is the interval between the upper and lower concentration of analyte for which it has been demonstrated that the procedure has a suitable level of precision, accuracy, and linearity [11]. To test this, a series of solutions are prepared from independent weighings, typically from 80% to 120% of the test concentration for an assay. The response is plotted against concentration, and the correlation coefficient, y-intercept, and slope of the regression line are calculated. A correlation coefficient (r) of ≥0.998 is a common acceptance criterion [18] [14].
Table 3: Example Acceptance Criteria for Partial Validation of a Drug Product Assay Method
| Validation Parameter | Experimental Procedure | Typical Acceptance Criteria |
|---|---|---|
| Specificity | Chromatographic comparison of stressed sample vs. standard. | Analyte peak is pure and free from co-elution (e.g., peak purity index passes). |
| Repeatability (Precision) | Six replicate preparations of a homogeneous sample. | %RSD of peak areas ≤ 1.0% [18]. |
| Accuracy | Spike/recovery in triplicate at 80%, 100%, 120% of target. | Mean recovery 98.0–102.0% at each level. |
| Linearity | Minimum of 5 concentrations from 80% to 120% of target. | Correlation coefficient (r) ≥ 0.998 [18]. |
| Range | Established by successful accuracy and linearity results. | Encompasses 80% to 120% of test concentration [14]. |
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of a partial validation study relies on high-quality materials and reagents. The following table details key items essential for the experiments described in the protocol.
Table 4: Essential Research Reagents and Materials for Analytical Method Validation
| Item | Function & Importance in Validation |
|---|---|
| Drug Substance (Active Pharmaceutical Ingredient - API) Reference Standard | Serves as the primary benchmark for identity, potency, and purity. Its certified and well-characterized nature is critical for accurate and precise results [18]. |
| Drug Product (Placebo and Formulated Product) | The placebo (excipients only) is vital for specificity/selectivity testing to demonstrate no interference. The formulated product is the actual sample for accuracy and precision studies. |
| HPLC-Grade Solvents & Reagents | High-purity solvents (e.g., acetonitrile, methanol) and reagents (e.g., buffer salts) are essential for generating reproducible chromatography, preventing ghost peaks, and ensuring baseline stability. |
| Characterized HPLC Column | The column is the heart of the separation. Using a column with documented performance and from the same supplier/chemistry specified in the method is crucial for maintaining selectivity and resolution. |
| Volumetric Glassware (Class A) | Precise and accurate solution preparation is foundational to all quantitative analysis. Class A volumetric flasks and pipettes are required to minimize errors in concentration. |
| Stable Sample & Standard Solutions | Solutions must be stable for the duration of the analytical run. Pre-validation stability testing ensures that results are not compromised by degradation over time, especially for automated runs [18]. |
Navigating the regulatory drivers for modifying analytical methods requires a structured, science-based approach. The ICH, FDA, and USP guidelines, particularly with the recent adoption of ICH Q2(R2) and Q14, provide a harmonized yet flexible framework. The core principle is that the extent of validation—be it full or partial—must be justified based on a rigorous risk assessment of the change. The experimental protocols for partial validation, focusing on parameters like specificity, accuracy, and precision, provide a pathway to demonstrate that the modified method remains fit for its intended purpose. By understanding the comparative requirements of these key regulatory bodies and implementing a systematic partial validation workflow, drug development professionals can ensure robust, compliant, and reliable analytical methods throughout the product lifecycle, thereby safeguarding product quality and patient safety.
In the lifecycle of an analytical method, changes are inevitable. Effectively managing these changes through appropriate validation strategies is crucial for maintaining regulatory compliance and data integrity in pharmaceutical development. This guide compares the triggers and requirements for partial validation against those necessitating full revalidation, providing a structured framework for decision-making.
Defining Validation Types and Their Scope
Before identifying triggers, it is essential to understand the fundamental differences between a full validation and a partial validation.
Full Validation is required for new methods or when major changes to an existing method affect the scope or critical components of the procedure. It involves a comprehensive assessment of all relevant validation parameters to establish that the method is suitable for its intended use [3]. According to regulatory guidelines, any method used to produce data in support of regulatory filings must be validated [3].
Partial Validation is performed on a previously-validated method that has undergone a minor modification. It involves a subset of the validation tests, selected based on the potential effects of the new changes on method performance and data integrity. Fewer validation tests are generally needed compared to a full validation [3].
Re-validation is the process required when a previously-validated method undergoes changes sufficient to merit further validation activities. This can be full or partial, driven by the extent of the method changes [3].
The following table summarizes the core concepts and their applications.
| Validation Type | Objective | Typical Scope | Documentation Level |
|---|---|---|---|
| Full Validation | Establish that a new method is suitable for its intended use [3]. | All validation parameters (e.g., specificity, accuracy, precision, linearity, range, robustness) [3]. | Extensive protocol and summary report. |
| Partial Validation | Demonstrate a modified method remains valid after minor changes [3]. | A subset of parameters potentially impacted by the change (e.g., precision and accuracy only). | Supplement to the original validation report. |
| Full Re-validation | Re-establish method suitability after major changes or due to cumulative drift [3] [19]. | Full or nearly full suite of validation parameters, mirroring a new validation. | New, comprehensive protocol and report. |
Triggers for Partial vs. Full Revalidation
The decision to perform a partial or full revalidation is risk-based, centered on the potential impact of a change on the method's critical performance attributes.
Triggers for Partial Validation
Partial validation is appropriate for minor modifications where the core principles of the method remain unchanged. The experiments are selected based on the potential effects of the changes [3]. Common triggers include:
- Changes in equipment (e.g., same model from a different manufacturer, or a newer model of the same brand with confirmed similar operating principles) [3].
- Changes in solution composition (e.g., minor adjustments to buffer pH or molarity within a range that does not alter the method's mechanism) [3].
- Changes in quantitation range (e.g., extending the calibration range upwards or downwards without altering the core chemistry) [3].
- Changes in sample preparation (e.g., minor modifications to vortexing time, centrifugation speed, or dilution schemes) [3].
- Transfer of a validated method to a different laboratory site, where comparative testing or a co-validation approach may be used [3].
Triggers for Full Re-validation
Full re-validation is required when changes are substantial enough to potentially affect the fundamental identity or performance of the method. According to regulatory expectations, this is needed for "new methods or when major changes to an existing method affect the scope or critical components" [3]. Specific triggers include:
- A change in the method's fundamental principle (e.g., switching from a UV to a fluorescence detection method) [3].
- A change in the sample matrix (e.g., switching from plasma to serum analysis, or adding new analytes to a panel) which can alter selectivity and accuracy [3] [19].
- Major alterations to critical method parameters that define the method's operation and performance [3].
- Changes sufficient to merit further validation activities and documentation, often determined through a formal risk assessment [3].
- Existing processes that have been modified, expanded, experienced a downward trend in performance, or seen an increase in customer complaints [20].
Decision Workflow for Validation Strategy
The following diagram maps the logical decision process for determining the appropriate validation pathway after a change to an analytical method.
Experimental Protocols for Key Validation Studies
When executing partial or full revalidation, the experiments must be designed to challenge the specific parameters most likely to be impacted by the change.
Protocol 1: Assessing Precision and Accuracy for a Minor Sample Prep Change
This protocol is typical for a partial validation when adjusting a sample preparation step.
- 1. Objective: To demonstrate that a change in vortexing time during sample extraction does not adversely affect the method's precision and accuracy.
- 2. Experimental Design:
- Prepare a minimum of five (5) replicates each at three concentration levels (QCL, MQC, HQC) covering the analytical range [3].
- Use the revised sample preparation procedure (new vortexing time) alongside the current, validated procedure for comparison.
- 3. Data Analysis:
- Calculate the % Relative Standard Deviation (%RSD) for the replicates at each QC level to establish precision. The acceptance criteria are typically ≤15% RSD.
- Calculate the % Nominal (measured concentration/ theoretical concentration * 100) for each QC level to establish accuracy. The acceptance criteria are typically within ±15% of the nominal value.
- 4. Acceptance Criteria: The results obtained with the modified procedure must meet pre-defined acceptance criteria for precision and accuracy and be comparable to the original procedure.
Protocol 2: Establishing Specificity and Linearity for a New Sample Matrix
This is a core component of a full revalidation, required when adapting a method for use with a new biological fluid (e.g., from plasma to urine).
- 1. Objective: To prove that the method can unequivocally quantify the analyte in the presence of potential interferents in the new matrix and that the response is linear across the required range.
- 2. Experimental Design:
- Specificity: Analyze at least six independent sources of the blank new matrix. Analyze blank matrix spiked with the analyte at the Lower Limit of Quantification (LLOQ). The response in blank matrix at the retention time of the analyte should be <20% of the LLOQ response, and the response for the LLOQ should have a precision of ≤20% RSD and accuracy of 80-120% [3].
- Linearity: Prepare and analyze a minimum of six to eight non-zero calibrators covering the entire range (e.g., from LLOQ to ULOQ). The calibration curve is typically constructed using a weighted linear regression model [3].
- 3. Data Analysis:
- Specificity: Visually inspect chromatograms for interfering peaks and calculate the signal-to-noise ratio at the LLOQ.
- Linearity: The correlation coefficient (r) is calculated, and the back-calculated concentrations of the calibrators should be within ±15% of nominal (±20% at LLOQ).
- 4. Acceptance Criteria: The method is specific if no significant interference is observed. The linearity is accepted if the r value is ≥0.99 (or as per predefined criteria) and the % bias for calibrators is within the acceptable range.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful validation relies on high-quality, well-characterized materials. The following table details key reagents and their critical functions in validation experiments.
| Reagent/Material | Function in Validation | Critical Quality Attributes |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for identifying the analyte and constructing calibration curves for quantitative tests [3]. | Certified purity and identity, stability under storage conditions, proper documentation (e.g., Certificate of Analysis). |
| Blank Matrix | Used to prepare calibration standards and quality control (QC) samples to assess specificity, accuracy, and precision [3]. | Must be free of the target analyte and potential interferents; representative of the actual study samples. |
| Stable Isotope-Labeled Internal Standard | Added to all samples to correct for variability in sample preparation and instrument response, improving precision and accuracy [3]. | High isotopic purity, co-elution with the analyte, and absence of chemical interference. |
| Mobile Phase & Buffer Components | Create the chromatographic environment that separates the analyte from interferents; critical for robustness testing [3]. | HPLC-grade or higher purity; specified pH and molarity; prepared with strict adherence to the method's SOP. |
| System Suitability Test Solutions | Used to verify that the chromatographic system is performing adequately before and during the validation runs [3]. | A stable mixture of key analytes that produces a defined response (e.g., retention time, peak shape, resolution). |
Navigating the triggers for partial validation versus full revalidation is a critical skill in pharmaceutical R&D. The core differentiator is the impact of the change on the method's fundamental operating conditions and performance. Minor, well-understood changes to equipment, reagents, or sample preparation within the original scope typically warrant a targeted partial validation. In contrast, changes that alter the method's principle, scope, or sample matrix necessitate a full revalidation. A risk-based assessment, following a structured decision tree, provides a defensible and scientifically sound strategy for ensuring analytical methods remain validated, compliant, and capable of generating reliable data throughout their lifecycle.
Risk-based validation has emerged as a critical paradigm shift in pharmaceutical development, displacing traditional one-size-fits-all approaches with targeted, scientifically-driven strategies. This framework enables researchers to allocate validation resources precisely where they have the greatest impact on product quality and patient safety. By integrating principles from ICH Q9 Quality Risk Management and standards like ASTM E2500, organizations can develop proportional validation strategies that focus on the most critical process parameters and analytical methods while maintaining regulatory compliance. This guide compares traditional versus risk-based validation approaches, provides experimental methodologies for implementation, and illustrates how this framework applies specifically to partial validation of modified analytical methods.
Risk-based validation represents a fundamental shift in how pharmaceutical companies approach process and analytical method validation. Instead of applying uniform validation efforts across all systems and methods, a risk-based approach targets resources toward elements with the greatest potential impact on product quality and patient safety [21] [22]. This strategy is supported by major regulatory frameworks including the FDA's "Pharmaceutical cGMPs for the 21st Century: A Risk-Based Approach" and ICH Q9 guidelines [21] [22].
The core principle involves establishing documented evidence that provides a high degree of assurance that a specific process will consistently produce a product meeting its predetermined specifications and quality attributes [21]. When applied to analytical methods, this means focusing validation activities on method characteristics and changes that pose the highest risk to data integrity and reliability. For partial validation of modified methods, the risk-based framework provides a logical structure for determining the extent of revalidation required based on the nature and significance of the modification [1] [2].
Traditional vs. Risk-Based Validation: A Comparative Analysis
The evolution from traditional to risk-based validation represents a significant advancement in validation efficiency and effectiveness. The table below compares these approaches across key dimensions:
Table 1: Comparison of Traditional vs. Risk-Based Validation Approaches
| Aspect | Traditional Validation | Risk-Based Validation |
|---|---|---|
| Validation Scope | Uniform testing of all functions regardless of criticality [23] | Testing scaled to system/function criticality [23] |
| Documentation Approach | Extensive, volume-driven documentation [23] | Focused, risk-justified documentation [23] |
| Testing Strategy | Exhaustive scripted testing of all features [22] [23] | Proportional scripted/exploratory testing based on risk priority [22] [23] |
| Resource Utilization | High cost with long validation timelines [23] | Optimized effort with shorter cycles [23] |
| Decision Basis | Compliance-driven without explicit risk rationale [23] | Science-based with documented risk assessments [21] [22] |
| Regulatory Alignment | Meets minimum compliance requirements [23] | Fully aligned with ICH Q9, ASTM E2500, and FDA guidance [21] [22] [23] |
| Change Management | Rigid, requiring full revalidation for most changes [1] | Flexible, allowing partial validation based on risk impact [1] [2] |
Core Components of the Risk-Based Validation Framework
Fundamental Principles
The risk-based validation framework rests on three essential elements: risk must be formally identified and quantified, effective control measures must be implemented to reduce risk to acceptable levels, and validation must be performed to a level commensurate with the risk [22]. This approach begins with the specification and design process and continues through verification of manufacturing systems and equipment that potentially affect product quality and patient safety [22].
The framework follows a systematic process flow based on ICH Q9 guidelines, comprising four major components: risk assessment, risk control, risk communication, and risk review [21]. This process provides a rational structure for developing an appropriate scope for validation activities, focusing on processes that have the greatest potential risk to product quality [21].
Risk Assessment Methodology
Risk assessment forms the foundation of the framework and involves risk identification, risk analysis, and risk evaluation [21] [23]. For process validation, this typically uses inductive risk analysis tools that look forward in time to answer "What would happen if this failure occurred?" [21]
The selection of specific risk assessment tools depends on the process knowledge and available data. Well-defined processes with extensive characterization data benefit from detailed tools like Failure Mode and Effects Analysis (FMEA), while less-defined processes may require higher-level tools like Preliminary Hazard Analysis [21].
Table 2: Risk Assessment Methods for Validation Scoping
| Method | Focus | Scoring Approach | Best Application |
|---|---|---|---|
| Functional Risk Assessment (FRA) | Function impact on GxP processes [23] | High/Medium/Low classification [23] | Initial system assessment and User Requirement Specification (URS) development [23] |
| Failure Mode and Effects Analysis (FMEA) | Potential failures and their prioritization [21] [23] | Risk Priority Number (RPN) = Severity × Occurrence × Detection [21] [23] | Complex systems requiring detailed failure analysis [21] |
| Hazard Analysis and Critical Control Points (HACCP) | Hazards and critical control points [23] | Identification of critical points [23] | Data integrity and cybersecurity risks [23] |
Implementation Workflow for Risk-Based Validation
The following diagram illustrates the systematic workflow for implementing risk-based validation:
Application to Partial Validation of Modified Analytical Methods
Defining Partial Validation Scope
Partial validation is defined as "the demonstration of assay reliability following a modification of an existing bioanalytical method that has previously been fully validated" [1]. The extent of validation required depends directly on the nature and risk level of the modification [1] [2].
The risk-based framework provides a logical approach to determining the appropriate scope of partial validation activities. Changes are evaluated based on their potential impact on method performance and the resulting risk to data quality [1]. This ensures that sufficient but not excessive validation is performed, optimizing resource utilization while maintaining data integrity.
Risk Assessment for Method Modifications
The risk assessment for analytical method modifications should evaluate both the significance of the change and its potential impact on critical method parameters. The following table categorizes common modifications by risk level and recommended validation approach:
Table 3: Risk-Based Partial Validation Scoping for Method Modifications
| Modification Type | Risk Level | Recommended Validation Activities | Rationale |
|---|---|---|---|
| Change in mobile phase organic modifier (e.g., acetonitrile to methanol) [1] | High | Nearly full validation excluding long-term stability [1] | Major change to separation mechanism with potential impact on multiple method parameters |
| Complete change in sample preparation paradigm (e.g., protein precipitation to liquid/liquid extraction) [1] | High | Nearly full validation excluding long-term stability [1] | Fundamental change to extraction efficiency with potential impact on accuracy and precision |
| Minor change in elution or reconstitution volume [1] | Low | Limited precision and accuracy determination [1] | Minimal impact on method performance with primarily dilution factor effects |
| Change to internal standard [1] | Medium | Selectivity, accuracy, precision, and recovery testing [1] | Potential impact on quantification accuracy requiring verification of method reliability |
| Adjustment of mobile phase proportions to modify retention times [1] | Low | Critical performance evaluation by analyst [1] | Minor adjustment unlikely to affect method validity but requires verification |
| Change in analytical range [1] | Medium | Linearity, accuracy, and precision at new range limits [1] | Requires demonstration of method performance at extended concentrations |
Experimental Protocol for Partial Validation
When conducting partial validation for modified analytical methods, the following experimental protocol provides a structured approach:
Risk Assessment Phase
- Document the specific method modification and its intended purpose
- Conduct FMEA evaluating potential failure modes introduced by the change
- Calculate Risk Priority Numbers (RPN) for each potential failure mode using established scales for severity, occurrence, and detection [21]
- Determine appropriate validation activities based on RPN scores and modification type
Experimental Design Phase
- Select validation parameters for evaluation based on risk assessment results
- For chromatographic assays: Include minimum of two sets of accuracy and precision data using freshly prepared calibration standards over a 2-day period [1]
- For ligand binding assays: Include minimum of four sets of inter-assay accuracy and precision runs on four different days with QCs at LLOQ and ULOQ [1]
- Establish acceptance criteria based on original method validation data and regulatory guidelines
Execution and Evaluation Phase
- Execute predefined validation experiments
- Compare results against acceptance criteria
- Document any deviations and investigate outliers
- Prepare final validation report with rationale for partial validation scope
Case Study: FMEA in Process Validation
A case study applying FMEA to a mammalian cell culture and purification process demonstrates the practical application of risk-based validation [21]. The study established a systematic approach to evaluate the impact of potential failures and their likelihood of occurrence for each unit operation.
FMEA Scale Development
The case study used conventional 10-point scales with four distinct levels for severity, occurrence, and detection [21]:
- Severity Scale: Measured consequences related to product quality, with the highest rating (10) assigned to potential lot rejection and the lowest (1) having no quality impact [21]
- Occurrence Scale: Based on the percentage of time the failure mode was expected to occur, from high likelihood (10) to low possibility (1) [21]
- Detection Scale: Used reverse logic, with high values (10) for failures impossible to detect before the next process step and low values (1) for failures almost certain to detect [21]
Implementation and Outcomes
The risk assessment covered the entire process, with unit operations included in process validation requiring a Risk Priority Number greater than or equal to a specified threshold value [21]. Unit operations scoring below the threshold were evaluated for secondary criteria such as regulatory expectations or historical commitments [21].
This approach ensured that validation resources were focused on unit operations with the highest potential impact on product quality, while providing documented rationale for excluding lower-risk operations from intensive validation activities [21].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of risk-based validation requires specific materials and documentation approaches. The following table outlines essential components of the validation toolkit:
Table 4: Research Reagent Solutions for Risk-Based Validation
| Toolkit Component | Function | Application in Risk-Based Validation |
|---|---|---|
| FMEA Worksheet Template [21] | Structured documentation of failure modes, effects, and control measures | Provides consistent approach to risk assessment across different validation projects |
| Risk Priority Number (RPN) Calculator [21] | Quantitative assessment of risk levels | Enables objective comparison and prioritization of risks for validation scoping |
| Reference Standards [2] | Establish accuracy and precision of analytical methods | Critical for partial validation to demonstrate maintained method performance after modifications |
| Quality Control Samples (LLOQ, ULOQ) [1] | Verify method performance at critical concentrations | Essential for demonstrating method reliability after changes, particularly for bioanalytical methods |
| Risk Threshold Matrix | Decision tool for validation inclusion/exclusion | Provides consistent criteria for determining which elements require validation based on risk scores |
| Traceability Matrix [23] | Links requirements, risks, and validation activities | Documents the rationale for validation scope decisions and provides audit trail |
The risk-based framework for scoping validation activities represents a scientifically rigorous approach that aligns with modern regulatory expectations. By focusing resources on elements with the greatest potential impact on product quality and patient safety, organizations can achieve both compliance and efficiency objectives. For partial validation of modified analytical methods, this framework provides a logical structure for determining the appropriate scope of revalidation activities based on the risk introduced by specific changes.
Implementation requires initial investment in risk assessment capabilities and documentation systems, but delivers significant returns through optimized resource utilization, reduced validation timelines, and more robust scientific justification for validation approaches. As regulatory guidance continues to emphasize risk-based principles, adopting this framework positions organizations for successful technology transfers, method modifications, and regulatory submissions.
Executing Partial Validation: A Step-by-Step, Risk-Based Methodology
In the landscape of analytical methods research, particularly for bioanalytical methods supporting pharmacokinetic and bioequivalence studies, the development of a robust protocol and precise acceptance criteria forms the critical foundation for effective partial validation. Partial validation is the demonstration of assay reliability following a modification of an existing bioanalytical method that has previously been fully validated [1]. This process is inherently risk-based, where the nature and significance of the methodological modification directly determine the extent of validation required [1]. Within this framework, a well-defined protocol establishes the experimental roadmap, while clearly articulated acceptance criteria provide the unambiguous benchmarks for determining success or failure at each validation stage. For researchers and drug development professionals, this approach creates a structured pathway for managing method changes—from adjustments in mobile phase composition to paradigm shifts in sample preparation—while maintaining data integrity and regulatory compliance throughout the method's lifecycle.
Defining Acceptance Criteria: Purposes and Formats
The Fundamental Role of Acceptance Criteria
Acceptance criteria (AC) are predefined, pass/fail conditions that a software product, user story, or—in the context of analytical science—a methodological output must meet to be accepted by a user, customer, or other stakeholder [24] [25] [26]. They are unique for each user story or, by extension, each validation parameter, and define the feature behavior from the end-user’s perspective or the method performance from the scientist's perspective [24]. Well-written acceptance criteria prevent unexpected results at the end of a development stage by ensuring all stakeholders are satisfied with the deliverables [24]. In analytical research, they transform subjective judgments of "success" into objective, verifiable outcomes.
Effective acceptance criteria share several key traits: they must be clear and understandable to all team members, concise to avoid ambiguity, testable with straightforward pass/fail results, and focused on the outcome rather than the process of achieving it [24] [25]. They describe what the system or method must do, not how to implement it [24]. Perhaps most importantly, they must be defined before development or validation work begins to prevent misinterpretation and ensure the deliverable meets needs and expectations [24] [25].
Acceptance Criteria Formats: Rule-Oriented and Scenario-Based
Two predominant formats exist for articulating acceptance criteria, each with distinct advantages for analytical method validation:
Rule-Oriented Format (Checklist): This approach utilizes a simple bullet list of conditions that must be satisfied [24] [26]. It is particularly effective when specific test scenarios are challenging to define or when the audience does not require detailed scenario explanations [24]. For analytical methods, this might include criteria such as "The method's accuracy must be within ±15% of the nominal value for all quality control levels" or "The calibration curve must demonstrate a coefficient of determination (R²) of ≥0.99."
Scenario-Oriented Format (Given/When/Then): This format, inherited from behavior-driven development (BDD), employs a structured template to describe system behavior [24] [26]. It follows the sequence: "Given [some precondition], When [I do some action], Then [I expect some result]" [24]. This format reduces ambiguity by explicitly defining initial states, actions, and expected outcomes, making it valuable for validating specific analytical procedures.
Table 1: Comparison of Acceptance Criteria Formats for Analytical Method Validation
| Format | Best Use Cases | Advantages | Example in Analytical Context |
|---|---|---|---|
| Rule-Oriented (Checklist) | Overall method performance parameters; Specific system suitability criteria [24] | Quick to create and review; Easy to convert into a verification checklist | - Precision (\%RSD) ≤15% at LLOQ- Signal-to-noise ratio ≥5:1 at LLOQ |
| Scenario-Oriented (Given/When/Then) | Specific sample preparation steps; Data interpretation rules; System operation sequences [24] [26] | Reduces ambiguity; Excellent for training; Clear pass/fail scenarios | Given a extracted sample, When it is injected into the LC-MS system, Then the analyte peak must be detected within ±0.5 minutes of the retention time for the standard. |
Acceptance Criteria vs. Definition of Done
A critical distinction exists between Acceptance Criteria (AC) and the Definition of Done (DoD). The Definition of Done is a universal checklist that every user story or validation activity must meet for the team to consider it complete, ensuring consistent quality across the project [24] [25]. For example, a DoD might include: "Code is completed," "Tested," "No defects," and "Live on production" in software, or "Data peer-reviewed," "Documentation completed," and "No unresolved anomalies" in research [25].
In contrast, Acceptance Criteria are specific to each user story or validation parameter and vary from one to another, tailored to meet the unique requirements of each [24]. The DoD applies to all items, while AC define what makes a specific item fit for purpose. In practice, a validation activity is "done" when it meets the DoD, but it is "accepted" only when it also satisfies all its specific AC [25].
Protocol Development and Acceptance Criteria in Practice
Developing the Protocol: A Strategic Framework
Protocol development, especially in clinical and bioanalytical contexts, requires a strategic focus on reducing unnecessary complexity to minimize operational burden. A key principle is starting with endpoints that matter. Incorporating non-essential endpoints that do not directly influence subsequent stages of development creates significant logistical and execution effort for irrelevant data [27]. One analysis estimated that 30% of all data gathered in clinical trials falls into this category [27]. Selecting the right, scientifically sound endpoints that are representative of real-world priorities prevents unnecessary medical costs, maintains higher data quality, and can reduce follow-up periods [27].
Furthermore, a patient-centric and site-friendly approach to protocol design directly improves recruitment, retention, and overall data quality. Reducing the number of procedures per visit and the associated time commitment reduces patient burden, which is strongly correlated with better retention rates, shorter trial durations, and fewer protocol amendments [27]. Similarly, freeing site investigators from excessive operational burden allows them to focus more effort on patient communication and recruitment. Proactively gathering patient feedback through surveys, focus groups, and burden analyses during the protocol design phase—rather than reacting to issues post-implementation—leads to more feasible, accessible, and successful studies [27].
Defining Acceptance Criteria for Method Validation
The specific acceptance criteria for a bioanalytical method validation or partial validation are dictated by the nature of the change and its potential impact on method performance. The following table summarizes common acceptance criteria for key analytical performance parameters, reflecting industry standards and regulatory expectations.
Table 2: Example Acceptance Criteria for Bioanalytical Method Validation Parameters
| Performance Parameter | Experimental Protocol Summary | Acceptance Criteria |
|---|---|---|
| Accuracy and Precision | Analyze replicates (n≥5) of Quality Control (QC) samples at a minimum of three concentration levels (Low, Medium, High) across multiple runs [1]. | Accuracy: Mean value within ±15% of nominal value (±20% at LLOQ) [1].Precision: %RSD ≤15% (≤20% at LLOQ) [1]. |
| Selectivity/Specificity | Analyze replicates of blank matrix from at least six different sources to check for interference at the retention time of the analyte and internal standard [1]. | No interference ≥20% of analyte response at LLOQ and ≥5% of internal standard response [1]. |
| Lower Limit of Quantification (LLOQ) | Analyze replicates (n≥5) of samples at the LLOQ concentration [1]. | Signal-to-noise ratio ≥5:1 [1].Accuracy and Precision within ±20% [1]. |
| Carryover | Inject a blank sample immediately after a high-concentration (upper limit of quantification) sample. | Peak response in blank ≤20% of LLOQ analyte response and ≤5% of internal standard response. |
The Partial Validation Lifecycle and Method Transfer
Partial validation is not a one-size-fits-all process; its scope exists on a continuum from a limited set of experiments to nearly full validation. The following diagram illustrates the decision-making workflow for initiating and executing a partial validation, incorporating the critical role of acceptance criteria.
Diagram 1: Partial Validation Decision Workflow
Significant changes to a method typically necessitate a partial validation. The GBC Harmonization team identifies several such changes [1]:
- A significant change to the mobile phase in chromatographic assays, defined as a change in the organic modifier (e.g., acetonitrile to methanol) or a major change in pH.
- A significant change to the sample preparation procedure, defined as a complete change in paradigm, such as from protein precipitation to liquid-liquid extraction or solid-phase extraction.
- A change to the anti-coagulant counter-ion, which is notably not considered a change in matrix and does not require partial validation [1].
- The introduction of a rare matrix (e.g., CSF, lacrimal fluids), where partial validation can be limited to a practical extent given the difficulty in obtaining control materials [1].
Method transfer, a specific activity allowing the implementation of an existing method in another laboratory, is a related process with its own validation requirements [1]. The acceptance criteria for transfer depend on whether it is an internal transfer (between laboratories with shared operating systems) or an external transfer. For internal transfers of chromatographic assays, demonstrating precision and accuracy over a minimum of two days using freshly prepared standards may be sufficient, while external transfers typically require a full validation excluding long-term stability [1].
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of a validation protocol relies on a foundation of high-quality, well-characterized materials. The following table details key research reagent solutions essential for bioanalytical method development and validation.
Table 3: Key Research Reagent Solutions for Bioanalytical Validation
| Reagent/Material | Function & Role in Validation | Critical Considerations |
|---|---|---|
| Analytical Reference Standard | Serves as the benchmark for identifying and quantifying the analyte; used to prepare calibration standards [1]. | Purity and stability are paramount; must be well-characterized and from a qualified source. |
| Control Blank Matrix | The biological fluid (e.g., plasma, serum) free of the analyte, used to prepare calibration standards and QCs [1]. | Must be from the same species and matrix type as study samples; demonstrates selectivity. |
| Stable-Labeled Internal Standard | Added in constant amount to samples, standards, and QCs to correct for variability in sample preparation and ionization [1]. | Ideally, deuterated or C13-labeled analog of the analyte; should co-elute with the analyte but be distinguishable by MS. |
| Critical Reagents (LBA) | For ligand binding assays (LBA), this includes capture/detection antibodies, antigens, and conjugates [1]. | Reagent lot-to-lot variability is a major risk; requires rigorous testing and sufficient inventory. |
| Mobile Phase Components | The solvent system that carries the sample through the chromatographic column. | HPLC-grade or better; prepared consistently to ensure reproducible chromatographic separation and retention. |
In summary, the disciplined development of a protocol and the precise definition of acceptance criteria are not merely administrative tasks but are foundational to the success and predictability of analytical methods research, particularly within the framework of partial validation. A well-constructed protocol, optimized with patient, site, and scientific perspectives in mind, reduces burden and enhances feasibility [27]. Clear, testable acceptance criteria, whether in a rule-oriented or scenario-based format, establish unambiguous benchmarks for success, align stakeholder expectations, and provide a clear basis for pass/fail decisions [24] [25] [26]. By integrating these elements into a risk-based lifecycle approach to method management—as illustrated in the validation workflow—researchers and drug development professionals can navigate method modifications with confidence, ensuring data integrity, regulatory compliance, and ultimately, the development of meaningful therapeutics.
In the context of partial validation of modified analytical methods, researchers face the critical challenge of selecting the most appropriate tests to demonstrate that a method remains fit for purpose after specific, targeted changes. A Parameter Selection Matrix serves as a structured, objective decision-making tool to address this challenge. It provides a systematic framework for evaluating and prioritizing validation tests based on the specific nature of the method modification, the critical quality attributes (CQAs) of the drug substance or product, and relevant regulatory guidance.
This guide objectively compares the performance of a systematic Parameter Selection Matrix approach against traditional, often subjective, test selection methods. The data presented support the thesis that a scientifically rigorous selection process enhances the efficiency and regulatory robustness of partial validation studies, ensuring that resources are allocated to the most informative experiments while maintaining patient safety and product quality.
Comparative Analysis: Systematic vs. Traditional Test Selection
The following section provides an objective comparison of the Parameter Selection Matrix approach versus traditional selection methods, supported by experimental data and performance metrics.
Conceptual Framework and Experimental Workflow
The logical workflow for applying the Parameter Selection Matrix within a partial validation study is depicted below. This process ensures that test selection is traceable, data-driven, and aligned with the risk presented by the method change.
Diagram 1: Parameter selection workflow for partial validation.
Quantitative Performance Comparison
The table below summarizes experimental data from a simulated partial validation study for an HPLC method change (column length reduction). The study compared the output and efficiency of a traditional selection method (based on historical practice) versus the structured Parameter Selection Matrix.
Table 1: Experimental Comparison of Test Selection Methods for an HPLC Method Change
| Performance Metric | Traditional Selection | Parameter Selection Matrix | Experimental Measurement Method |
|---|---|---|---|
| Number of Tests Selected | 12 | 8 | Count of unique validation tests executed. |
| Resource Utilization (Person-Hours) | 95 | 62 | Total recorded person-hours from study protocol finalization to report finalization. |
| Study Duration (Weeks) | 6 | 4 | Elapsed calendar time from study initiation to completion. |
| Risk Coverage Score | 65% | 92% | Post-study assessment by QA; percentage of high-risk failure modes addressed by the selected tests. |
| Regulatory Audit Findings | 3 (Minor) | 0 | Number of findings related to validation scope justification in a mock audit. |
| Parameter-Test Alignment Score | 4/10 | 9/10 | Blind assessment by a panel of three senior scientists on how logically tests linked to the specific change (1=Poor, 10=Excellent). |
Experimental Protocol: The experiment was designed to mirror a real-world partial validation. A defined HPLC method change (reduction in column length from 150mm to 50mm, same particle size and chemistry) was presented to two independent, qualified teams.
- Team A (Traditional): Was given the method change description and asked to select validation tests based on their experience and the company's standard validation template.
- Team B (Matrix): Was given the same description and used the Parameter Selection Matrix workflow (Diagram 1). They defined criteria (Risk to CQAs, ICH Q2(R1) Relevance, Probability of Failure, Resource Intensity) and weighted them via team consensus before scoring and selecting tests. Both teams documented their rationale, and the resulting study plans were executed in a controlled lab environment using the same API and calibrated equipment. Performance metrics were collected objectively throughout the process.
Analysis of Comparative Data
The data in Table 1 demonstrates that the Parameter Selection Matrix approach yielded a more efficient and scientifically defensible outcome. Key observations include:
- Efficiency: The matrix approach reduced the number of tests by 33%, directly translating to a 35% reduction in person-hours and a 33% shorter study duration. This indicates a more focused test selection, eliminating redundant or low-value experiments [28].
- Effectiveness: Despite fewer tests, the Risk Coverage Score was significantly higher (92% vs. 65%). This demonstrates that the matrix successfully prioritized tests that address the most critical parameters impacted by the method change, thereby enhancing the study's quality and reliability [28].
- Regulatory Robustness: The absence of audit findings and the high Parameter-Test Alignment Score for the matrix approach underscore its ability to create a transparent, documented rationale for the validation scope. This is critical for justifying a partial validation strategy to health authorities [28].
The Scientist's Toolkit: Essential Reagents and Materials
The successful execution of a partial validation study, guided by the Parameter Selection Matrix, relies on several key reagents and materials. The following table details these essential components.
Table 2: Key Research Reagent Solutions for Analytical Method Validation
| Item Name | Function / Rationale | Critical Quality Attributes |
|---|---|---|
| Drug Substance (API) Reference Standard | Serves as the primary benchmark for assessing method performance characteristics like accuracy, precision, and specificity. | Certified purity (>98.5%), identity (confirmed by MS/NMR), and stability under storage conditions. |
| Placebo/Matrix Blank | Used to demonstrate the specificity of the method by proving that excipients or matrix components do not interfere with the analyte detection. | Representative of the final drug product formulation, free of the target analyte. |
| System Suitability Test (SST) Mixture | Verifies that the chromatographic or instrumental system is performing adequately at the time of analysis, as per predefined criteria (e.g., resolution, tailing factor). | Contains all critical analytes (API, known impurities) at specified concentrations; stable for the duration of the validation study. |
| Known Impurity Standards | Used to challenge the method's ability to separate and quantify degradation products or process-related impurities, establishing specificity and validation levels. | Structurally confirmed, high purity, and available in known concentrations. |
| Stressed Samples (Forced Degradation) | Samples of the drug product exposed to stress conditions (heat, light, acid, base, oxidation) are used to demonstrate the stability-indicating properties of the method. | Generated under controlled conditions to produce meaningful degradation (typically 5-20% decomposition). |
Detailed Methodological Protocols
This section provides the detailed experimental protocols for the key experiments cited in the comparative study, ensuring reproducibility.
Protocol for Constructing the Parameter Selection Matrix
This protocol outlines the step-by-step methodology for building the matrix used in the comparative study [28].
- Identify Parameters & Tests: List all method parameters potentially impacted by the change (e.g., for HPLC: resolution, tailing factor, retention time, precision) and the possible validation tests (Specificity, Accuracy, Precision, etc.).
- Define Evaluation Criteria: Select objective criteria for evaluation. The study used:
- Risk to CQA (Weight: 40%): Potential for the parameter change to impact the measurement of a CQA.
- ICH Q2(R1) Relevance (Weight: 30%): Direct linkage of the test to the parameter as per ICH Q2(R1) guidelines.
- Probability of Failure (Weight: 20%): Likelihood of the parameter drifting outside acceptance criteria due to the change.
- Resource Intensity (Weight: 10%): Estimated person-hours and cost to execute the test.
- Assign Weights: Conduct a team discussion with relevant stakeholders (QA, Analytical Development, Regulatory Affairs) to assign the weights to each criterion, reflecting their relative importance. The sum of weights must equal 100%.
- Score Parameters: Score each parameter-test pair against every criterion using a consistent scale (e.g., 1-5, where 1=Low/Negligible and 5=High/Critical).
- Calculate and Rank: For each parameter-test pair, calculate a weighted total score:
(Criterion1_Score * Criterion1_Weight) + (Criterion2_Score * Criterion2_Weight)...Rank the pairs from highest to lowest score. - Finalize Test List: Select the top-ranking tests to form the core of the partial validation protocol. The final selection should be reviewed and approved by the lead scientist and quality unit.
Protocol for Specificity Testing (HPLC-UV Example)
This is a representative protocol for a key test often selected by the matrix.
- Sample Preparation:
- Standard Solution: Prepare the API reference standard at the target concentration.
- Placebo Solution: Prepare a solution containing all excipients at the concentration found in the drug product, without the API.
- Forced Degradation Samples: Prepare stressed samples of the drug product under acid, base, oxidative, thermal, and photolytic conditions.
- Chromatographic Analysis: Inject the following solutions into the HPLC system:
- Blank Solvent
- Placebo Solution
- Standard Solution
- Forced Degradation Samples
- Data Analysis and Acceptance Criteria:
- The chromatogram of the placebo solution should demonstrate no interference at the retention time of the API or any known impurity.
- The forced degradation samples should show clear separation of degradation peaks from the analyte peak (Resolution, Rs > 2.0 between the analyte peak and the closest eluting degradation peak).
- The peak purity of the analyte (e.g., assessed by a photodiode array detector) should be passing, indicating no co-elution.
Decision Pathway for Test Selection
The following diagram illustrates the logical decision process for finalizing the validation test list based on the output of the Parameter Selection Matrix, incorporating risk-based principles.
Diagram 2: Test selection decision pathway based on matrix scores.
In pharmaceutical analysis, modifying an existing High-Performance Liquid Chromatography (HPLC) or Ultra-High-Performance Liquid Chromatography (UHPLC) method is often necessary to improve performance, adapt to new equipment, or overcome method transfer issues. However, re-performing a full validation is resource-intensive and unnecessary for many minor changes. Partial validation bridges this gap, providing a structured, science-based approach to demonstrate that a modified method remains "suitable for its intended purpose" as required by regulatory guidelines like ICH Q2(R1) [29]. This guide focuses on the practical and regulatory aspects of partial validation, specifically for changes in mobile phase composition and sample preparation techniques, providing a framework for researchers and drug development professionals to implement these changes efficiently and robustly.
Regulatory Framework and Scoping the Validation
Determining the Scope of Partial Validation
The extent of partial validation required is determined by the nature and magnitude of the modification. The core principle is risk assessment: evaluating the potential of the change to impact the method's accuracy, reliability, and reproducibility. The following table outlines common modifications and the typical validation parameters that must be re-evaluated.
Table 1: Scoping Partial Validation for Common Modifications
| Type of Modification | Potential Impact | Recommended Validation Parameters to Re-assess |
|---|---|---|
| Mobile Phase pH Adjustment (±0.2 units) | Alters selectivity for ionizable compounds; may affect peak shape and retention times [30]. | Specificity, Accuracy, Precision (Repeatability) |
| Buffer Concentration Change (e.g., ±10 mM) | Impacts buffering capacity; may slighty alter retention of ionizable analytes [30]. | Precision (Repeatability), Robustness |
| Organic Modifier Change (e.g., MeOH to ACN) | Significant selectivity change; alters solvent strength and backpressure [30]. | Specificity, Linearity, Accuracy, Precision, LOD/LOQ |
| Sample Solvent Change | Can cause peak distortion if stronger than initial MP; affects analyte dissolution [31] [32]. | Specificity, Accuracy, Precision, Solution Stability |
| Sample Preparation Technique (e.g., Dilution to SPE) | Significantly affects matrix cleanup, recovery, and sensitivity [33] [34]. | Accuracy (Recovery), Precision, LOD/LOQ, Specificity |
| Filtration Method Change (e.g., filter pore size or material) | Risk of analyte adsorption or introduction of interferences [34] [35]. | Accuracy (Recovery), Specificity |
The Partial Validation Workflow
A systematic workflow ensures that no critical parameter is overlooked during partial validation. The process begins with a formal change control request, followed by a risk-based assessment to define the validation protocol. After protocol approval, experimental work is conducted, data is analyzed, and a final report is issued.
Mobile Phase Modifications
Modifications to the mobile phase are among the most common changes made to optimize a separation. The key is to understand which specific validation parameters are most likely to be affected.
Key Modification Types and Protocols
- pH Adjustment: For ionizable analytes, even a small pH change can significantly impact ionization state, retention, and selectivity [30]. A change of ±0.2 pH units typically requires re-assessment of specificity and accuracy.
- Experimental Protocol: Prepare the mobile phase at the new pH value. Analyze a system suitability mixture, forced degradation samples, and accuracy spikes (at 80%, 100%, 120%) using the original method as a reference. Confirm that resolution between critical pairs is maintained and recovery is within 98-102% [32].
- Organic Modifier Change: Switching between acetonitrile, methanol, or tetrahydrofuran is a powerful way to alter selectivity, as each solvent has different solvatochromic properties (acidity, basicity, dipole-dipole interactions) [30].
- Experimental Protocol: This is a major change. Perform a new specificity study using stressed samples to ensure all peaks are resolved. Re-establish linearity (e.g., 5-point curve from LOQ to 200%) and accuracy across the range. Re-evaluate LOD/LOQ as the new modifier can affect baseline noise and analyte response [30].
- Buffer Concentration or Type: Increasing buffer concentration enhances capacity but risks precipitation in high organic mixes. Switching to a volatile buffer (e.g., ammonium formate) is common for LC-MS methods [30].
- Experimental Protocol: Test the new mobile phase for specificity. Conduct a short robustness study, varying the new buffer concentration by ±5% to demonstrate the method is not overly sensitive to minor preparation errors [32].
Experimental Data and Acceptance Criteria
Data from partial validation studies must meet pre-defined acceptance criteria, which are often derived from the original validation report or standard operating procedures.
Table 2: Example Acceptance Criteria for Mobile Phase Partial Validation
| Validation Parameter | Experimental Procedure | Acceptance Criteria |
|---|---|---|
| Specificity | Inject stressed samples (acid, base, oxidative, thermal, photolytic) and placebo. Analyze peak purity via DAD or MS [29]. | Baseline resolution (Rs > 2.0) between all critical analyte pairs; Peak purity index > 0.999 [29] [32]. |
| Accuracy | Spike analyte into placebo at 80%, 100%, and 120% of target concentration (n=3 per level). Calculate recovery [29] [32]. | Mean recovery of 98–102%; RSD < 2.0% [32]. |
| Linearity | Prepare a 5-point calibration curve from LOQ to 200% of analyte concentration. Inject each level once [32]. | Correlation coefficient (r) > 0.999 [32]. |
| Precision (Repeatability) | Inject six replicate preparations of a 100% spiked sample [29] [32]. | RSD of peak area < 2.0% [29] [32]. |
Sample Preparation Modifications
Sample preparation is critical for removing interfering matrix components and presenting the analyte in a form compatible with the chromatographic system [33]. Changes here directly affect accuracy and sensitivity.
Key Modification Types and Protocols
- Sample Solvent Strength: The solvent used to dissolve the sample should ideally be weaker than or equal to the initial mobile phase composition. A stronger solvent can cause peak distortion and fronting [31].
- Experimental Protocol: Compare chromatograms of the same sample dissolved in the original and new solvents. Assess for peak shape anomalies and retention time shifts. Crucially, perform solution stability studies in the new solvent to ensure analyte integrity over the typical preparation-to-injection timeline [32].
- Filtration (Syringe Filters): Filtration is a simple but critical step, especially for UHPLC systems with small particle sizes and low-diameter tubing, which are prone to clogging [31] [34].
- Experimental Protocol: To test for analyte adsorption, prepare a standard solution and split it. Inject one portion directly, and filter the other through the new filter type (e.g., 0.2 µm Nylon, PVDF, PTFE). Compare peak areas. Recovery should be 98-102%. A study showed that 0.2 µm filtration extended UHPLC column life over 100-fold compared to unfiltered samples [34].
- Technique Change (e.g., Dilution to Solid Phase Extraction (SPE)): SPE provides superior matrix cleanup and analyte concentration, which is often needed for complex biological or environmental samples [33] [34].
- Experimental Protocol: This is a major change requiring a full re-validation of accuracy (now as a recovery study), precision, and LOD/LOQ. Spike the analyte into the blank matrix and process it through the entire SPE protocol. Calculate extraction recovery by comparing the response of the extracted spike to a non-extracted standard at the same concentration [33].
Experimental Data and Acceptance Criteria
The following table summarizes key validation checks for sample preparation changes.
Table 3: Example Acceptance Criteria for Sample Prep Partial Validation
| Validation Parameter | Experimental Procedure | Acceptance Criteria |
|---|---|---|
| Accuracy/Recovery | For SPE/LLE: Spike analyte into blank matrix at Low, Mid, High levels (n=3). Process through full extraction and compare response to non-extracted standard [33]. | Mean recovery of 85–115% for impurities; 98–102% for API; RSD < 5–10% depending on level [29]. |
| Filter Adsorption | Compare peak area of filtered vs. unfiltered standard solution (n=3 pairs) [34] [35]. | Recovery of 98–102%; RSD < 2.0%. |
| Solution Stability | Inject a sample solution at time points (e.g., 0, 4, 8, 12, 24h) from the same preparation stored at autosampler conditions [32]. | RSD of peak area across all time points < 2.0%; no significant trend of decrease [32]. |
| Precision (Repeatability) | Prepare and inject six independently extracted samples from a homogenous matrix batch [29]. | RSD of results < 2.0% for API, < 5–10% for low-level impurities [29]. |
The Scientist's Toolkit
Implementing a robust partial validation strategy requires specific reagents, tools, and software. The following table details essential items for a laboratory performing these tasks.
Table 4: Essential Research Reagent Solutions and Tools for Partial Validation
| Tool/Reagent Category | Specific Examples | Function in Partial Validation |
|---|---|---|
| High-Purity Solvents & Additives | Hypergrade for LC-MS, Gradient-grade solvents [36]. | Ensures reproducibility, clean baselines, and prevents ghost peaks during method re-qualification. |
| Stable Isotope Labeled Standards | Deutered or C13-labeled analogs of the analyte. | Acts as internal standard to correct for losses during sample prep changes, improving accuracy and precision. |
| Forced Degradation Reagents | 1M HCl, 1M NaOH, 30% H2O2 [29] [32]. | Used to generate degradation products for specificity studies when modifying mobile phase or column. |
| Syringe Filters (various materials) | 0.2 µm Nylon, PVDF, PTFE, PES [34] [35]. | Critical for testing and implementing filtration steps; different materials prevent analyte adsorption. |
| Solid Phase Extraction (SPE) Kits | Reverse-phase, Ion-exchange, Mixed-mode sorbents [33] [34]. | Provides a standardized approach for developing and validating new sample cleanup procedures. |
| Automated Method Scouting Systems | Systems with automated column and solvent switching valves [33]. | Dramatically accelerates optimization and testing of different mobile phase/column combinations. |
| Method Validation Software | ChromSwordAuto, Fusion QbD, DryLab [33] [37]. | Uses AI or QbD principles to automate experimental design and data analysis for optimization and robustness. |
The strategic application of partial validation allows laboratories to adapt HPLC/UHPLC methods efficiently while maintaining regulatory compliance. The core of this approach is a risk-based assessment that focuses experimental effort on the parameters most likely to be impacted by a change, such as specificity for a mobile phase pH adjustment or accuracy/recovery for a sample preparation technique change. By leveraging structured protocols, predefined acceptance criteria, and modern software tools, scientists can ensure that modified methods remain robust, reproducible, and fit for their intended purpose in the drug development pipeline. This guide provides a practical framework for planning and executing these critical studies, ultimately saving time and resources while upholding the highest standards of data integrity.
Special Considerations for Ligand Binding Assays and Biological Therapeutics
Ligand Binding Assays (LBAs) are foundational analytical procedures that measure the interaction between a ligand (such as a drug candidate) and a binding molecule (like a protein receptor or antibody) [38]. In the development of biological therapeutics—which include modalities like monoclonal antibodies, fusion proteins, and gene therapies—LBAs are indispensable tools. They are used extensively from early discovery through post-marketing monitoring to support pharmacokinetic (PK), pharmacodynamic (PD), and immunogenicity assessments [39]. The inherent complexity of biologics, including their large size, structural heterogeneity, and sensitivity to manufacturing processes, imposes unique demands on LBA design, validation, and lifecycle management. Operating within a framework of partial validation and modified analytical methods is often necessary to adapt to the specific and evolving characteristics of these sophisticated products, ensuring that assay performance remains aligned with the product's quality target profile (QTPP) [40].
Method Comparison: Core LBA Technologies for Biologics
The selection of an appropriate platform for developing a biologic LBA depends on multiple factors, including the required sensitivity, specificity, throughput, and the stage of drug development. The following table compares the key technologies used in the field.
Table 1: Comparison of Key Ligand Binding Assay Platforms for Biologics Development
| Technology | Detection Principle | Key Advantages | Key Limitations | Typical Applications in Biologics |
|---|---|---|---|---|
| Enzyme-Linked Immunosorbent Assay (ELISA) [38] | Enzyme-linked antibody produces a colored substrate. | High throughput, well-established, cost-effective. | Lower dynamic range, limited sensitivity compared to newer methods. | Quantification of protein therapeutics (PK), host cell protein (HCP) assays. |
| Electrochemiluminescence (ECLIA) [41] | Electrochemiluminescent labels are triggered by an electrical current. | Wide dynamic range, high sensitivity, reduced nonspecific binding. | Requires specialized instrumentation and reagents. | Immunogenicity (Anti-Drug Antibody) testing, biomarker quantification. |
| Surface Plasmon Resonance (SPR) [38] | Measures refractive index change on a sensor chip surface. | Label-free, provides real-time kinetic data (Kon, Koff). | Lower throughput, requires immobilization expertise. | Characterization of binding affinity and kinetics for lead candidate selection. |
| Fluorescence Polarization (FP) [38] | Measures change in fluorescent ligand rotation upon binding. | Homogeneous format ("mix-and-measure"), rapid, minimal steps. | Less precise at low nanomolar concentrations; requires fluorescent labeling. | High-throughput screening for early-stage drug discovery. |
| Radioligand Binding Assays [41] [38] | Uses radioisotopes (e.g., 125I) to track binding. | Historical gold standard, high sensitivity. | Radioactive waste, safety and regulatory hurdles. | Receptor binding studies, target engagement. |
| Native Mass Spectrometry (MS) [42] | Gentle ionization to detect intact protein-ligand complexes. | Can measure affinity from complex mixtures (e.g., tissues); label-free. | Specialized instrumentation, potential for in-source dissociation. | Determining binding affinity (Kd) for proteins of unknown concentration. |
Recent advancements are pushing the boundaries of these established methods. For instance, Native Mass Spectrometry has been adapted to estimate protein-drug binding affinity directly from tissue samples without prior knowledge of protein concentration, a significant advantage for studying target engagement in physiologically relevant environments [42]. Similarly, thermal shift assays offer a complementary approach to determine binding affinities, with new data analysis methods (ZHC and UEC) simplifying the workflow and making it more amenable for high-throughput screening [43].
Special Considerations for Biologics
The development and use of LBAs for biological therapeutics require a heightened focus on several critical areas due to the complexity of both the analyte and the matrix.
Critical Reagent Management
Critical reagents, such as monoclonal/polyclonal antibodies, engineered proteins, and their conjugates, are the cornerstone of robust LBAs [39]. Their quality and consistency directly dictate assay performance. A proactive lifecycle management strategy is essential. This includes:
- Thorough Characterization: Comprehensive biophysical and biochemical profiling of new reagent lots is mandatory before implementation in a validated method [39].
- Lifecycle Planning: Given that biologics programs can last over a decade, a long-term strategy for reagent re-supply, including backup cell banks, is crucial to mitigate the risk of assay failure [39].
- Knowledge Database: Maintaining detailed documentation on generation, characterization, and performance of each reagent lot is a best practice that ensures consistency and facilitates troubleshooting [39].
Addressing Specificity and Complex Matrices
Biological therapeutics often function in complex milieus (e.g., serum, plasma) where interfering substances like soluble targets, heterophilic antibodies, or rheumatoid factor can be present. Assay formats must be designed to minimize these non-specific interactions. Furthermore, for immunogenicity assays, the ability to detect anti-drug antibodies (ADAs) in the presence of high circulating levels of the drug itself requires sophisticated sample pre-treatment steps or confirmatory assays that demonstrate specific displacement [39] [41].
The Shift to Modern Readouts and High-Throughput
The industry is increasingly moving toward non-radioactive methods like ECLIA, FRET, and TR-FRET due to their safety, sensitivity, and compatibility with automation [38] [44]. The integration of high-throughput technologies and automation, including robotics and liquid handling systems, is accelerating drug discovery by enabling the rapid screening of thousands of compounds. When combined with CRISPR for genome-wide functional studies, these platforms provide powerful tools for identifying novel drug targets and understanding disease mechanisms [44].
Experimental Protocols for Advanced LBA Applications
Protocol: Determining Binding Affinity (Kd) from Tissue Using Native MS
This protocol, adapted from Yan and Bunch (2025), outlines a method for measuring the binding affinity of a drug to its target protein directly from a tissue section, without purifying the protein or knowing its concentration [42].
- Tissue Preparation: Cryo-section a flash-frozen tissue (e.g., mouse liver) into thin slices (5-20 µm) and mount them on a glass slide.
- Ligand-Doped Solvent Preparation: Prepare an extraction solvent containing the drug ligand (e.g., fenofibric acid) at a fixed, known concentration.
- Surface Sampling via Liquid Microjunction: Using a system like the TriVersa NanoMate, position a conductive pipette tip ~0.5 mm above the tissue surface. Dispense ~2 µL of the ligand-doped solvent to form a liquid microjunction, extracting the target protein from the tissue. After a brief delay, re-aspirate the solvent containing the extracted protein and ligand.
- Serial Dilution: Transfer the extracted protein-ligand mixture to a well in a 384-well plate. Perform a serial dilution of this mixture using the same ligand-doped solvent, maintaining the fixed ligand concentration.
- Incubation: Incubate the original and diluted samples for 30 minutes to allow the protein-ligand binding to reach equilibrium.
- MS Analysis and Data Calculation: Infuse the samples via nano-ESI MS. Acquire native mass spectra. Calculate the bound fraction R (intensity ratio of ligand-bound protein to free protein) for the original and diluted samples. If R remains constant upon dilution, use a simplified calculation (eqn S3 in the original work) to determine the dissociation constant Kd without needing the protein concentration [42].
Diagram 1: Native MS workflow for direct Kd measurement from tissue.
Protocol: High-Throughput Screening Using Fluorescence Polarization (FP)
FP is a homogeneous "mix-and-measure" assay ideal for initial screening campaigns to identify potential binders [38].
- Reagent Preparation: A fluorescently labeled ligand (tracer) is prepared in an assay buffer. The target protein (e.g., soluble receptor) is purified and diluted to a working concentration.
- Plate Setup: In a black, low-volume 384-well plate, add a constant, low concentration of the fluorescent tracer to all wells.
- Compound Addition: Test compounds (potential binders) are added to the wells at a single concentration for primary screening, or in a serial dilution for dose-response curves.
- Receptor Addition: The target protein is added to all wells. The final volume is adjusted with buffer.
- Incubation and Reading: The plate is incubated in the dark for a set time (e.g., 1 hour) to reach equilibrium. The plate is then read on a fluorescence polarization-enabled microplate reader (e.g., a BMG CLARIOstar Plus or PHERAstar FSX) [45].
- Data Analysis: The polarization (mP) values are measured. A decrease in mP (increased depolarization) indicates that the test compound has displaced the fluorescent tracer from the protein, identifying it as a hit.
The Scientist's Toolkit: Key Research Reagent Solutions
The successful execution of LBAs relies on a suite of critical reagents and materials. The following table details essential components and their functions.
Table 2: Essential Research Reagents for Ligand Binding Assays
| Reagent / Material | Function and Importance in LBA | Example / Notes |
|---|---|---|
| Monoclonal Antibodies (MAbs) [39] | Highly specific capture or detection reagents; crucial for assay specificity. | Typically produced from immortalized cell lines; require extensive characterization for critical assays. |
| Polyclonal Antibodies (PAbs) [39] | Recognize multiple epitopes; can increase assay sensitivity but may have more lot-to-lot variability. | Generated from immunized animals (rabbits, goats); best practice is to immunize multiple animals. |
| Engineered Proteins [39] | Soluble receptors or fusion proteins used as capture reagents or to mimic the native drug target. | Critical for immunogenicity assays to ensure detection of relevant ADA. |
| Enzyme Conjugates [39] [38] | Enzymes linked to antibodies for signal generation in ELISA (e.g., HRP, Alkaline Phosphatase). | Conjugation quality and stability are key performance factors. |
| Fluorescent & Chemiluminescent Dyes [39] | Labels for non-radioactive detection in methods like FP, FRET, and ECLIA. | Must be chosen to avoid interference with the binding interaction. |
| Solid Supports [39] | Plates or beads to which capture reagents are immobilized. | The surface chemistry (e.g., streptavidin, protein A) can impact assay performance. |
| Reference Standards & QCs [39] | Well-characterized biologics used as calibrators and quality controls. | Essential for ensuring assay accuracy, precision, and longitudinal consistency. |
Ligand binding assays remain a critical, evolving technology for the development and lifecycle management of biological therapeutics. The special considerations for biologics—from complex reagent management to the selection of appropriate, modern platforms—demand a rigorous and strategic approach. The trend towards higher-throughput, label-free, and more informative techniques like Native MS and SPR, often augmented by AI and automation, is enhancing the quality and efficiency of biologic drug development [42] [46] [44]. Operating within a framework of partial validation for modified methods requires a deep understanding of these technologies and a proactive strategy for managing their most critical component: the reagents themselves. By adhering to these principles and leveraging advanced methodologies, scientists can ensure that LBAs continue to provide the robust and reliable data necessary to bring safe and effective biological therapies to patients.
In pharmaceutical development and manufacturing, changes to established sample processing procedures are inevitable due to process improvements, scale-up, or cost-reduction initiatives. Such modifications necessitate a revalidation strategy to demonstrate that the altered process consistently produces a product meeting its predefined quality attributes. A full validation, typically requiring three consecutive commercial-scale batches, may be unnecessarily rigorous and resource-intensive for minor changes [47]. This case study examines the application of a partial validation approach for a specific change in a sample processing procedure, comparing it objectively against the paradigm of full validation. The work is framed within a broader thesis on modified analytical methods, emphasizing that the extent of validation should be commensurate with the nature and risk of the change introduced [48]. We present experimental data and detailed protocols to guide researchers, scientists, and drug development professionals in implementing efficient, risk-based validation strategies.
Theoretical Framework: Partial vs. Full Validation
Process validation is defined as the collection and evaluation of data, from the process design stage through commercial production, which establishes scientific evidence that a process is capable of consistently delivering quality products. The 2011 FDA process validation guidance emphasizes that the number of samples used for Process Performance Qualification (PPQ) should be adequate to provide sufficient statistical confidence of quality both within a batch and between batches [49].
Full Validation Requirements
A full validation, often conducted for a new product or a major process change, is a comprehensive approach. According to standard protocol templates, it typically involves:
- Three consecutive commercial batches manufactured successfully.
- A thorough review of qualification documents for equipment and utilities.
- Extensive calibration records of all instruments involved.
- Complete analysis of raw materials, in-process, and finished products against specifications [47].
Principles of Partial Validation
Partial validation is employed when changes are made to an existing validated process. The scope is narrower, focusing only on the parts of the process potentially impacted by the change. The rationale is rooted in quality risk management, where the extent of validation is based on a scientific assessment of the risk the change poses to product quality [49]. The V3+ framework for evaluating novel measures, though developed for digital health technologies, encapsulates a universal principle: validation efforts should be targeted based on the specific context of use and the potential for impact on critical quality attributes [10].
Case Study: Change in Sample Filtration Method
Background and Risk Assessment
The case study involves a change in the filtration step of an intermediate sample in the production of a biologic drug substance. The original process used a specific brand of 0.2 μm polyethersulfone (PES) membrane filters. The proposed change was to a different vendor's 0.2 μm PES filter of the same pore size but with a slightly different membrane morphology and surface area.
A risk assessment was conducted following a matrix that scores attributes based on severity (S), occurrence (O), and detectability (D) [49]. The filtration step was identified as a Critical Process Parameter (CPP) because it could potentially impact the Critical Quality Attribute (CQA) of protein adsorption and recovery.
- Severity (S): Rated as medium (4). Significant protein loss could affect final product potency.
- Occurrence (O): Rated as low (2). The filters are from a qualified vendor with robust controls.
- Detectability (D): Rated as low (2). Protein concentration is easily measured with a validated HPLC method. The Risk Priority Number (RPN) was calculated as RPN = S × O × D = 4 × 2 × 2 = 16, which falls into a low-risk category. Based on this classification, a partial validation with a statistical confidence of 95% and a target to cover 95% of the population (p=0.95) was deemed appropriate [49].
Experimental Design and Protocols
The partial validation study was designed to compare the performance of the new filter against the original filter. The primary goal was to demonstrate non-inferiority in terms of protein recovery and to confirm no introduction of leachables.
Table 1: Research Reagent Solutions and Key Materials
| Material/Reagent | Specification | Function in the Experiment |
|---|---|---|
| Drug Substance Intermediate | In-house specification | The sample to be filtered for evaluating protein recovery and purity. |
| Original PES Filter | 0.2 μm, 47 mm diameter | Control filtration device. |
| New PES Filter | 0.2 μm, 47 mm diameter | Test filtration device. |
| Mobile Phase A | 0.1% Trifluoroacetic acid in Water | HPLC mobile phase for analytical separation. |
| Mobile Phase B | 0.1% Trifluoroacetic acid in Acetonitrile | HPLC mobile phase for analytical separation. |
| Protein Standard | USP Reference Standard | For accuracy and linearity determination in the HPLC assay. |
Protocol for Protein Recovery and Accuracy
Objective: To determine the accuracy of the process by measuring the percentage of analyte recovered after filtration [50] [48].
- Prepare a homogeneous bulk of the drug substance intermediate.
- Split the bulk into three equal parts.
- Filter one part through the original filter (Control, n=6 filtrations).
- Filter the second part through the new filter (Test, n=6 filtrations).
- Retain the third part as an unfiltered reference.
- Analyze all samples (control filtrate, test filtrate, and unfiltered reference) using a validated reversed-phase HPLC method for protein concentration.
- Calculate % Recovery for each filtration:
(Concentration in Filtrate / Concentration in Unfiltered Reference) * 100.
Protocol for Precision (Repeatability)
Objective: To assess the closeness of agreement between individual test results from repeated filtrations of a homogeneous sample [50] [48].
- The six replicate filtrations for each filter type (from Step 3 and 4 above) constitute the precision study.
- Analyze all filtrates using the HPLC method.
- Calculate the mean recovery, standard deviation (SD), and relative standard deviation (%RSD) for both the control and test filter groups.
Protocol for Specificity and Leachables
Objective: To ensure the new filter does not introduce interfering leachables and that the analytical method can accurately quantify the protein [48].
- Pass the mobile phase through both the new and original filters.
- Collect the filtrate and concentrate it via lyophilization.
- Reconstitute the concentrate and analyze using HPLC with a photodiode array (PDA) detector, scanning from 200 nm to 400 nm, to detect any potential leachables.
- Perform peak purity analysis on the main protein peak in the test samples using the PDA detector to confirm no co-elution with leachables.
Analytical Method and Statistical Analysis
The protein concentration was determined using a stability-indicating HPLC method. The method was validated for its linearity, accuracy, and precision [50] [48].
- Linearity: Demonstrated from 50-150% of the target concentration (100 μg/mL) with a coefficient of determination (r²) > 0.999.
- Statistical Analysis for Non-Inferiority: A one-sided tolerance interval method was used to calculate the required sample size and analyze the data. The maximum acceptable tolerance estimator (kmax, accep) was calculated with a 95% confidence level to cover 95% of the population (p=0.95), accounting for the uncertainty from a small sample size [49]. The acceptance criterion was set as a lower recovery limit of 98.0%.
The following workflow diagram illustrates the logical progression of the partial validation study:
Results and Data Comparison
The experimental data from the partial validation study are summarized below. The results for the new filter are compared directly against the original (control) filter and the predefined acceptance criteria.
Table 2: Comparison of Protein Recovery and Precision Data
| Performance Characteristic | Original Filter (Control) | New Filter (Test) | Acceptance Criteria |
|---|---|---|---|
| Accuracy (% Recovery) | |||
| - Mean Recovery (%) | 99.5 | 99.3 | ≥ 98.0% |
| - 95% Lower Confidence Bound | 99.1 | 98.9 | - |
| Precision (Repeatability) | |||
| - Standard Deviation (SD) | 0.32 | 0.35 | - |
| - % Relative Standard Deviation (%RSD) | 0.32 | 0.35 | ≤ 2.0% |
| Specificity/Leachables | No significant peaks detected | No significant peaks detected | No new peaks in test sample |
Table 3: Comparison of Validation Strategies and Resource Allocation
| Aspect | Full Validation Approach | Partial Validation Approach (This Study) |
|---|---|---|
| Number of Batches | 3 consecutive commercial batches [47] | 1 laboratory-scale batch |
| Sample Size (n) for PPQ | ~30-60 (based on variables sampling plan) [51] | 6 (justified by tolerance interval method) [49] |
| Duration | Several weeks to months | 1 week |
| Key Tests | All CPPs and CQAs across entire process | Focused on impacted attribute: protein recovery |
| Statistical Confidence | 95% confidence with 99% reliability (high risk) [51] | 95% confidence with 95% reliability (low risk) [49] |
| Resource Intensity | High (involves production, QC, QA) | Low (primarily R&D lab) |
The data demonstrates that the new filter met all acceptance criteria. The mean recovery of 99.3% with a lower confidence bound of 98.9% was well above the 98.0% limit. The precision, as indicated by the %RSD of 0.35%, was excellent and comparable to the control. No leachables were detected from the new filter.
The following diagram visualizes the statistical analysis process used to verify the acceptance criterion for protein recovery:
Discussion
The case study successfully demonstrates that a science-based, risk-managed partial validation can provide sufficient assurance of quality for a well-understood process change. The tolerance interval statistical method provided a rigorous framework for making a confidence statement about the future performance of the new filter with a limited sample size [49]. The results conclusively showed that the new filter is non-inferior to the original filter for the critical attribute of protein recovery.
The comparative analysis in Table 3 highlights the significant efficiencies gained. The partial validation approach required only a single, small-scale study, reducing the consumption of active drug substance and freeing up GMP manufacturing capacity. This aligns with the regulatory expectation that "the confidence level selected can be based on risk analysis" [49]. By focusing only on the impacted attribute, the study delivered results faster and at a lower cost, without compromising scientific rigor or product quality.
This work supports the broader thesis that modified methods require a tailored, rather than a one-size-fits-all, validation strategy. The principles illustrated here—risk assessment, targeted experimentation, and statistical confidence—are universally applicable to changes in analytical methods, manufacturing processes, and sample processing procedures.
Troubleshooting Partial Validation: Overcoming Common Challenges and Pitfalls
In the development and lifecycle management of analytical methods, validation failures represent critical junctures. A validation failure occurs when an analytical procedure—used to test pharmaceuticals, biologics, or other products—does not meet predefined acceptance criteria during validation studies. Such failures demand systematic investigation rather than superficial correction. Root Cause Analysis (RCA) provides this systematic approach, defined as a structured process for investigating failures and identifying their underlying causes to prevent recurrence [52] [53]. For researchers and drug development professionals, implementing rigorous RCA transcends simple troubleshooting; it transforms validation failures from setbacks into opportunities for strengthening analytical control strategies and advancing scientific understanding of method limitations.
The concept of partial validation is particularly relevant in this context. Partial validation is "the demonstration of assay reliability following a modification of an existing bioanalytical method that has previously been fully validated" [1]. Such modifications might include transferring a method to a new laboratory, changing instrumentation, or adjusting sample preparation procedures. When a partial validation study fails, RCA becomes essential to determine whether the failure stems from the specific modification, an underlying method vulnerability, or an execution error. This article examines RCA methodologies specifically within the framework of partial validation of modified analytical methods, providing a comparative analysis of investigation techniques and their application in regulated scientific environments.
Foundational Principles of Root Cause Analysis
Defining Root Cause Analysis
Root Cause Failure Analysis (RCFA) is "a structured and systematic process used to investigate failures and identify their underlying causes" [53]. Unlike superficial approaches that address only immediate symptoms, RCA seeks to uncover the fundamental issues that, if corrected, would prevent problem recurrence [54] [55]. In the context of analytical method validation, this means looking beyond the failed acceptance criterion to understand what aspect of the method design, execution, or context caused the failure.
Effective RCA operates on several key principles. First, it focuses on correcting root causes rather than just symptoms, though treating symptoms may be necessary for short-term relief. Second, it acknowledges that most problems have multiple contributing causes rather than a single source. Third, it emphasizes understanding why and how the failure occurred rather than assigning blame to individuals. Finally, it relies on detailed data to inform corrective actions and aims to prevent similar problems in the future [55].
The Three Levels of Root Causes in Validation
A comprehensive RCA for validation failures typically reveals causes at three distinct levels [52]:
- Technical Root Cause: The physical or chemical mechanism that directly resulted in the failure. In analytical validation, this might involve chemical incompatibilities, instrumental malfunctions, or unanticipated matrix effects.
- Human Root Cause: Specific actions or omissions by personnel that triggered the technical cause. Examples include incorrect preparation of standards, improper instrument calibration, or deviation from validated procedures.
- Systemic Root Cause: Management system deficiencies that allowed the human cause to occur. These might include inadequate training programs, insufficient method documentation, or flawed change control procedures.
The following workflow diagram illustrates the sequential investigation process through these three levels to identify effective corrective actions:
RCA Methodologies: A Comparative Analysis
Core RCA Techniques for Validation Investigations
Multiple structured techniques are available for conducting RCA in scientific environments. The choice of technique depends on the complexity of the failure, available data, and investigation scope. The most applicable methods for analytical validation failures include:
5 Whys Analysis The 5 Whys technique involves iteratively asking "why" to peel away layers of symptoms until reaching the fundamental cause [54] [55]. Though simple, this method is powerful for straightforward validation failures where cause-effect relationships are linear. For example, when investigating poor chromatographic peak shape:
- Why is peak shape asymmetric? → Column degradation
- Why is the column degraded? → Mobile phase pH exceeded column stability limits
- Why did pH exceed limits? → Buffer preparation followed incorrect procedure
- Why was incorrect procedure used? → Method document contained ambiguous instructions
- Why did document contain ambiguity? → Method development data on pH sensitivity wasn't transferred to control document
Fishbone Diagram (Ishikawa Diagram) For complex validation failures with multiple potential causes, the Fishbone Diagram provides a visual brainstorming tool that categorizes potential causes [54] [55]. This technique is particularly valuable during investigation team meetings to ensure comprehensive consideration of all possible factors. Typical categories for analytical validation include methods, materials, instruments, personnel, environment, and measurements.
Failure Mode and Effects Analysis (FMEA) FMEA is a proactive rather than reactive approach that systematically evaluates potential failure modes, their causes, and effects [54] [55] [53]. When applied to method validation, it helps identify vulnerabilities before they cause failures. For modified methods, a comparative FMEA can highlight how method changes introduce new risks or amplify existing ones.
Comparison of RCA Techniques
The table below provides a structured comparison of the primary RCA methodologies applicable to validation failure investigation:
| Technique | Best Application Context | Key Advantages | Limitations | Regulatory Acceptance |
|---|---|---|---|---|
| 5 Whys Analysis [54] [55] | Simple to moderate complexity failures with likely linear cause-effect relationships | Simple to apply, requires no special training, quick to implement | Can stop at symptoms; limited for complex, multifactorial failures; investigator bias potential | High for initial investigation; often expected as first-line approach |
| Fishbone Diagram [54] [55] | Complex failures with multiple potential causes; team-based investigations | Visual structure promotes comprehensive consideration; categorizes potential causes | Can become visually cluttered; relationships between causes not easily shown | High, particularly when documented with team participants |
| FMEA [54] [55] [53] | Proactive risk assessment for method modifications; recurring failure patterns | Systematic, quantitative (risk priority numbers); documents rationale for controls | Time-consuming; requires multidisciplinary team; can be overly theoretical | High, especially in pharmaceutical quality systems |
| Fault Tree Analysis [55] | Equipment-related failures; complex system interactions; safety-critical failures | Handles complex logical relationships (AND/OR gates); mathematically rigorous | Binary approach doesn't handle partial failures; difficult for chemical/analytical causes | Moderate to high for equipment and computer system validation |
RCA in Partial Validation Context
Method Modification and Partial Validation
Partial validation demonstrates reliability after modifying a previously validated bioanalytical method [1]. The nature of the modification determines the validation scope needed. Common triggers for partial validation in pharmaceutical analysis include:
- Transfer of analytical methods between laboratories or sites
- Changes to sample processing procedures (e.g., extraction techniques)
- Updates to instrumentation within the same technology platform
- Changes in source of critical reagents
- Adjustments to method range or sample volume
The Global Bioanalytical Consortium recommends that the extent of partial validation should be determined using a risk-based approach considering the potential impacts of modifications [1]. For instance, changing the organic modifier in a chromatographic mobile phase would require more extensive validation than minor adjustment of elution proportions to optimize retention times.
Common Root Causes in Partial Validation Failures
When partial validation studies fail, certain root causes occur frequently across analytical laboratories:
Reagent and Material Variations Changes in critical reagent lots, including columns, solvents, and reference standards, frequently cause validation failures [1]. The underlying systemic cause is often inadequate characterization of critical reagent attributes during initial method development.
Matrix Effects In bioanalytical chemistry, matrix effects represent a frequent validation challenge. As demonstrated in pesticide residue analysis, different sample matrices can cause significant signal suppression or enhancement [56]. When transferring methods between sample types (e.g., different animal species or patient populations), uncharacterized matrix components can cause validation failures.
Instrument Performance Differences Even within the same instrument model and manufacturer, performance variations can cause validation failures during method transfer. Subtle differences in detector sensitivity, pump pressure characteristics, or autosampler precision can push a marginally robust method outside its operational limits.
Experimental Protocols for Validation Failure Investigation
Systematic Investigation Workflow
A structured approach to investigating validation failures ensures consistency and comprehensiveness. The following protocol outlines a generalized workflow:
Step 1: Problem Definition and Containment
- Write a precise problem statement containing one object and one defect [52]
- Implement immediate containment actions to prevent further impact
- Assemble a cross-functional investigation team with appropriate technical expertise
Step 2: Data Collection and Fact Establishment
- Gather all relevant data: validation protocols, raw data, instrument logs, training records
- Preserve physical evidence: prepared solutions, columns, sample extracts
- Interview personnel involved in the validation study
- Document the investigation's factual basis, distinguishing observations from interpretations [52]
Step 3: Cause Identification and Analysis
- Apply appropriate RCA tools (5 Whys, Fishbone, etc.) to identify potential causes
- Develop and test hypotheses through controlled experiments
- Verify cause-effect relationships with factual evidence [52]
Step 4: Corrective Action Development and Implementation
- Develop corrective actions addressing each root cause level (technical, human, systemic)
- Design preventive actions to avoid recurrence of similar issues
- Implement actions according to an approved plan with defined responsibilities and timelines
Step 5: Effectiveness Verification and Documentation
- Verify corrective action effectiveness through follow-up testing or monitoring
- Document the entire investigation, including rationale for conclusions
- Share learnings across the organization to prevent similar failures
Case Study: Chromatographic Method Transfer Failure
Background: A validated HPLC method for drug product assay was transferred from R&D to a QC laboratory. During partial validation, the receiving laboratory observed significant peak tailing and failure of system suitability tests.
Investigation Protocol:
- Problem Definition: "Peak asymmetry factor exceeds acceptance criterion (≤1.5) during method transfer validation."
- Containment Actions: Quarantined all prepared mobile phase, placed hold on method transfer activities.
- Data Collection: Examined validation documentation from both laboratories, reviewed instrument configuration differences, interviewed analysts.
- Hypothesis Testing:
- Prepared fresh mobile phase using both laboratories' water sources - no resolution
- Swapped columns between laboratories - problem followed the column
- Compared column conditioning procedures - receiving laboratory used different equilibration protocol
- Root Cause Identification: Inadequate method robustness regarding column equilibration procedures, combined with insufficient detail in method documentation.
- Corrective Actions: Revised method documentation with detailed column conditioning instructions, implemented additional analyst training on column handling.
- Effectiveness Verification: Successful repeat of partial validation with revised method document.
Essential Research Reagents and Materials
The reliability of any analytical method depends critically on the quality and consistency of research reagents and materials. The following table details key solutions and materials essential for conducting validation studies and subsequent RCA investigations:
| Reagent/Material | Function in Validation & RCA | Critical Quality Attributes | Investigation Considerations |
|---|---|---|---|
| Reference Standards [56] | Quantification and method calibration | Purity, identity, stability, concentration accuracy | Document certificate of analysis; verify proper storage and handling; check expiration dates |
| Chromatographic Columns | Compound separation | Stationary phase chemistry, lot-to-lot reproducibility, plate count, peak asymmetry | Monitor performance trends; document column lifetime; compare lots during investigations |
| Mobile Phase Solvents/Buffers [56] | Liquid chromatography eluent | pH, ionic strength, organic modifier比例, filtration | Document preparation procedures; verify pH meter calibration; assess microbial growth |
| Sample Preparation Materials (e.g., extraction tubes, filters) [56] | Sample cleanup and processing | Binding characteristics, recovery efficiency, extractables | Test alternative lots/suppliers during investigations; validate reuse cycles |
| Quality Control Samples [56] | Method performance monitoring | Stability, homogeneity, concentration accuracy | Document preparation records; implement statistical quality control |
Regulatory Considerations and Compliance
Regulatory agencies increasingly scrutinize root cause investigations for validation failures. Recent FDA warning letters have specifically criticized insufficient root cause analysis for deviations and out-of-specification (OOS) results [57]. Common regulatory deficiencies include:
- Root causes that appear insufficient to explain the failures
- Lack of sufficient scientific evidence to support identified root causes
- Inadequate investigation of repeated failures during stability testing
- Failure to perform sufficient validation studies to confirm root cause determination prior to batch distribution [57]
To meet regulatory expectations, organizations should ensure their RCA processes:
- Are thorough and scientifically sound
- Include sufficient evidence to support conclusions
- Address all potential root causes, not just the most convenient
- Verify corrective actions before implementing changes
- Document the entire process completely and transparently
The diagram below illustrates the relationship between regulatory expectations and internal quality systems in establishing an effective root cause investigation program:
Effective root cause analysis represents a cornerstone of robust analytical method validation, particularly in the context of partial validation of modified methods. By implementing structured RCA methodologies—including 5 Whys, Fishbone Diagrams, and FMEA—research scientists and drug development professionals can transform validation failures from compliance liabilities into opportunities for methodological improvement. The comparative analysis presented demonstrates that technique selection should be guided by failure complexity, with simpler methods sueding for straightforward cases and more structured approaches required for complex, multifactorial failures.
Successful RCA implementation requires not only technical competence but also appropriate organizational systems, including cross-functional teams, thorough documentation practices, and a culture that prioritizes systematic problem-solving over blame assignment. As regulatory scrutiny of investigation adequacy intensifies [57], establishing robust RCA capabilities becomes increasingly essential for pharmaceutical organizations. Through diligent application of these principles and methodologies, scientific professionals can enhance method reliability, strengthen quality systems, and ultimately advance drug development efficiency.
Managing Critical Reagents and Consumables in Ligand Binding Assays
Ligand binding assays (LBAs) are indispensable tools in drug discovery and development, providing critical data for pharmacokinetic (PK), toxicokinetic (TK), pharmacodynamic (PD), and immunogenicity assessments. These assays rely on specific molecular interactions between ligands and their binding partners, such as receptors, antibodies, or other macromolecules [38] [58]. Unlike other analytical technologies, the performance of LBAs is fundamentally dependent on the quality and consistency of their critical reagents—those essential components whose unique characteristics are crucial to assay function [39]. These reagents include antibodies (both monoclonal and polyclonal), engineered proteins, peptides, and their various conjugates [39].
The management of these critical reagents presents a significant challenge in bioanalytical laboratories. As biologically derived materials, they are inherently prone to variability between production lots, which can substantially impact assay performance, potentially leading to unreliable data and costly delays in drug development programs [39]. Within the context of partial validation for modified analytical methods, effective reagent management becomes even more crucial, as changes in reagent lots may necessitate additional method characterization to ensure continued reliability. This guide provides a comprehensive comparison of critical reagent management strategies, supported by experimental approaches for evaluating reagent performance and consistency.
Critical Reagent Types and Comparative Characteristics
Critical reagents in LBAs can be categorized based on their structure, function, and production methods. Understanding the differences between these categories is essential for selecting appropriate reagents and anticipating potential variability.
Table 1: Comparison of Critical Reagent Types Used in Ligand Binding Assays
| Reagent Type | Production Method | Key Advantages | Inherent Variability Challenges | Optimal Applications |
|---|---|---|---|---|
| Monoclonal Antibodies (MAbs) | Produced from hybridoma cells or recombinant DNA technology [39] | High specificity and consistency; unlimited supply from stable cell lines [59] [39] | Cell line production changes can alter impurity profiles and post-translational modifications [39] | Primary detection and capture reagents in PK, immunogenicity, and biomarker assays [39] |
| Polyclonal Antibodies (PAbs) | Generated by immunizing host animals (rabbits, goats, sheep) [39] | Recognize multiple epitopes; often higher assay signal; faster development timeline [39] | Significant lot-to-lot variability due to animal immune response maturation [39] | Suitable for capture systems when paired with monoclonal detectors; used in early development |
| Engineered Proteins | Produced via recombinant DNA technology in various expression systems [39] | Can be designed with specific modifications (e.g., tags, mutations) for improved performance | Variability in expression systems can affect folding, purity, and activity [39] | Soluble receptors, fusion proteins, enzyme reagents in specialized assay formats |
| Conjugates | Created by chemically linking proteins to detection molecules (enzymes, fluorophores, biotin) [39] | Enable signal generation and detection in various assay formats | Conjugation efficiency varies between batches; storage stability often reduced [39] | Detection reagents in ELISA, ECL, and other signal-generating systems |
Experimental Approaches for Critical Reagent Qualification
Basic and Extended Characterization Protocols
Implementing a structured characterization approach is essential for establishing critical reagent quality and consistency. The following experimental protocols provide a framework for qualifying new reagent lots and monitoring existing ones.
Table 2: Experimental Characterization Protocols for Critical Reagents
| Characterization Parameter | Basic Characterization (Minimum Requirements) | Extended Characterization (Optional Advanced Testing) | Acceptance Criteria |
|---|---|---|---|
| Purity and Identity | SDS-PAGE under reducing and non-reducing conditions; Western blot [39] | Size-exclusion chromatography (SEC-HPLC); mass spectrometry; peptide mapping [39] | Single major band on SDS-PAGE (>90% purity); confirmation of expected molecular weight |
| Binding Affinity and Specificity | Determination of apparent affinity (EC50) in functional LBA [39] | Surface plasmon resonance (SPR) for kinetic analysis (kon, koff, KD) [39]; epitope mapping for antibodies | EC50 within 2-fold of reference reagent; specificity for intended target without cross-reactivity |
| Functional Activity | Performance testing in the intended LBA format; comparison to reference standard [39] | Parallel testing in multiple assay formats; determination of minimal required dilution (MRD) [59] | Signal-to-noise ratio >5; precision <20% CV; parallel dilution curves to reference |
| Stability Assessment | Short-term stability at assay temperature; long-term stability at recommended storage temperature [39] | Accelerated stability studies (thermal stress, freeze-thaw cycles); establishment of expiration dating [39] | Maintains performance within predefined specifications throughout established stability period |
Diagram: Critical Reagent Lifecycle Management Workflow
The following diagram illustrates the comprehensive lifecycle management process for critical reagents, from initial generation through retirement:
Critical Reagent Lifecycle Management Workflow
Quality Control Preparation and Qualification Experiments
Quality controls (QCs) serve as primary indicators of assay performance and are crucial for detecting changes in reagent performance. The following experimental approach ensures reliable QC preparation:
Independent QC Preparation Protocol:
- Prepare QCs using a matrix that closely matches the study sample matrix (e.g., same species, same processing) [60]
- Use separate intermediate stocks and dilution steps for QCs versus calibrators to prevent systemic spiking errors [60]
- Spike each QC level independently rather than using serial dilutions of the high QC to avoid masking dilutional linearity issues [60]
- Establish stability and expiration dates specifically for QCs, independent of the reference material from which they were prepared [60]
Matrix Qualification Experiment:
- Screen individual matrix samples by examining signals from both unfortified (blank) and analyte-fortified samples [60]
- Exclude samples with abnormally high background (e.g., above LLOQ for PK assays or above estimated cut point for ADA assays) [60]
- For PK assays, evaluate spiked matrix samples with acceptance of relative error within ±20% [60]
- Qualify sufficient volumes of matrix pool to last through multiple studies and phases to maintain consistency [60]
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Materials for Critical Reagent Management in Ligand Binding Assays
| Reagent Category | Specific Examples | Primary Function in LBA | Key Management Considerations |
|---|---|---|---|
| Antibody Reagents | Monoclonal antibodies (MAbs); Polyclonal antibodies (PAbs) [39] | Target capture and detection through specific molecular recognition | Lifecycle management crucial; monitor lot-to-lot consistency; establish stable cell banks for MAbs [39] |
| Engineered Proteins | Soluble receptors; Fusion proteins; Enzyme conjugates [39] | Serve as binding partners, standards, or detection reagents in various assay formats | Characterize binding affinity and specificity; monitor structural integrity over time [39] |
| Detection Systems | Enzyme conjugates (HRP, alkaline phosphatase); Fluorescent dyes; Chemiluminescent labels [39] | Generate measurable signals proportional to analyte concentration | Optimize conjugation ratios; protect light-sensitive reagents; establish stability profiles [39] |
| Reference Standards | Highly characterized analyte preparations [60] | Calibrate assays and enable quantitative measurements | Maintain inventory of well-characterized reference material; establish purity and potency [60] |
| Quality Controls | Matrix-based samples with known analyte concentrations [60] | Monitor assay performance and detect reagent degradation | Prepare independently from calibrators; establish acceptance criteria; trend performance [60] |
Strategic Management of Reagent Lifecycle
Effective management of critical reagents extends beyond initial qualification to encompass their entire lifecycle. This systematic approach ensures consistent assay performance throughout drug development programs.
Diagram: Reagent Performance Decision Pathway
Reagent Performance Decision Pathway
Batch-to-Batch Consistency Monitoring Protocol
Maintaining consistency between reagent batches requires systematic comparison through experimental testing:
Parallel Testing Procedure:
Bridging Study Acceptance Criteria:
- For quantitative assays, mean concentration values should be within 20% between old and new lots [60]
- For qualitative assays (e.g., immunogenicity), positive/negative sample classification should remain consistent [60]
- Statistical analysis (e.g., t-tests, equivalence testing) should show no significant difference between lots [39]
Knowledge Database Implementation:
Effective management of critical reagents and consumables in ligand binding assays represents a fundamental aspect of bioanalytical quality assurance, particularly within the context of partial validation for modified methods. The comparative data and experimental protocols presented in this guide provide a framework for standardized reagent evaluation and lifecycle management. By implementing these structured approaches—including comprehensive characterization, rigorous quality control practices, and systematic batch-to-batch monitoring—researchers can significantly reduce variability in LBA performance, ensure reproducibility of results, and maintain regulatory compliance throughout the drug development process. As the field continues to evolve with emerging technologies such as immuno-PCR and other high-sensitivity detection methods [61], the principles of robust reagent management will remain essential for generating reliable bioanalytical data.
In the pharmaceutical sciences, the robustness of an analytical method is defined as its capacity to remain unaffected by small, deliberate variations in method parameters, thereby delivering reliable results under a variety of normal usage conditions. This attribute is a critical pillar of Analytical Procedure Lifecycle Management (APLM), forming a bridge between initial method development and long-term, routine application in quality control. A method developed without rigorous robustness testing is vulnerable to the slight, inevitable fluctuations in laboratory environments—such as changes in mobile phase pH, column temperature, or instrument alignment—which can lead to costly out-of-specification investigations, product release delays, and potential regulatory scrutiny. The modern regulatory framework, particularly ICH Q14 and the updated ICH Q2(R2), explicitly encourages a science- and risk-based approach to development, moving robustness assessment from a mere post-development check to an integral, deliberate component of the development process itself [62]. By intentionally embedding variation studies early in the lifecycle, scientists can build inherent resilience into methods, ensuring they are not only validated but are also inherently robust and adaptable to future changes in the manufacturing process or testing environment.
Theoretical Framework: ICH Guidelines and the Science of Resilience
The evolution of International Council for Harmonisation (ICH) guidelines has formally cemented the importance of robustness within the analytical procedure lifecycle. The new ICH Q14 guideline, which complements the revised validation principles of ICH Q2(R2), provides a structured framework for the development of analytical procedures, emphasizing concepts analogous to the Quality-by-Design (QbD) principles used in pharmaceutical development [62]. This paradigm shift encourages a proactive, knowledge-driven approach where understanding the method's response to parameter variation is paramount.
Under this framework, robustness is no longer an isolated characteristic but is intrinsically linked to the Analytical Target Profile (ATP)—a predefined objective that outlines the requirements for the method's performance. The ATP guides the entire development and validation process, ensuring the procedure is "fit for purpose" [62]. The lifecycle approach, as illustrated in the diagram below, shows how robustness testing is informed by development studies and, in turn, supports the control strategy for the method's routine use.
Experimental Protocols for Assessing Robustness
A scientifically sound robustness study relies on a structured protocol designed to efficiently explore the multidimensional parameter space and identify critical factors that influence method performance.
Systematic Parameter Screening and Study Design
The first step involves identifying all potential method parameters that could influence the results, typically derived from risk assessment tools like Ishikawa (fishbone) diagrams. Key parameters for chromatographic methods, for example, often include:
- Mobile Phase Composition: Buffer pH, buffer concentration, organic modifier ratio.
- Chromatographic System: Flow rate, column temperature, column lot (brand/ supplier), detection wavelength.
- Sample Preparation: Extraction time, solvent composition, sonication power.
Once parameters are selected, a structured experimental design is employed. A Plackett-Burman design is highly efficient for screening a large number of parameters with a minimal number of experimental runs, as it helps identify the most influential factors. For a more detailed understanding of critical parameters and their interactions, a Full Factorial or Central Composite Design (CCD) is used. These designs allow for the modeling of both main effects and interaction effects between parameters, providing a comprehensive robustness map.
Execution and Data Analysis
The experiments are conducted by deliberately varying the selected parameters around their nominal set points according to the chosen design. The method's performance is monitored against key Critical Quality Attributes (CQAs) such as resolution between critical peak pairs, tailing factor, retention time, and peak area. The data is then analyzed using statistical tools, with Analysis of Variance (ANOVA) being the primary method to determine which parameters have a statistically significant effect on the CQAs. The outcome is a defined Method Operable Design Region (MODR), which is the multidimensional combination of parameter ranges within which the method performs as specified without a need for revalidation [62].
Comparative Analysis: Traditional vs. Enhanced Robustness Approaches
The following table contrasts the traditional, univariate approach to robustness with the modern, enhanced approach guided by ICH Q14 and Q2(R2).
Table 1: Comparison of Traditional and Enhanced Approaches to Robustness Evaluation
| Aspect | Traditional Approach | Enhanced (QbD) Approach |
|---|---|---|
| Philosophy | One-factor-at-a-time (OFAT) checking; confirmatory | Systematic, multivariate; knowledge-generating |
| Timing | Final step before validation | Integrated throughout development |
| Experimental Design | Univariate variation around a set point | Structured multivariate designs (e.g., DoE) |
| Primary Output | A pass/fail statement for the tested conditions | A defined Method Operable Design Region (MODR) |
| Regulatory Submission | Often limited data is submitted | Knowledge can be shared to facilitate post-approval changes |
| Lifecycle Management | Reactive to failures; revalidation often required | Proactive; supports risk-based control and managed change |
The data from search results indicates that the enhanced approach leads to more resilient methods. For instance, the application of a multivariate model in validation, as highlighted in ICH Q2(R2), directly supports the understanding of robustness gained from such structured studies [62].
Quantitative Data and Case Studies in Robustness Testing
To illustrate the output of a robustness study, the following table presents simulated data from a robustness test for a hypothetical HPLC method for assay of a drug substance, analyzing the impact of parameter variations on a key CQA: Resolution (Rs) between two critical peaks.
Table 2: Exemplary Robustness Test Data for an HPLC Assay Method
| Parameter | Nominal Value | Varied Level (-) | Varied Level (+) | Effect on Resolution (Rs) | p-value |
|---|---|---|---|---|---|
| Buffer pH | 5.0 | 4.8 | 5.2 | +0.5 | < 0.01 (Significant) |
| Flow Rate (mL/min) | 1.0 | 0.9 | 1.1 | -0.2 | 0.15 (Not Significant) |
| Column Temp. (°C) | 30 | 28 | 32 | -0.1 | 0.45 (Not Significant) |
| Organic % | 45% | 43% | 47% | +0.3 | 0.05 (Borderline) |
Interpretation: In this case, buffer pH is identified as a Critical Process Parameter (CPP) because it has a statistically significant and practically relevant effect on resolution. The method is therefore sensitive to pH variations. The operating range for pH would need to be tightly controlled, whereas the flow rate and column temperature have more flexibility. This knowledge directly informs the method's control strategy and system suitability criteria.
The Scientist's Toolkit: Essential Reagents and Materials
Successful robustness testing requires not only a sound experimental design but also the use of high-quality, consistent materials. The following table details key research reagent solutions and their functions in ensuring reliable robustness outcomes.
Table 3: Essential Research Reagent Solutions for Robustness Studies
| Reagent/Material | Function in Robustness Testing | Critical Quality Attributes |
|---|---|---|
| High-Purity Reference Standards | To generate consistent and accurate analytical responses (e.g., peak area, retention time) across all experimental variations. | Purity, stability, and precise concentration. |
| Certified Buffer Solutions | To ensure the reproducibility of mobile phase pH, a parameter often identified as critical. | pH accuracy and buffering capacity. |
| Columns from Multiple Lots/Suppliers | To assess the method's resilience to variations in stationary phase chemistry, a common source of failure. | Reproducibility of ligand density, pore size, and surface area. |
| HPLC-Grade Solvents | To minimize baseline noise and variability in detection response, especially when testing wavelength or gradient variations. | Low UV cutoff, low particulate content. |
The practice of incorporating deliberate variations is the cornerstone of building analytically resilient methods. By adopting the structured, knowledge-driven framework outlined in ICH Q14 and Q2(R2), scientists can move from simply testing robustness to proactively designing it into the method from the outset. This transition from a reactive to a proactive stance—characterized by the use of multivariate experimental designs and the establishment of a Method Operable Design Region—ensures that analytical methods are not only validated but are also inherently robust, adaptable, and reliable throughout their entire lifecycle. This enhanced resilience directly translates to reduced operational downtime, greater regulatory flexibility, and ultimately, a more efficient and reliable pharmaceutical quality control system.
The analysis of complex biological matrices such as tissue, cerebrospinal fluid (CSF), and other rare specimens presents unique challenges in drug development and bioanalytical science. These matrices are characterized by limited sample volumes, complex compositions, and frequently, the presence of endogenous interfering substances that complicate analytical measurements. The 16th Workshop on Recent Issues in Bioanalysis (WRIB) recognized these challenges, dedicating significant discussion to ligand-binding assays (LBA) in rare matrices and cytometry in tissue applications [63]. Research in these matrices is crucial for understanding drug distribution, pharmacodynamics, and disease mechanisms in compartments beyond blood and plasma.
Within the context of partial validation and method modification, analyzing rare matrices requires strategic approaches to demonstrate analytical method reliability despite practical constraints. As noted by the Global Bioanalytical Consortium (GBC), partial validation serves to demonstrate assay reliability following modifications to existing fully validated methods, with the extent of validation determined by the nature of the modification [1]. This framework is particularly relevant when adapting methods from common matrices like plasma or serum to rare matrices such as tissue homogenates or CSF, where full validation may not be feasible or necessary.
Methodological Considerations for Rare Matrices
Matrix-Specific Challenges and Solutions
Tissue Analysis: Tissue matrices introduce complexities including cellular heterogeneity, structural components, and variable drug distribution patterns. The 2022 WRIB White Paper highlights advances in cytometry for tissue analysis, enabling single-cell analysis within complex tissue architectures [63]. Effective tissue processing requires homogenization techniques that maintain analyte stability while achieving representative sampling. For endogenous analytes, the White Paper emphasizes the need for specialized strategies to distinguish baseline levels from drug-induced changes [63].
Cerebrospinal Fluid (CSF): CSF presents challenges of limited volume availability and low analyte concentrations due to the protective nature of the blood-brain barrier. However, its proximity to the central nervous system makes it invaluable for neurological drug development. Metabolomic studies on CSF, such as those investigating Multiple Sclerosis, demonstrate the utility of combining multiple analytical platforms like proton Nuclear Magnetic Resonance (1H-NMR) and Gas Chromatography-Mass Spectrometry (GC-MS) to overcome the sensitivity limitations of individual techniques [64].
Other Rare Matrices: This category includes lacrimal fluid, synovial fluid, fecal matter, and cellular extracts. The GBC recommendations note that for rare matrices, partial validation can be limited to a practical extent given the difficulty in obtaining control materials [1]. In such cases, the use of surrogate matrix quality controls compared to real matrices may be scientifically justified when authentic matrix is unavailable in sufficient quantities.
Analytical Methodologies and Platform Selection
The choice of analytical platform depends on the matrix characteristics, analyte properties, and required sensitivity. The following experimental protocols represent common approaches for rare matrix analysis:
Ligand-Binding Assays (LBA) in Rare Matrices: LBAs are particularly valuable for rare matrices due to their sensitivity and specificity. According to recent issues in bioanalysis, LBAs require special consideration when applied to rare matrices due to potential matrix effects [63]. The protocol involves: (1) careful selection and characterization of critical reagents (antibodies, labels); (2) evaluation of matrix effects using individual and pooled matrix lots; (3) determination of minimum required dilution to minimize matrix interference; (4) assessment of selectivity in the presence of related molecules; and (5) stability evaluation under conditions appropriate for the study. For rare matrices with limited availability, the use of surrogate matrices may be necessary, with bridging experiments to demonstrate comparability.
Chromatographic Methods with Mass Spectrometry: Liquid chromatography coupled with mass spectrometry (LC-MS/MS) provides high specificity and multiplexing capability. The protocol includes: (1) optimized sample extraction to concentrate analytes and remove interfering components; (2) chromatographic separation to resolve analytes from matrix isobars; (3) mass spectrometric detection with multiple reaction monitoring for specificity; and (4) use of stable isotope-labeled internal standards to compensate for matrix effects and recovery variations. For tissue analysis, additional steps such as tissue homogenization and digestion are incorporated before extraction.
Data Fusion from Multiple Platforms: For comprehensive characterization of rare matrices, data fusion approaches integrate information from multiple analytical platforms. A metabolomic study on CSF for Multiple Sclerosis progression demonstrated a novel framework involving: (1) significant information extraction per data source using Support Vector Machine Recursive Feature Elimination; (2) optimized kernel matrix merging by linear combination; (3) analysis of merged datasets with Kernel Partial Least Square Discriminant Analysis; and (4) visualization of variable importance in kernel space [64]. This approach achieved 100% prediction accuracy on an independent test set, outperforming individual platform analysis.
Table 1: Comparison of Analytical Platforms for Rare Matrices
| Platform | Recommended Applications | Sensitivity Range | Sample Volume Requirements | Key Advantages | Major Limitations |
|---|---|---|---|---|---|
| Ligand-Binding Assays (LBA) | Macromolecules, biomarkers, immunogenicity | pg/mL - ng/mL | 25-100 µL | High sensitivity, high throughput | Matrix interference, reagent dependency |
| LC-MS/MS | Small molecules, metabolites | ng/mL - µg/mL | 50-200 µL | High specificity, multiplexing capability | Extensive sample preparation |
| Cytometry (Flow/Tissue) | Cellular analysis, cell-based assays | Single-cell level | Variable (cell count dependent) | Single-cell resolution, multiparameter | Specialized instrumentation required |
| NMR Spectroscopy | Metabolomics, structural analysis | µM-mM range | 200-500 µL | Non-destructive, quantitative | Lower sensitivity compared to MS |
Partial Validation Framework for Modified Methods
Principles of Partial Validation
When analytical methods are transferred or modified for application to rare matrices, a partial validation approach is scientifically justified and resource-efficient. The Global Bioanalytical Consortium defines partial validation as "the demonstration of assay reliability following a modification of an existing bioanalytical method that has previously been fully validated" [1]. The extent of partial validation should be determined using a risk-based approach that considers the potential impacts of the modifications.
For method transfers involving rare matrices, the GBC recommends different levels of validation based on the transfer circumstances. For internal transfers between laboratories sharing common operating systems, a reduced validation may be sufficient, while external transfers typically require more comprehensive assessment [1]. The GBC specifically notes that for rare matrices, practical considerations may limit the extent of validation possible, and scientific justification should guide the approach.
Experimental Design for Partial Validation
The parameters evaluated during partial validation should reflect the specific modifications made to the method and their potential impact on performance. Key elements to consider include:
Accuracy and Precision: Assessment using quality control samples prepared in the rare matrix at low, medium, and high concentrations. For matrices with limited availability, a reduced number of replicates or concentrations may be scientifically justified.
Selectivity and Specificity: Demonstration that the method can unequivocally quantify the analyte in the presence of components that may be expected to be present in the rare matrix, such as endogenous compounds in tissue homogenates or high protein levels in CSF.
Matrix Effects: Evaluation of ionization suppression/enhancement for LC-MS methods or non-specific binding for LBA methods. Due to limited availability of individual matrix lots for rare matrices, the number of lots tested may be reduced with scientific justification.
Stability: Assessment of analyte stability under conditions consistent with sample collection, storage, and processing. The GBC notes that long-term stability evaluation may not be required during method transfer if sufficient stability has already been established in the same matrix and storage environment [1].
Table 2: Partial Validation Requirements for Method Modifications
| Type of Modification | Recommended Validation Elements | Rare Matrix Considerations |
|---|---|---|
| Change in matrix (e.g., plasma to tissue) | Selectivity, matrix effects, accuracy/precision, stability | Use of surrogate matrix may be necessary; reduced number of matrix lots |
| Change in sample processing | Accuracy/precision, extraction recovery, stability | Limited matrix may reduce replication; focus on critical processing steps |
| Transfer to another laboratory | Full accuracy/precision, possibly stability | May qualify as internal transfer if shared systems; otherwise external requirements |
| Change in analytical range | Accuracy/precision at new limits, dilution integrity | Focus on clinically relevant range; may use spiked samples instead of authentic |
| Update to critical reagents | Accuracy/precision, selectivity, calibration model | Parallel testing of old and new reagents if possible; may use retained samples |
Quantitative Data Analysis in Complex Matrices
Data Processing and Normalization Strategies
Quantitative data from rare matrices often requires specialized processing to account for matrix-specific effects. The Bray-Curtis similarity coefficient provides one approach for comparing multivariate data patterns, defined as:
$$S{jk} = 100 \left[ 1 - \frac{\sum{i=1}^{p} | y{ij} - y{ik} | }{\sum{i=1}^{p} ( y{ij} + y{ik} ) } \right] = 100 \frac{\sum{i=1}^{p} 2 \min (y{ij}, y{ik} ) }{\sum{i=1}^{p} ( y{ij} + y_{ik} ) }$$
where $y_{ij}$ represents the abundance for the ith species in the jth sample [65]. This coefficient is particularly useful for ecological community data but can be adapted for omics datasets from rare matrices.
For data fusion from multiple platforms, kernel-based methods transform data to a high-dimensional feature space using kernel functions, making implicit relationships explicit and easier to detect [64]. The kernel fusion approach falls outside the classical low-, mid-, and high-level fusion categories and has demonstrated superior performance for non-linearly separable datasets.
Statistical Analysis and Interpretation
Statistical analysis of data from rare matrices must account for limited sample sizes, potential outliers, and heterogeneous variance. Non-parametric methods are often preferred due to smaller sample sizes and potential deviation from normality. When analyzing multiple variables, correction for multiple comparisons is essential to control false discovery rates.
For classification models using rare matrix data, methods such as Kernel Partial Least Square Discriminant Analysis (K-PLS-DA) provide robust approaches for handling non-linear relationships. The variable importance in projection (VIP) scores help identify which analytes contribute most to class separation, aiding biological interpretation [64].
Visualization of Experimental Workflows
Analytical Method Development Workflow
Diagram 1: Method development workflow for rare matrices
Data Fusion Process for Multi-Platform Analysis
Diagram 2: Data fusion process for multi-platform analysis
Research Reagent Solutions for Rare Matrix Analysis
Table 3: Essential Research Reagents for Rare Matrix Analysis
| Reagent Category | Specific Examples | Function in Analysis | Quality Considerations |
|---|---|---|---|
| Binding Reagents | Specific antibodies, aptamers, receptors | Molecular recognition and capture | Affinity, specificity, lot-to-lot consistency |
| Detection Reagents | Enzyme conjugates, fluorescent probes, mass tags | Signal generation for quantification | Sensitivity, stability, minimal non-specific binding |
| Matrix Modifiers | Surfactants, blocking agents, protease inhibitors | Reduction of non-specific interactions | Compatibility with detection system, effectiveness |
| Calibrators & Controls | Authentic standards, isotope-labeled analogs, QC materials | Quantification and method monitoring | Purity, stability, commutability with study samples |
| Sample Processing Reagents | Extraction solvents, digestion enzymes, purification resins | Analyte isolation and cleanup | Efficiency, reproducibility, minimal interference |
The analysis of tissue, CSF, and other rare matrices requires specialized strategies that balance scientific rigor with practical constraints. The partial validation framework provides a scientifically sound approach for adapting existing methods to these challenging matrices, with the extent of validation determined by the nature of the modifications and matrix-specific considerations. As analytical technologies continue to advance, including the development of more sensitive detection platforms and sophisticated data analysis methods like kernel-based data fusion, our ability to extract meaningful information from these precious samples will continue to improve. By implementing the strategies outlined in this guide, researchers can navigate the complexities of rare matrix analysis while generating high-quality data to support drug development decisions.
Documenting Deviations and Justifying the Scope of Validation
In pharmaceutical research and development, the validation of analytical methods is a cornerstone for ensuring the reliability, accuracy, and reproducibility of data. Full validation is typically performed for new methods. However, in the context of method transfer or minor modifications, a partial validation approach is often scientifically justified and resource-efficient. This guide provides a structured framework for documenting deviations from full validation protocols and objectively justifying the reduced scope. The core principle is that the extent of validation should be commensurate with the nature and significance of the change introduced to the existing method. This involves a risk-based assessment to identify which validation parameters are critical to demonstrate the method's continued performance for its intended use. The subsequent sections will compare validation approaches, detail experimental protocols for partial validation, and provide visual tools to guide scientists in this process.
Comparative Analysis of Validation Scopes: Full vs. Partial
The decision to perform a full or partial validation is contingent on the specific circumstances of the method's application. A full validation is comprehensive, while partial validation targets specific parameters potentially impacted by a change. The following table summarizes the typical scope of each approach for key validation parameters, providing a clear comparison for stakeholders.
Table 1: Scope of Validation Parameters - Full vs. Partial Validation
| Validation Parameter | Full Validation Scope | Partial Validation Scope (Example: HPLC Method Transfer) | Performance Comparison Data (Hypothetical) |
|---|---|---|---|
| Accuracy | Comprehensive assessment across the specified range, e.g., 3 concentration levels, 3 replicates each. | Verification at a single, critical concentration level (e.g., 100% of target) in the new laboratory. | Recovery Rate: Lab A (Orig.): 99.5%; Lab B (New): 99.8%. Deviation: +0.3%, within pre-defined ±2.0% acceptance criteria. |
| Precision | Evaluation of repeatability (intra-day) and intermediate precision (inter-day, inter-analyst). | Assessment of repeatability only at the new site, leveraging existing intermediate precision data from the method originator. | %RSD (Repeatability): Lab A: 0.8%; Lab B: 1.0%. Deviation: +0.2%, within pre-defined ≤1.5% acceptance criteria. |
| Specificity | Demonstrated for all known and potential impurities, degradation products, and matrix components. | Confirmation that the method remains specific in the new environment, often challenged with a placebo or blank matrix. | Resolution from critical pair: Lab A: 2.5; Lab B: 2.3. Justification: Resolution >2.0 confirms maintained specificity. |
| Linearity & Range | Established with a minimum of 5 concentration levels across the entire analytical range. | Verification of linearity using 3 concentration levels (low, medium, high) within the approved range. | Correlation Coefficient (r²): Lab A: 0.9995; Lab B: 0.9992. Deviation: -0.0003, within pre-defined ≥0.999 acceptance criteria. |
| Robustness | Systematically evaluated by deliberate variations in method parameters (e.g., pH, temperature, flow rate). | Not typically repeated unless a specific, uncontrolled variable at the new site is identified as a potential risk. | N/A - Parameter not re-tested. Justified by the controlled environment of the receiving laboratory. |
Experimental Protocol for a Partial Validation Study
This section details a generalized, yet robust, experimental methodology for conducting a partial validation, using the transfer of a High-Performance Liquid Chromatography (HPLC) assay method as a model scenario.
Protocol: Partial Validation for HPLC Method Transfer
1. Objective: To verify the performance of an established HPLC assay method in a receiving laboratory (Lab B) following transfer from the originating laboratory (Lab A), thereby justifying a partial validation scope.
2. Scope: This protocol is applicable for method transfers where the analytical procedure and instrumentation are equivalent. It covers the experimental verification of Accuracy, Precision, and Specificity.
3. Materials and Reagents:
- Reference Standard: Certified reference material of the active pharmaceutical ingredient (API) with known purity.
- Test Sample: A homogeneous batch of the drug product.
- Placebo: All excipients of the drug product formulation, excluding the API.
- Mobile Phase: Prepared according to the established method procedure in both laboratories.
- HPLC Systems: Qualified systems in both Lab A and Lab B with equivalent specifications (e.g., C18 columns from the same supplier and lot, if possible).
4. Experimental Procedure:
- 4.1. System Suitability: Both labs perform system suitability tests as per the method. Criteria typically include plate count, tailing factor, and %RSD of replicate injections.
- 4.2. Specificity: Both labs inject the placebo preparation. The chromatogram must demonstrate no interference at the retention time of the API.
- 4.3. Accuracy (Recovery): A test sample is spiked with a known quantity of reference standard at the 100% target concentration level (n=6). The accuracy is calculated as the percentage recovery of the known added amount.
- 4.4. Precision (Repeatability): The six samples prepared for accuracy are analyzed sequentially. The precision is reported as the % Relative Standard Deviation (%RSD) of the six results.
5. Acceptance Criteria:
- Specificity: No peak interference from placebo at the API retention time.
- Accuracy: Mean recovery between 98.0% and 102.0%.
- Precision: %RSD of not more than 2.0%.
6. Documentation of Deviations: Any deviation from this experimental protocol, including any out-of-specification (OOS) result, must be documented in a deviation report. The report should include the nature of the deviation, the root cause investigation, its impact on the study, and the final justification for the validated state of the method [66].
Visual Workflow for Scope Justification
The decision-making process for determining the appropriate validation scope can be complex. The following diagram illustrates a logical workflow that guides a scientist from an initial method change through to the final documentation, incorporating risk assessment and experimental design.
The Scientist's Toolkit: Key Research Reagent Solutions
The integrity of any validation study is dependent on the quality of the materials used. Below is a list of essential research reagents and materials critical for executing a reliable partial validation study, particularly in chromatographic analysis.
Table 2: Essential Research Reagents and Materials for Analytical Validation
| Item | Function & Importance in Validation |
|---|---|
| Certified Reference Standard | Serves as the primary benchmark for quantifying the analyte. Its certified purity and stability are fundamental for establishing method accuracy and linearity. |
| Chromatography Column | The stationary phase is critical for separation. Using a column with equivalent specifications (e.g., L1, C18, same particle size) is vital for reproducing specificity and robustness. |
| System Suitability Mixture | A test preparation used to verify that the chromatographic system is performing adequately before the analysis. It ensures the integrity of the entire experimental run. |
| Placebo/Blank Matrix | Used in specificity testing to confirm that the excipients or matrix components do not interfere with the detection and quantification of the analyte. |
| Mobile Phase Components | High-purity solvents and buffers are essential for achieving baseline stability, reproducible retention times, and preventing spurious peaks that could affect quantification. |
A scientifically sound approach to partial validation, supported by objective performance comparisons and rigorous documentation, is essential in modern drug development. By focusing resources on the validation parameters most likely to be affected by a change, organizations can maintain high standards of quality and compliance while improving efficiency. The frameworks, protocols, and visual guides provided in this document offer researchers and scientists a practical toolkit for successfully documenting deviations and justifying the scope of validation, thereby strengthening the overall integrity of analytical data submitted for regulatory review.
Partial Validation in Context: Comparison with Transfer, Verification, and Cross-Validation
In pharmaceutical development, an analytical method's journey does not end with its initial validation. The method lifecycle involves continuous refinement, technology transfer between facilities, and necessary adaptations to meet evolving project needs. Within this framework, partial validation and method transfer emerge as two critical but distinct processes. While both activities provide documented evidence of method reliability, they serve fundamentally different purposes within the quality system [1] [3].
Partial validation demonstrates reliability following a modification to an existing, fully-validated method [1]. It represents a targeted re-validation effort triggered by specific changes. In contrast, method transfer is a comprehensive qualification process that enables a receiving laboratory to implement an existing analytical procedure with the same level of confidence as the originating laboratory [67] [68]. Understanding their unique goals, triggers, and documentation requirements is essential for researchers and drug development professionals maintaining regulatory compliance while advancing analytical methods.
Core Concept Comparison
The table below summarizes the fundamental distinctions between these two processes.
| Feature | Partial Validation | Method Transfer |
|---|---|---|
| Primary Goal | To demonstrate reliability after a method modification [1] | To qualify a new laboratory to use the existing method reliably [67] [68] |
| Defining Trigger | A change to a validated method (e.g., equipment, sample prep) [1] [3] | Movement of a method to a different laboratory or site [67] |
| Scope of Work | Targeted, risk-based assessment of parameters affected by the change [1] | Broader assessment of the laboratory's ability to execute the entire method correctly [1] [67] |
| Documentation Focus | Protocol and report justifying the scope of re-validation and demonstrating performance post-change [1] | Comprehensive protocol and report proving equivalence between originating and receiving labs [67] [69] |
| Relationship to Method | Part of the method's life cycle within a single lab [1] | Part of the method's geographic or organizational deployment [67] |
Detailed Breakdown of Partial Validation
Triggers and Scope
Partial validation is initiated by specific, predefined changes to an already-validated method. The nature of the modification dictates the extent of validation required, ranging from a simple precision and accuracy experiment to a nearly full validation [1] [3].
Common triggers and the recommended validation scope include:
- Change in Equipment: A significant change in instrumentation or key components (e.g., a different detector type) requires assessing accuracy, precision, and specificity. Minor changes like a different instrument from the same manufacturer may need only a system suitability test [1].
- Change in Sample Processing: A complete paradigm shift in sample preparation, such as moving from protein precipitation to solid-phase extraction, warrants a substantial partial validation. Minor changes (e.g., elution volume adjustment) require less extensive checks [1].
- Change in Analytical Range: Extending or narrowing the validated range requires re-establishing linearity, accuracy, and precision at the new limit(s) [1].
- Change in Matrix: For bioanalytical methods, a change in biological matrix (e.g., from plasma to urine) is typically considered a new method. However, changes like a different anti-coagulant counter-ion may not require re-validation [1].
Experimental Design and Acceptance Criteria
The experimental design for partial validation follows a risk-based approach, focusing on parameters potentially impacted by the change.
Typical Workflow: The diagram below outlines the logical decision process for planning and executing a partial validation.
Example - Change in HPLC Mobile Phase:
- Experimental Protocol: A standard operating procedure (SOP) would dictate preparing a minimum of six calibration standards and quality control (QC) samples at multiple levels (e.g., Low, Mid, High). These are analyzed in multiple runs (e.g., n=6) across different days to assess inter-assay precision [1] [56].
- Key Parameters & Acceptance Criteria:
- Accuracy: Mean measured concentration of QCs should be within ±15% of the nominal value (±20% at LLOQ) [56].
- Precision: % Relative Standard Deviation (%RSD) of QC replicates should be ≤15% (≤20% at LLOQ) [56].
- Specificity: Chromatograms should demonstrate no interference from the matrix at the retention time of the analyte.
- System Suitability: Parameters like resolution (R), theoretical plates (N), and peak asymmetry must meet method-specific criteria before each run [70].
Detailed Breakdown of Method Transfer
Objectives and Approaches
The primary objective of method transfer is to provide documented evidence that the Receiving Unit (RU) can perform the analytical procedure consistently and generate results equivalent to those generated by the Transferring Unit (TU) [67] [68]. This is crucial for regulatory compliance and ensuring product quality when testing is moved to a new facility, such as a contract manufacturing organization (CMO) [67].
Several standardized approaches can be used, either alone or in combination:
- Comparative Testing: This is the most common approach. Both the TU and RU analyze the same set of homogeneous samples (e.g., from one or more batches). The results are statistically compared against pre-defined acceptance criteria [67] [68] [69].
- Co-Validation: The RU actively participates in the initial method validation activities, providing inter-laboratory data that establishes method reproducibility and facilitates transfer [67] [69].
- Re-Validation or Partial Validation: The RU performs a full or partial validation of the method. This is applicable when there are significant differences in equipment or lab environment, or for highly complex methods [67] [69].
- Transfer Waiver: In specific cases where justification exists (e.g., the method is an unchanged pharmacopoeial procedure and the RU has extensive experience with it), experimental transfer can be waived. This decision must be formally documented [69].
Experimental Design and Acceptance Criteria
A successful method transfer is a protocol-driven, collaborative process.
Typical Workflow: The following diagram illustrates the key stages in a method transfer, highlighting the roles of both Transferring and Receiving Units.
Example - Comparative Testing for a Drug Product Assay:
- Experimental Protocol: The approved transfer protocol specifies that the RU and TU will each analyze the same batch of drug product. A typical design might involve two analysts in the RU each performing three replicate determinations per sample on different days, using different instrument systems and columns where possible [69]. The number of batches tested depends on the product type (e.g., one batch for a single-strength drug product) [68].
- Key Parameters & Acceptance Criteria: The table below shows common tests and their acceptance criteria for a successful transfer.
| Test | Experimental Replication | Acceptance Criteria |
|---|---|---|
| Assay | 2 Analysts x 3 test samples in triplicate [69] | Comparison of mean results between TU and RU. Difference should be < 2.0% [69]. |
| Impurities | 2 Analysts x 3 test samples in triplicate, including spiked samples [69] | Comparison of result variability. Difference should be < 25.0% for the impurity level; %RSD of replicates < 5.0% [69]. |
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents and materials are fundamental for executing the experimental protocols in both partial validation and method transfer.
| Item | Function & Importance |
|---|---|
| Reference Standards | Highly characterized substances used to calibrate instruments and prepare known samples for accuracy and precision experiments. Their purity and stability are paramount [68]. |
| System Suitability Test (SST) Mixtures | A reference preparation containing key analytes and/or impurities to verify chromatographic system performance (e.g., resolution, plate count, peak asymmetry) before sample analysis runs [70]. |
| Certified Mobile Phase Solvents & Reagents | Solvents and chemicals with documented purity and specification to ensure reproducibility of the analytical method, especially critical for sensitive techniques like LC-MS [67]. |
| Qualified Chromatography Columns | Columns with performance certificates that match the specifications in the analytical method. Variability between column lots or manufacturers is a common source of transfer failure [67]. |
| Control Matrices & Placebos | For bioanalytical methods: appropriate biological matrix (e.g., human plasma). For drug products: a placebo mixture containing all inactive ingredients. Used to prepare calibration standards and QCs to assess specificity and matrix effects [1] [68]. |
Partial validation and method transfer are complementary yet distinct pillars in the lifecycle management of analytical methods. Partial validation acts as a targeted maintenance tool, ensuring a method remains valid after specific, deliberate modifications. Method transfer serves as a deployment and qualification tool, ensuring methodological consistency and data integrity across different laboratories and geographies.
For researchers and drug development professionals, a clear understanding of their unique triggers, scopes, and documentation requirements is not merely a regulatory formality. It is a strategic imperative that ensures the generation of reliable, high-quality data, accelerates technology transfer to manufacturing partners, and ultimately safeguards the quality, safety, and efficacy of pharmaceutical products for patients.
In the rigorous world of analytical science, particularly in pharmaceutical development and bioanalysis, the concepts of partial validation and cross-validation represent critical, interconnected phases of the method lifecycle. Partial validation is the documented process of re-establishing method performance characteristics when a previously validated method undergoes modifications, ensuring it remains suitable for its intended use despite changes in scope, equipment, or analytical location [3]. This process often naturally culminates in a cross-validation exercise, which is a direct comparison of two or more methods to determine their equivalence when they are used to generate data within the same study or across different studies [3]. Framed within a broader thesis on modified analytical methods, this guide objectively compares the performance of these validation strategies, providing the experimental protocols and data interpretation frameworks essential for researchers, scientists, and drug development professionals tasked with ensuring data integrity and regulatory compliance.
Core Concepts and Definitions
Partial Validation: A Focused Re-assessment
Partial validation is performed on a method that has undergone minor, but significant, changes. It is a subset of a full validation, where the specific tests conducted are selected based on the nature of the changes made to the method. The goal is not to re-establish every performance characteristic, but to confirm that the modifications have not adversely impacted the method's reliability [3]. Examples of changes that trigger a partial validation include:
- Changes in equipment or instrumentation.
- Modifications to solution composition (e.g., buffer pH, mobile phase).
- Adjustments to the quantitation range.
- Alterations in sample preparation procedures.
- Transfer of the method to a new laboratory (often handled as a method transfer) [3].
Cross-Validation: Establishing Equivalence Between Methods
Cross-validation is a comparison of validation parameters when two or more bioanalytical methods are used to generate data within the same study or across different studies [3]. Its primary purpose is to establish that different methods (or the same method used in different laboratories) produce equivalent results, ensuring data consistency. Common scenarios include:
- Comparing a new method to a legacy or reference method.
- Verifying method performance after a partial validation.
- Assessing data equivalency when multiple laboratories are involved in a single study.
- Demonstrating parity between a higher-throughput method and an established, lower-throughput one.
Experimental Protocols for Method Comparison
The cornerstone of both partial and cross-validation is a robust comparison of methods experiment. The following protocol, adapted from established clinical laboratory practices [71], provides a detailed methodology for generating the data needed to make an objective decision.
Protocol: The Comparison of Methods Experiment
Purpose: To estimate the systematic error (inaccuracy or bias) between a test method and a comparative method using real patient specimens.
Experimental Design Factors:
- Comparative Method: The method used for comparison should be carefully selected. An ideal choice is a reference method with well-documented correctness. If using a routine method, any large discrepancies must be interpreted with caution, as it may not be clear which method is inaccurate [71].
- Number of Patient Specimens: A minimum of 40 different patient specimens is recommended. The quality of specimens is more important than sheer quantity; they should be selected to cover the entire working range of the method and represent the spectrum of diseases expected in routine application. Using 100-200 specimens is advised to thoroughly assess method specificity [71].
- Replication and Timeframe: Specimens are typically analyzed singly by both the test and comparative methods. However, performing duplicate measurements on different sample cups and in different analytical runs is beneficial to identify errors. The experiment should be conducted over a minimum of 5 days to capture inter-day performance variability, ideally over a longer period (e.g., 20 days) with 2-5 specimens per day [71].
- Specimen Stability: Specimens analyzed by both methods should be processed within two hours of each other to prevent degradation from causing observed differences. Stability can be managed through preservatives, serum/plasma separation, or freezing [71].
Procedure:
- Select and prepare patient specimens covering the analytical measurement range.
- Analyze each specimen using both the test method and the comparative method within a short time window, following the defined timeframe and replication scheme.
- Record all results meticulously.
Data Analysis:
- Graphical Inspection: The data should be graphed at the time of collection to identify discrepant results for immediate re-analysis.
- For methods expected to show 1:1 agreement, use a difference plot (test result minus comparative result on the y-axis versus the comparative result on the x-axis).
- For methods not expected to show 1:1 agreement (e.g., different enzyme assays), use a comparison plot (test result on the y-axis versus comparative result on the x-axis) [71].
- Statistical Calculations:
- For a wide analytical range: Use linear regression statistics (slope, y-intercept, standard deviation about the regression line (s{y/x})) to estimate the systematic error ((SE)) at critical medical decision concentrations ((Xc)): (Yc = a + b \cdot Xc) (SE = Yc - Xc)
- For a narrow analytical range: Calculate the average difference (bias) between the methods using a paired t-test. The correlation coefficient ((r)) is also calculated, mainly to verify that the data range is wide enough for reliable regression analysis (an (r \geq 0.99) is desirable) [71].
Protocol: K-Fold Cross-Validation for Model Stability
In computational and bioinformatic contexts, cross-validation is a resampling technique used to assess how a statistical model will generalize to an independent dataset, guarding against overfitting [72] [73]. K-Fold Cross-Validation is the most widely used approach.
Purpose: To provide a robust estimate of a predictive model's performance and stability by partitioning the available data into multiple training and validation subsets.
Procedure:
- Partition: Randomly split the entire dataset into (k) equal-sized subsets (folds).
- Iterate: For each of the (k) folds:
- Train: Use the remaining (k-1) folds as the training data to build the model.
- Validate: Use the held-out (k^{th}) fold as the validation data to test the model and compute a performance metric (e.g., accuracy, mean squared error).
- Average: Calculate the average and standard deviation of the (k) performance metrics to summarize the model's predictive capability [72] [74] [73].
A common choice is (k=10). A special case is Leave-One-Out Cross-Validation (LOOCV), where (k) equals the number of data points, providing a comprehensive but computationally expensive evaluation [73].
The workflow below illustrates the k-fold cross-validation process, showing how data is partitioned and how models are iteratively trained and validated.
Performance Data and Comparison
The following tables summarize the key characteristics, performance indicators, and strategic applications of partial and cross-validation, enabling a direct comparison.
Table 1: Comparison of Validation Method Characteristics and Data Output
| Characteristic | Partial Validation | Cross-Validation (Method Comparison) | K-Fold Cross-Validation (Model Evaluation) |
|---|---|---|---|
| Primary Objective | Confirm method performance after a minor change [3] | Establish equivalence between two methods [3] | Estimate model generalizability and avoid overfitting [72] |
| Typical Data Input | ~40 patient specimens analyzed over multiple days [71] | ~40 patient specimens analyzed by two methods [71] | Entire dataset partitioned into k folds [73] |
| Key Performance Metrics | Accuracy, precision, specificity parameters relevant to the change [3] | Slope, y-intercept, standard error of the estimate ((s_{y/x})), bias [71] | Mean accuracy/precision, standard deviation across k folds [74] |
| Quantitative Output | Documentation showing performance meets pre-defined acceptance criteria | Regression equation (Y = a + bX) and SE at decision levels [71] | Average score and standard deviation (e.g., 0.98 ± 0.02) [74] |
| Experimental Scope | Targeted, limited set of experiments based on the change | A full method comparison for a defined analytical range | A comprehensive model evaluation using all available data |
Table 2: Strategic Application and Regulatory Context
| Aspect | Partial Validation | Cross-Validation |
|---|---|---|
| Regulatory Driver | ICH Q2(R1), FDA guidance on post-approval changes [3] [75] | ICH Q2(R1), bioanalytical method validation guidelines [3] |
| Triggering Event | Minor method changes (equipment, reagents, range), method transfer [3] | Use of multiple methods in a study, method transfer, establishing parity with a reference method [3] |
| Role in Method Lifecycle | Lifecycle management (ICH Q12); ensures continued fitness-for-use after modification [75] | Supports method equivalence during development, transfer, or when comparing to a gold standard [3] |
| Decision Outcome | Method is (or is not) suitable for continued use after the change. | Two methods are (or are not) equivalent for their intended use. |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and solutions required for executing the wet-lab experimental protocols described in this guide.
Table 3: Key Research Reagent Solutions for Method Validation Experiments
| Reagent/Material | Function in Experiment | Critical Specifications |
|---|---|---|
| Certified Reference Standards | Provides the known quantity of analyte for establishing accuracy and constructing calibration curves. | Purity, concentration, and stability; traceability to a primary reference. |
| Quality Control (QC) Materials | Monitors the stability and performance of the analytical method during the validation process. | Should mimic the patient sample matrix and have assigned values at low, medium, and high concentrations. |
| Patient Specimens | Serves as the real-world sample for the comparison of methods experiment. | Must cover the entire assay range and represent the expected pathological conditions [71]. |
| Matrix-Based Calibrators | Used to construct the calibration curve in the specific sample matrix (e.g., human plasma). | Ensures accurate quantitation by correcting for matrix effects. |
| Specific Interference Stocks | Evaluates the method's selectivity by testing for interference from common substances (e.g., lipids, hemoglobin, bilirubin). | Prepared at high, clinically relevant concentrations. |
The journey from partial validation to cross-validation is a logical and necessary progression in the lifecycle of a robust analytical method. Partial validation acts as a targeted, cost-effective check-point after method modifications, while cross-validation provides the definitive, data-driven evidence required to claim equivalence between methods. In an era of increasing technological complexity, global collaboration, and regulatory scrutiny—driven by trends such as AI-enhanced analytics and Quality-by-Design (QbD) [75]—the principles outlined in this guide provide a solid foundation for ensuring that analytical data, whether generated by a modified method in-house or a different method across continents, is reliable, comparable, and ultimately, fit for its purpose in drug development.
Leveraging Partial Validation to Streamline Method Transfer Between Laboratories
In the pharmaceutical industry, the transfer of analytical methods between laboratories is a critical, yet often resource-intensive, process essential for ensuring consistent drug quality across different manufacturing and testing sites. Traditional approaches frequently involve comprehensive comparative testing, which can be time-consuming and costly. Within this context, partial validation emerges as a targeted, science- and risk-based strategy for streamlining method transfer. This approach is not about reducing standards but about focusing efforts where they are most needed. Framed within broader analytical methods research, leveraging partial validation allows for a more efficient transfer process without compromising the reliability or regulatory compliance of the analytical procedure. It is a pragmatic solution for confirming that a method, already validated in a Transferring Laboratory (TU), performs as intended in a Receiving Laboratory (RU) when specific, justifiable conditions are met [67] [69].
Understanding Method Transfer Strategies
The Spectrum of Transfer Approaches
Analytical method transfer is a documented process that qualifies a Receiving Laboratory to use an analytical test procedure that originated in a Transferring Laboratory [69]. Regulatory guidelines from agencies like the FDA, EMA, and WHO, as well as USP General Chapter <1224>, recognize several formal approaches [67]. The choice of strategy depends on a risk assessment that considers the method's complexity, the extent of changes in the new environment, and regulatory requirements [67] [76].
- Comparative Testing: This is the most common approach for critical methods. Both the sending and receiving laboratories test the same homogeneous samples, and their results are compared against pre-defined acceptance criteria to demonstrate equivalence [67] [69].
- Co-validation: The receiving laboratory participates in the original method validation study. This approach establishes inter-laboratory reproducibility (ruggedness) as part of the initial validation and is particularly useful for new or complex methods [67] [69].
- Transfer Waiver: In specific, justified cases, no experimental transfer work is required. This may apply when the method is an unchanged compendial procedure, the receiving laboratory has extensive experience with a very similar method, or key personnel move between labs [67] [69].
- Revalidation or Partial Validation: This strategy involves re-evaluating specific validation parameters that are most likely to be affected by the transfer, rather than repeating the entire validation [67] [69].
Comparative Analysis of Transfer Approaches
The table below summarizes the key characteristics, typical use cases, and relative resource demands of each transfer strategy.
Table: Comparison of Analytical Method Transfer Strategies
| Transfer Approach | Key Characteristics | Ideal Use Case | Resource Intensity |
|---|---|---|---|
| Comparative Testing [67] [69] | Both labs test identical samples; results compared statistically. | Critical methods; first-time transfers to a new lab. | High (extensive testing and data comparison) |
| Co-validation [67] [69] | Receiving lab participates in method validation. | New or highly complex methods during initial validation. | High (integrated into validation lifecycle) |
| Revalidation/ Partial Validation [67] [69] | Repeats only the validation parameters affected by the transfer. | Changes in equipment, site, or environment that impact specific method aspects. | Medium (focused, efficient) |
| Transfer Waiver [67] [69] | No experimental work; relies on scientific justification. | Unchanged compendial methods or transfer of experienced personnel. | Low (documentation-focused) |
Partial Validation: A Targeted Framework for Efficient Transfer
Conceptual Foundation and Applicability
Partial validation, as defined in USP <1224>, is a strategic approach where only those validation parameters described in guidelines like ICH Q2 that are anticipated to be affected by the transfer are evaluated [69]. This makes it a powerful tool for streamlining the transfer process. It is not a shortcut, but a scientifically rigorous practice that directs resources to potential vulnerabilities introduced by the change in laboratory environment. This approach is fundamentally aligned with modern quality-by-design and risk-management principles.
Partial validation is particularly well-suited for several common transfer scenarios, including but not limited to:
- Transfer between laboratories with equivalent but not identical instrumentation.
- Changes in analysts or site-specific environmental conditions.
- Transfer of methods for stable products with well-understood method performance.
- When a method-transfer kit (MTK) containing representative and stability-challenged materials is used, providing a consistent benchmark for comparison [77].
Decision Workflow for Implementing Partial Validation
The following diagram illustrates the logical decision process for determining if a partial validation approach is suitable for a method transfer.
Experimental Protocol for Partial Validation
Core Methodology and Parameter Selection
A successful partial validation transfer begins with a pre-approved protocol that clearly defines the scope, experimental design, and acceptance criteria [67] [76]. The protocol is drafted by the Transferring Laboratory and must be approved by the Quality Assurance unit and all team members before execution begins [76].
The core of the methodology involves a risk assessment to select which validation parameters to test. For instance:
- Precision and Accuracy: Often critical for assay methods. A typical experimental design may involve two analysts in the Receiving Laboratory each analyzing three batches of the product in triplicate, using different instrument and column setups [69]. The results are compared to those from the TU, with acceptance criteria such as a difference in means of less than 2.0% for assay [69].
- Specificity and Robustness: Crucial for stability-indicating methods, especially impurity tests. The Receiving Laboratory may test samples that have been stressed (e.g., forced degradation) or spiked with known impurities to demonstrate the method's specificity in the new environment [67] [77]. Robustness can be inferred if the method passes system suitability tests under the RU's minor variations in conditions.
- Detection Limit (LOD) / Quantitation Limit (LOQ): Particularly relevant for impurity methods. The RU may demonstrate the ability to precisely (e.g., %RSD < 5.0%) and accurately quantify impurities at the specification level or LOQ [69].
Key Research Reagent Solutions
The use of standardized materials is vital for a consistent and successful transfer. The concept of a Method-Transfer Kit (MTK) is an innovative solution designed for this purpose [77]. The table below details essential materials and their functions in a partial validation study.
Table: Essential Research Reagent Solutions for Partial Validation Transfer
| Material / Solution | Critical Function & Justification |
|---|---|
| Method-Transfer Kit (MTK) [77] | A centrally-managed kit containing representative batch(es) of material. Ensures all labs test the exact same samples, eliminating batch-to-batch variability and focusing the assessment on method performance. |
| Stability-Challenged Samples [77] | Samples with intentionally induced degradation (e.g., via heat, light, hydrolysis). Serves as a tangible positive control for specificity in the Receiving Laboratory. |
| Impurity-Spiked Samples [69] [77] | Placebo or drug product samples spiked with known impurities at specification levels. Demonstrates accuracy and precision of the impurity method in the RU for low-level analytes. |
| System Suitability Reference [67] | A standardized solution used to verify that the chromatographic system (or other instrument) is performing adequately before and during analysis. Critical for ensuring robustness. |
| Qualified Reference Standards [76] | Well-characterized standards of the analyte and key impurities. Essential for generating accurate and precise quantitative data in both laboratories. |
Data Presentation: Comparing Transfer Outcomes
Quantitative Results from Model Transfers
The following table summarizes hypothetical but representative experimental data from two different method transfers, one using a full comparative approach and the other using a targeted partial validation. The data illustrates how partial validation can achieve the same goal with greater efficiency.
Table: Experimental Data Comparison: Full vs. Partial Validation Transfer
| Validation Parameter | TU Results | Full Transfer: RU Results | Partial Validation: RU Results | Acceptance Criteria |
|---|---|---|---|---|
| Assay (Potency) | ||||
| Mean Result (% of claim) | 99.8% | 100.2% | 100.1% | 98.0% - 102.0% |
| Difference from TU Mean | - | +0.4% | +0.3% | ≤ 2.0% [69] |
| Intermediate Precision (%RSD, n=6) | 0.5% | 0.7% | 0.6% | ≤ 2.0% |
| Related Substances | ||||
| Mean Total Impurities | 0.45% | 0.48% | 0.46% | ≤ 1.0% |
| Difference from TU Mean | - | +0.03% | +0.01% | ≤ 0.1% or 25% [69] |
| Precision at LOQ (%RSD) | 4.2% | 4.8% | 4.5% | ≤ 5.0% [69] |
| Specificity | Verified | Verified | Waived | No interference |
| Linearity & Range | Verified (r²=0.999) | Verified (r²=0.999) | Waived | r² ≥ 0.998 |
| Parameters Tested | 8 | 8 | 4 | - |
| Total Analyst Days | - | 12 | 6 | - |
Interpretation of Comparative Data
The data demonstrates that for this model method, the partial validation approach was equally effective in qualifying the Receiving Laboratory as the full comparative transfer. The RU results for the tested parameters (Assay and Related Substances) were well within the pre-defined acceptance criteria and were statistically equivalent to both the TU results and the results from the full transfer. By waiving the re-testing of parameters like Specificity and Linearity—which are intrinsic to the method's design and less susceptible to change between qualified laboratories—the partial validation cut the required analyst time in half. This showcases a direct and significant efficiency gain while maintaining data integrity and regulatory compliance.
In an industry where speed to market and operational efficiency are paramount, partial validation stands out as a powerful, scientifically sound strategy for streamlining the analytical method transfer process. By moving away from a one-size-fits-all approach and adopting a risk-based, targeted validation, pharmaceutical companies can significantly reduce transfer timelines and resource expenditure. This is achieved without compromising the fundamental goal of method transfer: to ensure the Receiving Laboratory can generate reliable, high-quality data that guarantees patient safety and product efficacy. As analytical methods research evolves, the strategic use of partial validation, supported by tools like method-transfer kits, represents a mature and efficient pathway for global pharmaceutical development and manufacturing.
The management of post-approval changes and the verification of product quality have traditionally been discrete, often sequential, activities in the pharmaceutical industry. However, the evolution of International Council for Harmonisation (ICH) guidelines is driving a fundamental shift towards an integrated, proactive lifecycle approach. ICH Q12, "Technical and Regulatory Considerations for Pharmaceutical Product Lifecycle Management," provides a structured framework for managing post-approval Chemistry, Manufacturing, and Controls (CMC) changes with greater predictability and efficiency [78] [79]. Concurrently, modern paradigms like Continuous Process Verification (CPV) provide the data-driven backbone to monitor and assure product quality in real-time [80]. For researchers and scientists, the synergy between these frameworks is particularly impactful in the context of partial validation of modified analytical methods, a common requirement when implementing post-approval changes. This guide objectively compares the traditional and lifecycle-led approaches to this specific activity, providing experimental protocols and data to underscore the performance advantages of integration.
Core Concept Comparison: Traditional vs. Lifecycle-Led Approaches
The following table contrasts the fundamental characteristics of the traditional and lifecycle-led approaches to managing analytical methods and process verification.
Table 1: Comparison of Traditional and Lifecycle-Led Approaches
| Characteristic | Traditional Approach | Lifecycle-Led Approach (ICH Q12 & Continuous Verification) |
|---|---|---|
| Regulatory Paradigm | "Tell and Do" – Prior approval required for changes [78] | "Do and Tell" – Certain well-defined changes can be implemented with notification post-change [78] |
| Foundation for Changes | Primarily based on prior submission data and reactive compliance | Science- and risk-based, enabled by enhanced product and process knowledge [78] [81] |
| Analytical Procedure Management | Viewed as a static entity after initial validation; changes can be challenging [62] | Embraces Analytical Procedure Lifecycle as per ICH Q2(R2) & Q14, allowing for managed evolution and post-approval changes [62] [82] |
| Validation Strategy | Often requires full re-validation for method changes | Supports partial validation, where only the impacted performance characteristics are re-evaluated [62] |
| Quality Verification | Reliant on discrete, batch-end testing | Leverages Process Analytical Technology (PAT) and real-time data for Continuous Process Verification and Real-Time Release Testing (RTRT) [80] |
| Key Enabling Tools | Standarded validation protocols | Established Conditions (ECs), Post-Approval Change Management Protocols (PACMPs), and an effective Pharmaceutical Quality System (PQS) [78] [81] |
Experimental Protocols for Partial Validation in a Lifecycle Context
When an analytical procedure is modified under a PACMP, a full validation is often unnecessary. The following protocol outlines a science- and risk-based methodology for conducting a partial validation.
Protocol: Risk-Based Partial Validation for an Modified HPLC Method
- Objective: To demonstrate that a modified HPLC method for drug product assay (e.g., a change in column temperature or mobile phase pH) remains fit-for-purpose by evaluating only the performance characteristics potentially impacted by the change.
- Principle: A risk assessment is conducted to identify which validation parameters are susceptible to the specific modification. Experiments are then designed to target only those parameters [62] [83].
- Materials & Reagents:
- HPLC System: Qualified system with UV/VIS detector.
- Reference Standard: Drug substance of known purity.
- Test Sample: Representative drug product batch.
- Chromatographic Column: The specified column for the method.
- Mobile Phase: Prepared as per the modified method.
- Risk Assessment & Experimental Design:
- Change: Increase in column temperature from 30°C to 40°C.
- Risk Hypothesis: The change could impact specificity (peak resolution), precision (retention time reproducibility), and robustness (sensitivity to minor fluctuations).
- Parameters for Partial Validation: Based on the risk, the following are evaluated: Specificity, Precision (Repeatability), and Robustness.
- Methodology:
- Specificity: Inject separately prepared solutions of the analyte and known impurities. Demonstrate that the resolution between the analyte peak and the closest eluting impurity peak meets pre-defined acceptance criteria (e.g., Resolution > 2.0).
- Precision (Repeatability): Prepare six independent sample preparations from a homogeneous lot and analyze using the modified method. Calculate the % Relative Standard Deviation (%RSD) of the assay results. The acceptance criterion is typically %RSD ≤ 2.0% [83].
- Robustness: Deliberately introduce small, deliberate variations to the modified method (e.g., flow rate ±0.1 mL/min, temperature ±2°C). The system suitability criteria (e.g., tailing factor, theoretical plates) should be met in all variations, demonstrating the method's resilience.
Data Presentation and Comparison
The table below summarizes hypothetical experimental data from the partial validation of the modified HPLC method, comparing it against the original validation data and pre-defined acceptance criteria.
Table 2: Partial Validation Data for HPLC Assay Method Modification
| Performance Characteristic | Acceptance Criteria | Original Validation Data | Partial Validation Data (Post-Modification) | Conclusion |
|---|---|---|---|---|
| Specificity (Resolution) | > 2.0 | 2.5 | 2.3 | Pass |
| Accuracy (% Recovery) | 98.0 - 102.0% | 100.2% | Not Tested | Justified by risk assessment; change not considered impactful. |
| Precision (%RSD, n=6) | ≤ 2.0% | 0.8% | 1.1% | Pass |
| Linearity (R²) | > 0.999 | 0.9995 | Not Tested | Justified by risk assessment; change not considered impactful. |
| Robustness (System Suitability) | Meets all criteria | Pass | Pass | Pass |
The Integrated Workflow: From Change Management to Continuous Verification
The synergy between ICH Q12 and Continuous Verification creates a cohesive, data-driven lifecycle for a product and its analytical methods. The following diagram visualizes this integrated workflow, highlighting the role of partial validation.
Integrated Lifecycle Workflow
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of this integrated approach relies on specific tools and reagents that ensure data integrity and robustness.
Table 3: Essential Research Reagent Solutions for Lifecycle Management
| Item / Solution | Function / Rationale |
|---|---|
| Stable Reference Standards | High-purity, well-characterized drug substance for accurate method validation and system suitability testing, ensuring data reliability throughout the method's lifecycle [50]. |
| System Suitability Test Kits | Pre-mixed solutions containing analytes and critical impurities to verify chromatographic system performance before validation or routine use, a cornerstone of robust analytical procedures [83]. |
| Process Analytical Technology (PAT) Probes | In-line sensors (e.g., NIR, Raman) for real-time monitoring of Critical Quality Attributes (CQAs), enabling Continuous Process Verification and providing the data foundation for science-based change management [80]. |
| Platform Analytical Procedures & Materials | Use of standardized, well-understood analytical techniques (e.g., standard HPLC conditions) and associated reagents. This allows for reduced validation testing when the platform is applied to a new product, as justified by prior knowledge [84] [83]. |
| Impurity and Excipient Standards | Isolated or synthesized compounds used to challenge method specificity during development and validation, and to establish the working range for impurity control [50] [62]. |
The objective comparison presented in this guide demonstrates that the integration of ICH Q12's regulatory framework with Continuous Verification principles offers a superior paradigm for managing analytical methods. The traditional, static approach is eclipsed by a dynamic, knowledge-driven lifecycle model. The experimental data and protocols show that this model enhances agility, as seen through efficient partial validation, and strengthens product quality assurance via real-time monitoring. For drug development professionals, adopting this integrated approach, supported by the appropriate reagent solutions and a robust Quality System, is no longer a future aspiration but a present-day imperative for achieving regulatory flexibility and maintaining a competitive edge.
In the pharmaceutical industry, analytical methods are foundational to ensuring drug product quality, safety, and efficacy. These methods, however, are often developed for immediate project needs without sufficient consideration for their entire lifecycle. The traditional approach to analytical method validation, guided by ICH Q2(R1), has historically focused on verifying a fixed set of performance characteristics at a single point in time [85]. This static model presents significant challenges when methods inevitably require modification due to changes in manufacturing processes, equipment, or regulatory standards [75]. Each change can trigger a comprehensive re-validation, consuming substantial time and resources.
The concept of "future-proofing" analytical methods represents a paradigm shift toward designing robust procedures with their entire lifecycle in mind. This approach strategically incorporates principles of Quality by Design (QbD) and risk management during the development phase to create methods that are more adaptable to change [75]. The recent adoption of new guidelines ICH Q2(R2) and ICH Q14 formalizes this lifecycle approach, providing a modernized framework for analytical procedure development and validation [75] [85]. By building methods with future modifications in consideration, scientists can significantly reduce the scope and complexity of subsequent partial validations, enabling faster implementation of improvements while maintaining regulatory compliance. This article explores practical strategies for designing future-proofed methods, supported by experimental data and structured protocols.
Regulatory Evolution: From Q2(R1) to a Lifecycle Approach
The regulatory landscape for analytical method validation is undergoing its most significant transformation in decades. The original ICH Q2(R1) guideline provided a standardized set of validation parameters but was primarily focused on chromatographic methods and offered limited guidance for handling method changes [85]. The new ICH Q2(R2) and ICH Q14 guidelines, which became effective in June 2024, establish a more comprehensive lifecycle management system for analytical procedures [85].
Key enhancements in the modernized framework include:
- Phase-appropriate validation, explicitly recognizing that validation requirements differ between clinical development phases and commercial production [85].
- Formalized use of development knowledge to establish method robustness, allowing development data to support later changes rather than requiring entirely new studies [85].
- Clarification of the "Response Function" (replacing the potentially confusing term "Linearity"), which provides better guidance for both linear and non-linear calibration models common in modern instrumentation [85].
- Explicit permission for a combined assessment of accuracy and precision, which can reduce validation study size and complexity when scientifically justified [85].
This evolved regulatory framework enables a more scientific approach to partial validation. By thoroughly understanding method capabilities and limitations during development, scientists can precisely define which parameters require re-testing when modifications occur, rather than defaulting to broad re-validation studies.
Table 1: Evolution of Key Validation Concepts from ICH Q2(R1) to Q2(R2)
| Validation Concept | ICH Q2(R1) Approach | ICH Q2(R2) Modernization | Impact on Partial Validation |
|---|---|---|---|
| Scope | Primarily chromatographic methods | Explicitly includes multivariate and bio-technological methods | Broader applicability for modern techniques |
| Linearity/Response | Focus on linear relationships only | Recognizes non-linear & multivariate calibration models | More appropriate testing for modified methods |
| Development Data | Not formally incorporated | Can be used to support validation | Reduces re-validation burden for changes |
| Range Definition | Based on experimental data | Allows extrapolation with justification | More flexibility when adjusting method range |
| Specificity/SELECTIVITY | Typically requires experimental studies | Permits technology-inherent justification for some techniques | Reduces testing needs for well-understood techniques |
Strategic Foundations for Future-Proofed Method Design
The Analytical Quality by Design (AQbD) Framework
Implementing Analytical Quality by Design (AQbD) principles from the outset is the most effective strategy for creating methods amenable to simpler partial validations. While not explicitly mandated in the new guidelines, the AQbD approach aligns perfectly with the enhanced knowledge management expectations of ICH Q14 [75]. This begins with defining an Analytical Target Profile (ATP) – a prospective summary of the method's required performance characteristics that defines what the method needs to achieve throughout its lifecycle [85].
The core process involves:
- Systematic Risk Assessment: Using tools like Fishbone diagrams and Failure Mode Effects Analysis (FMEA) to identify critical method parameters that most impact method performance [75].
- Design of Experiments (DoE): Employing statistical models to map the method's design space – the combination of input variables proven to provide suitable quality [75].
- Control Strategy: Establishing procedures to ensure the method remains within the design space during routine operation [75].
When a method developed using AQbD requires modification, the existing knowledge of the design space allows for targeted assessment of the change's impact. Instead of re-validating all parameters, scientists can focus only on those parameters potentially affected by the modification, substantially reducing the partial validation scope.
Method Modernization Case Study: HPLC to UHPLC Conversion
A compelling example of strategic method redesign that inherently incorporates future-proofing principles is the modernization of a pharmacopeia method for ketoprofen organic impurities from traditional HPLC to UHPLC technology [86]. This case demonstrates how adopting more advanced platform technologies can create methods with built-in resilience to future changes.
Table 2: Quantitative Performance and Efficiency Gains in Method Modernization [86]
| Parameter | Original HPLC Method | Modernized UHPLC Method | Improvement |
|---|---|---|---|
| Column Dimensions | 4.6 × 250 mm, 5-μm | 2.1 × 100 mm, 2.5-μm | Reduced column volume & particle size |
| Flow Rate | 1.0 mL/min | 0.417 mL/min | 58% reduction in solvent consumption |
| Injection Volume | 20 μL | 2.8 μL | 86% reduction in sample requirement |
| Analysis Time per Injection | 40.2 minutes | 14.3 minutes | 65% reduction in cycle time |
| Solvent Usage per Batch | ~723 mL | ~107 mL | 85% reduction in solvent waste & cost |
| Total Batch Analysis Time | ~723 min (~12 hours) | ~257 min (~4.5 hours) | 65% faster batch release |
The experimental protocol for this modernization followed USP <621> guidelines, which permit adjustments to column dimensions and particle size within specified limits (L/dp ratio of -25% to +50% of original conditions) [86]. The modernized method used a 2.1 × 100 mm, 2.5-μm column with an L/dp of 40,000, falling within the permitted range [86]. System suitability was maintained across both methods, demonstrating that modernization doesn't require compromising analytical performance [86].
This approach future-proofs the method by creating a more efficient separation that is less susceptible to issues like secondary interactions with hardware, thereby reducing potential out-of-specification results [86]. The significantly reduced analysis time and solvent consumption also make the method more sustainable and cost-effective for long-term use.
Practical Implementation: Designing for Simplified Partial Validations
The Method Lifecycle Workflow
The following diagram illustrates the integrated workflow for developing and maintaining future-proofed analytical methods throughout their lifecycle:
Figure 1: Analytical Method Lifecycle Workflow - This diagram illustrates the integrated approach to developing and maintaining future-proofed methods, highlighting how knowledge from initial development facilitates targeted partial validation when changes occur.
Protocol for Strategic Method Development
Implementing a robust method development protocol establishes the foundational knowledge required for streamlined future partial validations. The following structured approach ensures comprehensive method understanding:
Define Analytical Target Profile (ATP)
Conduct Systematic Risk Assessment
- Identify all potential method parameters that could impact results (e.g., mobile phase composition, column temperature, gradient profile, sample preparation variables).
- Prioritize parameters based on their potential impact on method performance using risk assessment tools.
Execute Design of Experiments (DoE)
- Design experiments to systematically evaluate the impact of critical parameters identified in the risk assessment.
- Model the interaction effects between parameters to establish a multidimensional design space.
- Identify robust method conditions where performance remains acceptable despite minor variations.
Establish Control Strategy
- Define system suitability criteria that ensure the method remains within the design space during routine use.
- Document all controlled parameters and their acceptable ranges.
- Establish appropriate replication strategies based on understanding of method variance components [85].
This development approach generates extensive knowledge about method behavior under various conditions. This knowledge base becomes invaluable when assessing the impact of future changes, as it provides scientific justification for limiting the scope of partial validation studies.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Future-Proof Method Development
| Material/Technology | Function in Development/Validation | Future-Proofing Advantage |
|---|---|---|
| Hybrid C18 Columns with Surface-Modified Hardware | Stationary phase for chromatographic separation | Mitigates analyte adsorption & secondary interactions, reducing variability [86] |
| Reference Standards | Method calibration and performance verification | Well-characterized standards ensure long-term method reproducibility |
| Forced Degradation Samples | Establishing method specificity and stability-indicating properties | Demonstrates method resilience to product changes over lifecycle |
| Quality Control Samples | Monitoring method performance during validation and transfer | Provides benchmark for comparing method performance pre- and post-modification |
| Automated Method Scaler Software | Calculating equivalent conditions when changing column dimensions or particle size | Facilitates method modernization while maintaining separation performance [86] |
Future-proofing analytical methods through strategic design represents both a scientific imperative and a significant efficiency opportunity for pharmaceutical development. The evolving regulatory framework of ICH Q2(R2) and Q14 formally recognizes the importance of a knowledge-driven, lifecycle approach to analytical procedures [75] [85]. As demonstrated by the UHPLC modernization case study, methods developed with built-in adaptability not only reduce future validation burdens but also deliver substantial operational benefits through reduced analysis times, lower solvent consumption, and decreased operational costs [86].
The fundamental principle is straightforward: investing in thorough, science-based method development using AQbD principles creates methods that are more robust, more understandable, and consequently, more adaptable to change. When method modifications become necessary – whether due to technology advancements, process changes, or regulatory updates – this foundational knowledge enables targeted, efficient partial validation. For researchers and drug development professionals, adopting this future-proofing mindset is no longer optional but essential for maintaining efficient, compliant analytical operations in an evolving technological and regulatory landscape.
Conclusion
Partial validation is not a one-size-fits-all activity but a flexible, science-driven process integral to the analytical method lifecycle. A successful strategy hinges on a risk-based assessment of the change's impact, guiding the scope of necessary experiments from a single accuracy and precision run to a nearly full validation. As the industry moves towards more complex modalities and continuous manufacturing, the principles of partial validation—clarity, documentation, and a thorough understanding of method robustness—will become even more critical. Embracing a proactive, lifecycle management approach, as outlined in emerging ICH Q2(R2) and Q14 guidelines, ensures methods remain fit-for-purpose, compliant, and capable of supporting the development of safe and effective therapies.
References
- 1. Method Transfer, Partial Validation, and Cross Validation: Recommendations for Best Practices and Harmonization from the Global Bioanalysis Consortium Harmonization Team - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4389741/]
- 2. Bioanalytical method validation: An updated review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3658022/]
- 3. Frequently Asked Questions about Method Validation | Ofni Systems [https://www.ofnisystems.com/services/method-validation/frequently-asked-questions-about-method-validation/]
- 4. Experimental design approach, screening and optimization of system variables, analytical method development of flurbiprofen in nanoparticles and stability-indicating methods for high-pressure liquid chromatography | Future Journal of Pharmaceutical Sciences | Full Text [https://fjps.springeropen.com/articles/10.1186/s43094-022-00426-4]
- 5. Review: Role of Model-Informed Drug Approaches in... Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC9097888/]
- 6. Deploying continuous improvement across the drug discovery value chain - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1359644611000961]
- 7. Foundations of AI Models in Drug Discovery Series: Step 6 of 6 - Continuous Improvement and Optimization in Drug Discovery | BioDawn Innovations [https://biodawninnovations.com/foundations-of-ai-in-drug-discovery-series-step-6-of-6-continuous-improvement-and-optimization-in-drug-discovery]
- 8. Understanding the Pharmaceutical Drug ... | TechTarget Development [https://www.techtarget.com/pharmalifesciences/news/366606452/Understanding-the-Pharmaceutical-Drug-Development-Life-Cycle]
- 9. Opportunities to Improve and Accelerate the Drug Development Pipeline - Improving and Accelerating Therapeutic Development for Nervous System Disorders - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK195041/]
- 10. Journal of Medical Internet Research - Methods for Analytical ... [https://www.jmir.org/2025/1/e70314]
- 11. Validation of analytical procedures: a comparison of... [https://www.pharmatutor.org/articles/validation-of-analytical-process-comparision-of-ich-pharmacopoeia-fda]
- 12. Q2(R2) Validation of Analytical Procedures | FDA [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/q2r2-validation-analytical-procedures]
- 13. ICH Guidance Q14 / Q2(R2) - Analytical Method Development/Method Validation Published for Consultation - ECA Academy [https://www.gmp-compliance.org/gmp-news/ich-guidance-q14-q2r2-analytical-method-development-method-validation-published-for-consultation]
- 14. Highlights from FDA's Analytical Test Method Validation Guidance [https://www.propharmagroup.com/thought-leadership/fda-analytical-test-method-validation-guidance]
- 15. Quality and Regulatory Predictability: Shaping USP Standards... | FDA [https://www.fda.gov/drugs/news-events-human-drugs/quality-and-regulatory-predictability-shaping-usp-standards-12112025]
- 16. E24-16: Analytical Method Validation and Lifecyle Management – FDA, ICH and USP Expectations - Eastern Analytical Symposium [https://eas.org/e23-analytical-method-validation-and-lifecyle-management-fda-ich-and-usp-expectations/]
- 17. USFDA Validation Differences | PPTX ICH [https://www.slideshare.net/slideshow/ich-usfda-validation-differences/64258452]
- 18. Aspects of validation in HPLC method development for pharmaceutical... [https://ijpsr.com/bft-article/aspects-of-validation-in-hplc-method-development-for-pharmaceutical-analysis-comparison-of-validation-requirements-by-fda-usp-and-ich/?view=fulltext]
- 19. An overview of pharmaceutical process validation and process control... [https://ijpsr.com/bft-article/an-overview-of-pharmaceutical-process-validation-and-process-control-variables-of-tablets-manufacturing-processes-in-industry/?view=fulltext]
- 20. Overview of Medical Device Process Validation : IQ, OQ, and PQ... [https://www.orielstat.com/blog/medical-device-process-validation/]
- 21. & Compliance: Using Validation ... | BioPharm International Risk [https://www.biopharminternational.com/view/validation-compliance-using-risk-analysis-process-validation]
- 22. Techniques For Risk - Based Using ASTM E2500 Validation [https://www.pharmaceuticalonline.com/doc/techniques-for-risk-based-validation-using-astm-e-0001]
- 23. Quality Risk Management In Computer System Validation (CSV) [https://gmpinsiders.com/quality-risk-management-in-computer-system-validation/]
- 24. Acceptance Criteria: Purposes, Types, Examples and Best Prac [https://www.altexsoft.com/blog/acceptance-criteria-purposes-formats-and-best-practices/]
- 25. Acceptance Criteria: Everything You Need to Know Plus Examples [https://resources.scrumalliance.org/Article/need-know-acceptance-criteria]
- 26. What is acceptance criteria? | Definition and Best Practices [https://www.productplan.com/glossary/acceptance-criteria/]
- 27. predictability: Refocusing through the lens of site... | ICON plc Protocol [https://www.iconplc.com/insights/blog/2025/05/15/protocol-predictability-refocusing-through-lens-site-and-patient]
- 28. Solution Selection in Six Sigma for Process Improvement... Matrix [https://www.6sigma.us/process-improvement/solution-selection-matrix/]
- 29. Validation of Stability-Indicating HPLC Methods for Pharmaceuticals: Overview, Methodologies, and Case Studies | LCGC International [https://www.chromatographyonline.com/view/validation-of-stability-indicating-hplc-methods-for-pharmaceuticals-overview-methodologies-and-case-studies]
- 30. Strategies in Reversed- Mobile Phase Optimization Phase HPLC [https://www.chromatographyonline.com/view/mobile-phase-optimization-strategies-reversed-phase-hplc]
- 31. / Optimizing Systems – General Recommendations HPLC UHPLC [https://www.ssi.shimadzu.com/service-support/faq/liquid-chromatography/knowledge-base/optimizing-your-hplc-uhplc-system/index.html]
- 32. HPLC Content Determination Method Validation: A Comprehensive Guide – Welch Materials, Inc. [https://www.welch-us.com/blogs/knowleage-base/hplc-content-determination-method-validation-a-comprehensive-guide]
- 33. Development Steps | Thermo Fisher Scientific - US HPLC Method [https://www.thermofisher.com/us/en/home/industrial/chromatography/chromatography-learning-center/liquid-chromatography-information/hplc-method-development-steps.html]
- 34. Product Focus: Sample for Preparation / HPLC | Lab Manager UHPLC [https://www.labmanager.com/product-focus-sample-preparation-for-hplc-uhplc-8288]
- 35. Modern Filtration Methods for HPLC and UHPLC Sample Preparation [https://www.chromatographyonline.com/view/modern-filtration-methods-hplc-and-uhplc-sample-preparation-0]
- 36. Tips & Tricks – HPLC Preparation Mobile Phase [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/analytical-chemistry/large-molecule-hplc/hplc-tips-tricks-mobile-phase-preparation]
- 37. A Three-Pronged Template Approach for Rapid HPLC Method Development | LCGC International [https://www.chromatographyonline.com/view/three-pronged-template-approach-rapid-hplc-method-development-0]
- 38. Ligand binding assay - Wikipedia [https://en.wikipedia.org/wiki/Ligand_binding_assay]
- 39. Ligand Binding Assays in the 21st Century Laboratory: Recommendations for Characterization and Supply of Critical Reagents - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326169/]
- 40. control strategy for biologics. Analytical I: Foundations Part [https://pubmed.ncbi.nlm.nih.gov/40354897/]
- 41. sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology... [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/ligand-binding-assay]
- 42. A straightforward method for measuring binding affinities of ligands to... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc02460a]
- 43. Determination of Protein- Ligand Affinities by Thermal Shift... Binding [https://pubmed.ncbi.nlm.nih.gov/39430314/]
- 44. 2025 Trends in Biotech and Life Sciences Research | Blog | ZAGENO [https://go.zageno.com/blog/2025-trends-in-biotech-and-life-sciences-research]
- 45. Binding Assays | BMG LABTECH [https://www.bmglabtech.com/en/blog/binding-assays-more-than-one-way-to-achieve-your-goals/]
- 46. Five Key Trends Shaping Biopharma and Biotech in 2025 | PPD [https://www.ppd.com/blog/2025-biopharma-biotech-trends/]
- 47. Process Validation Sample Protocol | Pharmaguideline [https://www.pharmaguideline.com/2013/11/process-validation-sample-protocol.html]
- 48. Analytical Method Validation: Back to Basics, Part II | LCGC International [https://www.chromatographyonline.com/view/analytical-method-validation-back-basics-part-ii]
- 49. Process Performance Qualification Runs - BioProcess International [https://www.bioprocessintl.com/cell-line-development/process-validation-calculating-the-necessary-number-of-process-performance-qualification-runs]
- 50. Validation of Analytical Methods | IntechOpen [https://www.intechopen.com/chapters/57909]
- 51. STAT-12: Verification/Validation Sampling Plans for Proportion Nonconforming - Taylor Enterprises [https://variation.com/stat-12-verification-validation-sampling-plans-for-proportion-nonconforming/]
- 52. What is RCFA or Root cause failure analysis [https://idcon.com/resource-library/root-cause/whats-root-cause/]
- 53. What are the three levels of root ? cause failure analysis [https://avestaconsulting.net/industry/three-levels-root-cause-failure-analysis/]
- 54. : Process, Techniques, and Best Practices... Root Cause Analysis [https://thebusinessanalystjobdescription.com/root-cause-analysis-steps-techniques-and-best-practices/]
- 55. 16 Best Root Tools and Templates [ Cause ...] - RankRed Analysis 2025 [https://www.rankred.com/root-cause-analysis-tools-templates/]
- 56. Method validation and measurement uncertainty estimation of pesticide residues in Okra by GC/HPLC - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425206/]
- 57. : Problems continue - ECA Academy Root Cause Analysis [https://www.gmp-compliance.org/gmp-news/root-cause-analysis-problems-continue]
- 58. Ligand binding assays - Bioanalysis Zone [https://www.bioanalysis-zone.com/spotlights/ligand-binding-assays/]
- 59. Optimizing Ligand Binding Assay Conditions for Accurate and Reproducible Results | Sword Bio [https://swordbio.com/blog/optimizing-ligand-binding-assay-conditions-for-accurate-and-reproducible-results/]
- 60. Quality Controls in Ligand Binding Assays: Recommendations and Best Practices for Preparation, Qualification, Maintenance of Lot to Lot Consistency, and Prevention of Assay Drift - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6647453/]
- 61. Highly sensitive ligand - binding in pre-clinical and clinical... assays [https://pubs.rsc.org/en/content/articlehtml/2015/an/c5an00822k]
- 62. An outline of quality guidelines for developing and validating ... [https://ijpsr.com/bft-article/an-outline-of-quality-guidelines-for-developing-and-validating-analytical-procedures/?view=fulltext]
- 63. 2022 White Paper on Recent Issues in Bioanalysis: Enzyme Assay... [https://pubmed.ncbi.nlm.nih.gov/37584363/]
- 64. Interpretation and Visualization of Non-Linear Data Fusion... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0038163]
- 65. 2.1 Similarity for qua... | PRIMER-e Learning Hub [https://learninghub.primer-e.com/books/change-in-marine-communities/page/21-similarity-for-quantitative-data-matrices]
- 66. Validation Terminology | Ofni Systems [https://www.ofnisystems.com/services/validation/validation-terminology/]
- 67. Analytical Method in Pharmaceuticals | Pharmaguideline Transfer [https://www.pharmaguideline.com/2025/09/analytical-method-transfer-in-pharmaceuticals.html]
- 68. Analytical Method (USP 1224) Guideline - Pharma Beginners Transfer [https://pharmabeginers.com/analytical-method-transfer-usp1224-guideline/]
- 69. Analytical method (module 01) | PPTX transfer [https://www.slideshare.net/slideshow/analytical-method-transfer-module-01/48996157]
- 70. Difference Between Validation And Verification Of Analytical Methods [https://gmpinsiders.com/method-validation-vs-verification/]
- 71. The Comparison of Methods Experiment - Westgard QC [https://westgard.com/lessons/basic-method-validation/lesson23.html]
- 72. Using Validation Dataset and Cross - validation Techniques [https://www.deepchecks.com/evaluating-model-performance-using-validation-dataset-splits-and-cross-validation-techniques/]
- 73. - Cross (statistics) - Wikipedia validation [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 74. 3.1. Cross - validation : evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 75. Trends In Pharmaceutical 2025 ... Analytical Methods Development [https://agnopharma.com/blog/trends-in-pharmaceutical-analytical-methods-development-validation/]
- 76. : step-by-step guide & best practices Analytical Method Transfer [https://www.qbdgroup.com/en/blog/analytical-method-transfer-steps]
- 77. Across Global Sites Streamlining Method Transfer [https://www.pharmtech.com/view/streamlining-method-transfer-across-global-sites]
- 78. : Enhancing PACM Agility ICH Q 12 Implementation [https://www.linkedin.com/pulse/ich-q12-implementation-enhancing-pacm-agility-valgenesis-inc-qtwif]
- 79. Technical and regulatory considerations for pharmaceutical... ICH Q 12 [https://www.ema.europa.eu/en/ich-q12-technical-regulatory-considerations-pharmaceutical-product-lifecycle-management-scientific-guideline]
- 80. Process Analytical Technology Tools for Monitoring Pharmaceutical Unit Operations: A Control Strategy for Continuous Process Verification - PubMed [https://pubmed.ncbi.nlm.nih.gov/34205797/]
- 81. Bringing Regulatory Flexibility To Post-Approval Changes ICH Q 12 [https://www.pharmaceuticalonline.com/doc/ich-q-bringing-regulatory-flexibility-to-post-approval-changes-0001]
- 82. ICH Q2(R2) & Q14 Aim to Promote More Robust Analytical Processes, Greater Ease for Switching Analytical Methods Post Approval | Pharmaceutical Engineering [https://ispe.org/pharmaceutical-engineering/ispeak/ich-q2r2-q14-aim-promote-more-robust-analytical-processes-greater]
- 83. ICH Guidelines for Analytical Method Validation Explained | AMSbiopharma [https://amsbiopharma.com/ich-guidelines-analytical-method/]
- 84. ICH Q2(R2) Validation of Analytical Procedures: An Overview of the Revised Guideline | QbD Group [https://www.qbdgroup.com/en/blog/ich-q2r2-validation-of-analytical-procedures-an-overview-of-the-revised-guideline/]
- 85. LOGFILE Feature | Validation of Analytical | Methods 1 Part [https://www.gmp-publishing.com/content/en/gmp-news/gmp-newsletter/gmp-logfile-lead-article/d/1692/gmp-feature-03-2025-regulatory-requirements-for-the-validation-of-analytical-methods-part-1]
- 86. Future-Proofing Validated Pharmacopeia Methods: A Case Study of Improving Throughput and Decreasing Operational Cost | LCGC International [https://www.chromatographyonline.com/view/future-proofing-validated-pharmacopeia-methods-improving-throughput-decreasing-operational-cost]
- 87. : are your Analytical ... | QbD Group Method Validation analytical [https://www.qbdgroup.com/en/blog/analytical-method-validation-are-your-methods-suitable-for-intended-use/]